Ann Clin Neurophysiol.
2024;26(2):57-62. 10.14253/acn.24003.
Detection of critical intratumoral hemorrhage during spine surgery by intraoperative neurophysiologic monitoring: a case report
- Affiliations
-
- 1Department of Neurology, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea
- 2Neuroscience Center, Samsung Medical Center, Seoul, Korea
- 3Department of Neurology, Jeju National University School of Medicine, Jeju, Korea
- KMID: 2560433
- DOI: http://doi.org/10.14253/acn.24003
Abstract
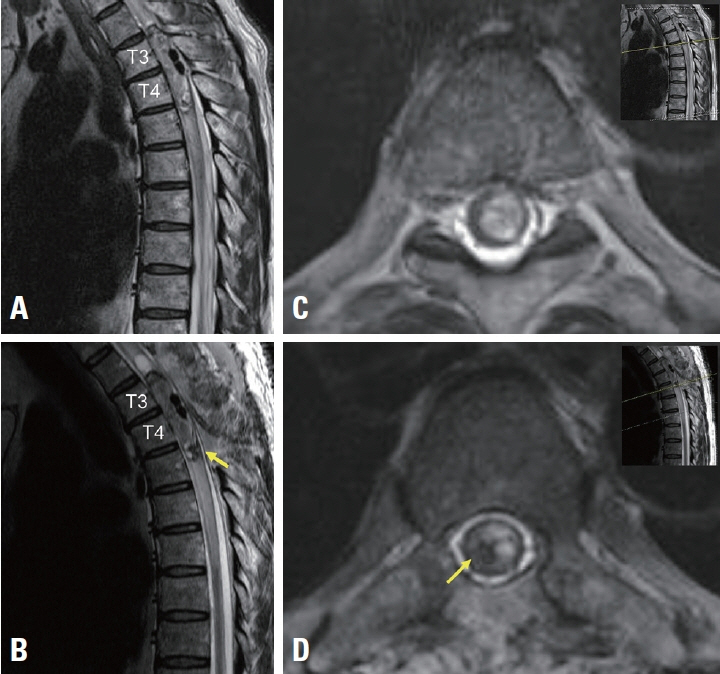
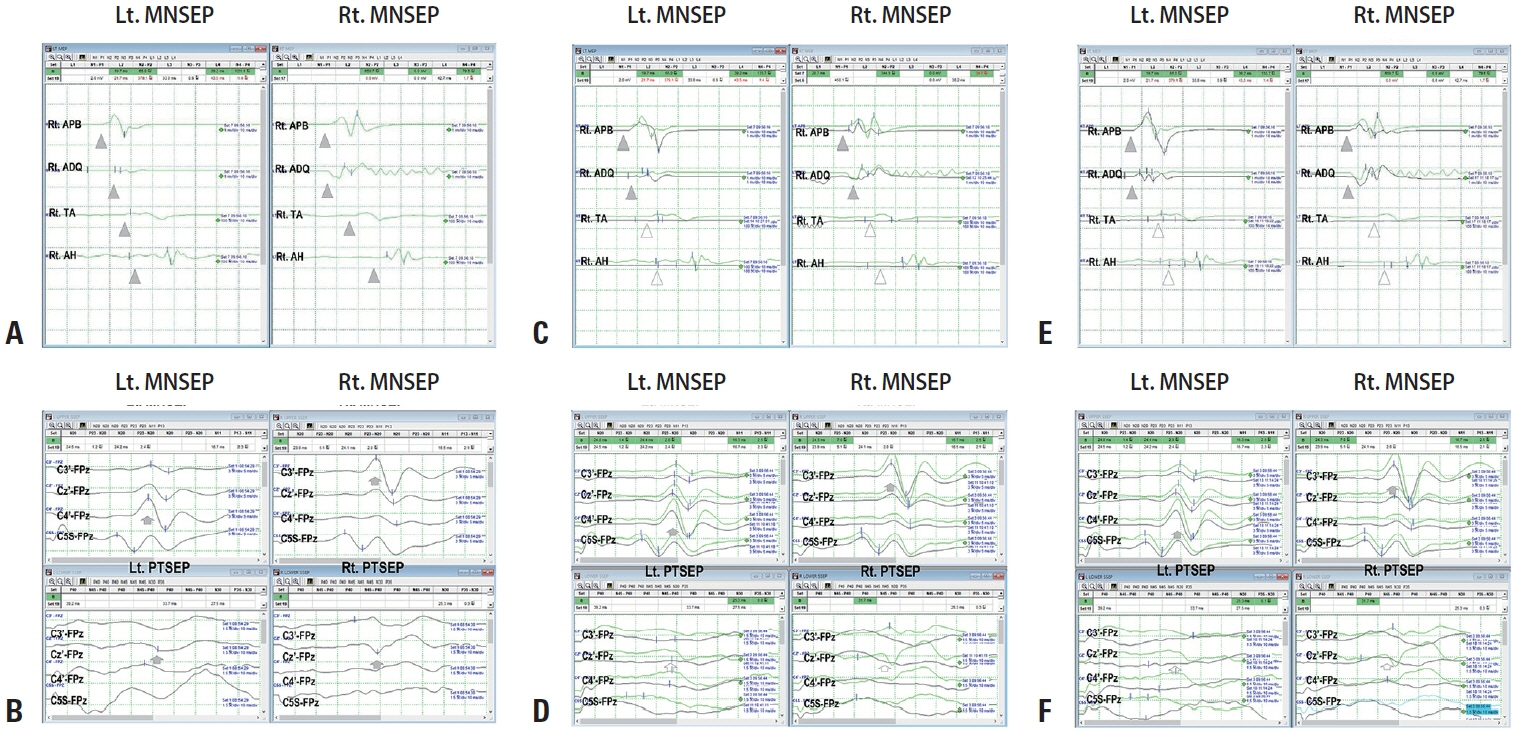
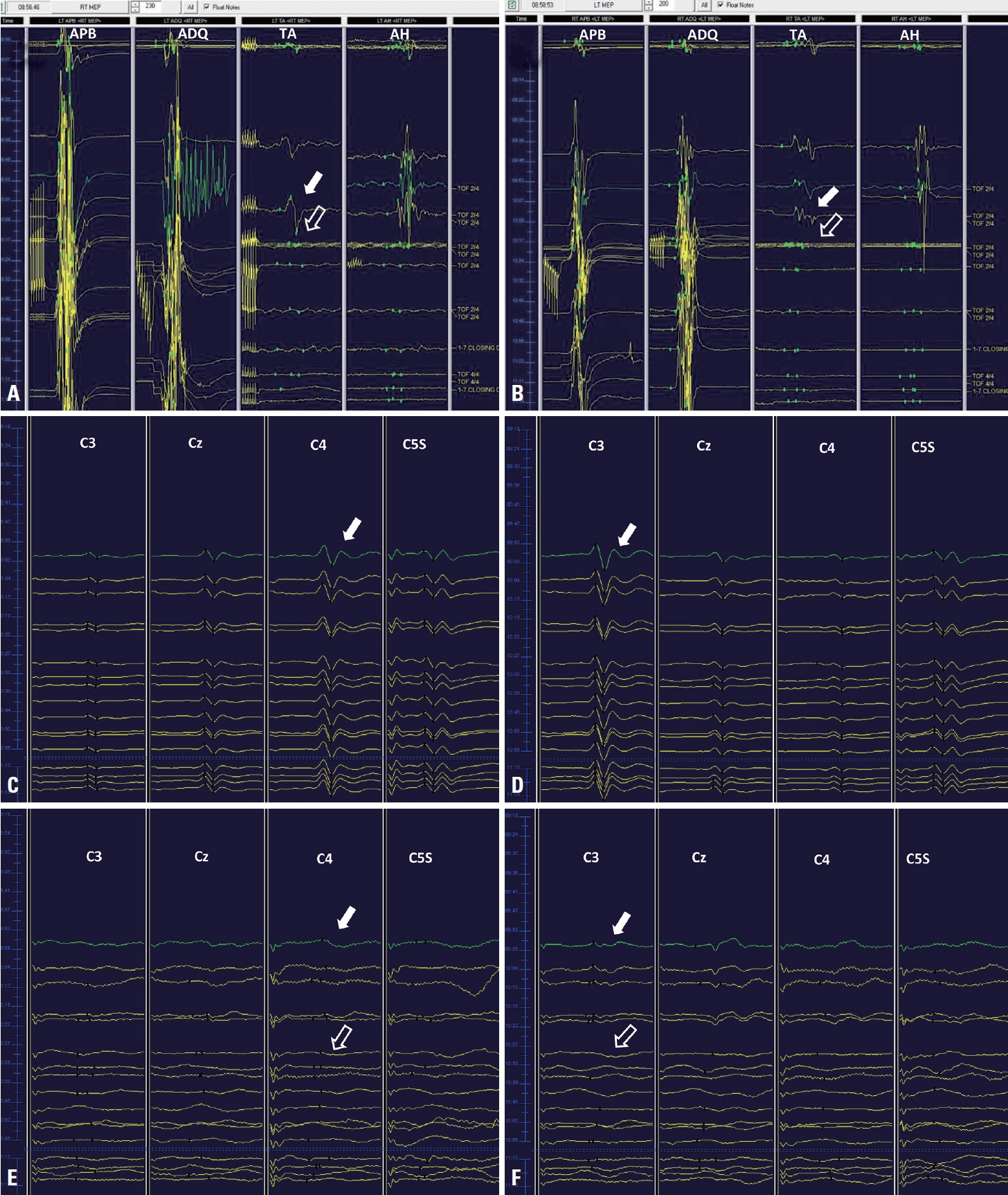
- Complete surgical resection is a well-known therapeutic gold standard for spinal ependymoma, but it is associated with high postoperative morbidity. Intraoperative neuromonitoring (INM) is important for detecting and reducing the rate of surgical complications during this operative procedure. We report a case of postoperative paraplegia due to tumor bleeding during the operation. INM of the patient revealed abrupt loss of waveforms during the operation. This finding suggested that INM is helpful for detecting intraoperative hematomyelia and minimizing postoperative neurologic sequelae.
Keyword
Figure
Reference
-
1. Aghakhani N, David P, Parker F, Lacroix C, Benoudiba F, Tadie M. Intramedullary spinal ependymomas: analysis of a consecutive series of 82 adult cases with particular attention to patients with no preoperative neurological deficit. Neurosurgery. 2008; 62:1279–1285. discussion 1285-1286.2. Klekamp J. Spinal ependymomas. Part 1: intramedullary ependymomas. Neurosurg Focus. 2015; 39:E6.
Article3. McCormick PC, Torres R, Post KD, Stein BM. Intramedullary ependymoma of the spinal cord. J Neurosurg. 1990; 72:523–532.
Article4. Wild F, Hartmann C, Heissler HE, Hong B, Krauss JK, Nakamura M. Surgical treatment of spinal ependymomas: experience in 49 patients. World Neurosurg. 2018; 111:e703–e709.
Article5. Kucia EJ, Bambakidis NC, Chang SW, Spetzler RF. Surgical technique and outcomes in the treatment of spinal cord ependymomas, part 1: intramedullary ependymomas. Neurosurgery. 2011; 68:57–63. discussion 63.
Article6. Charalampidis A, Jiang F, Wilson JRF, Badhiwala JH, Brodke DS, Fehlings MG. The use of intraoperative neurophysiological monitoring in spine surgery. Global Spine J. 2020; 10:104S–114S.
Article7. Harel R, Schleifer D, Appel S, Attia M, Cohen ZR, Knoller N. Spinal intradural extramedullary tumors: the value of intraoperative neurophysiologic monitoring on surgical outcome. Neurosurg Rev. 2017; 40:613–619.
Article8. Korn A, Halevi D, Lidar Z, Biron T, Ekstein P, Constantini S. Intraoperative neurophysiological monitoring during resection of intradural extramedullary spinal cord tumors: experience with 100 cases. Acta Neurochir (Wien). 2015; 157:819–830.
Article9. Fehlings MG, Brodke DS, Norvell DC, Dettori JR. The evidence for intraoperative neurophysiological monitoring in spine surgery: does it make a difference? Spine (Phila Pa 1976). 2010; 35:S37–S46.10. Sala F, Palandri G, Basso E, Lanteri P, Deletis V, Faccioli F, et al. Motor evoked potential monitoring improves outcome after surgery for intramedullary spinal cord tumors: a historical control study. Neurosurgery. 2006; 58:1129–1143. discussion 1129-1143.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Chondrosarcoma with Intratumoral Hemorrhage: Case Report
- Surveillance in the Cerebral Aneurysm Surgery
- Supratentorial Extraventricular Anaplastic Ependymoma Presenting with Repeated Intratumoral Hemorrhage
- Treatment of Nasopharyngeal Angiofibroma with Intraoperative Serial Intratumoral Embolization : 2 Cases
- Intraoperative Neurophysiologic Monitoring: Basic Principles and Recent Update