J Korean Neurosurg Soc.
2024 Nov;67(6):637-645. 10.3340/jkns.2023.0221.
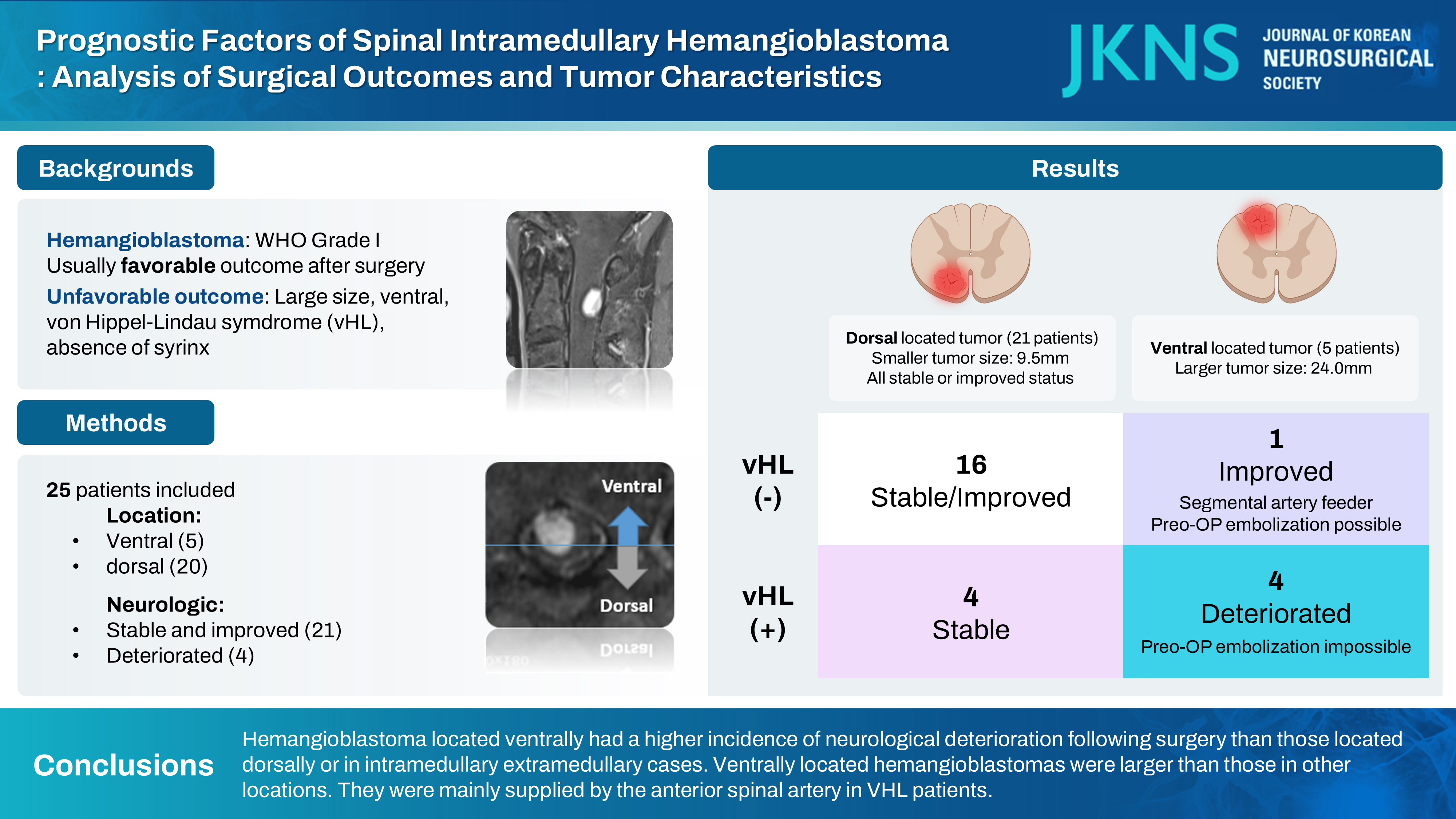
Prognostic Factors of Spinal Intramedullary Hemangioblastoma : Analysis of Surgical Outcomes and Tumor Characteristics
- Affiliations
-
- 1Department of Neurosurgery, Spine and Spinal Cord Institute, Gangnam Severance Hospital, Yonsei University College of Medicine, Seoul, Korea
- 2Department of Neurosurgery, Leon Wiltse Memorial Hospital, Suwon, Korea
- KMID: 2560405
- DOI: http://doi.org/10.3340/jkns.2023.0221
Abstract
Objective
: Spinal intramedullary hemangioblastoma is a rare and highly vascularized benign tumor. The characteristics of the tumor, its corresponding location, and surgical outcomes remain unknown. The purpose of this study was to identify risk factors and strategies for neurologic deterioration following hemangioblastoma surgery.
Methods
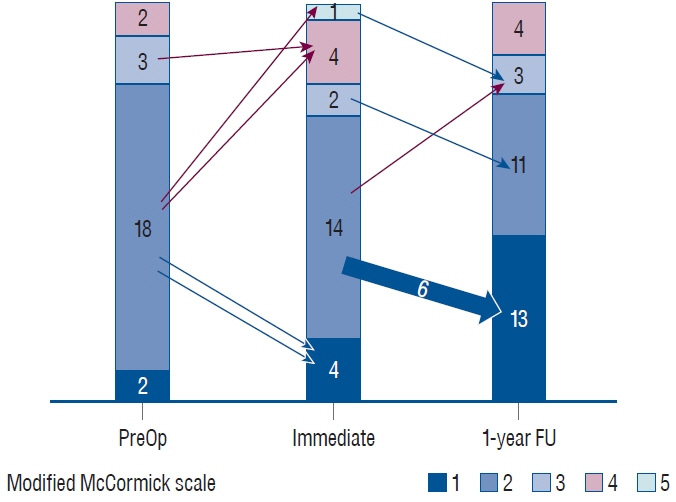
: A comprehensive retrospective analysis was undertaken to evaluate patients who underwent surgical intervention for intramedullary hemangioblastoma at our institution from 1993 to 2022. Patients with at least 1 year of follow-up data were included. The analysis covered patient demographics, pre- and post-operative modified McCormick scale (MMCS), tumor location, and tumor size.
Results
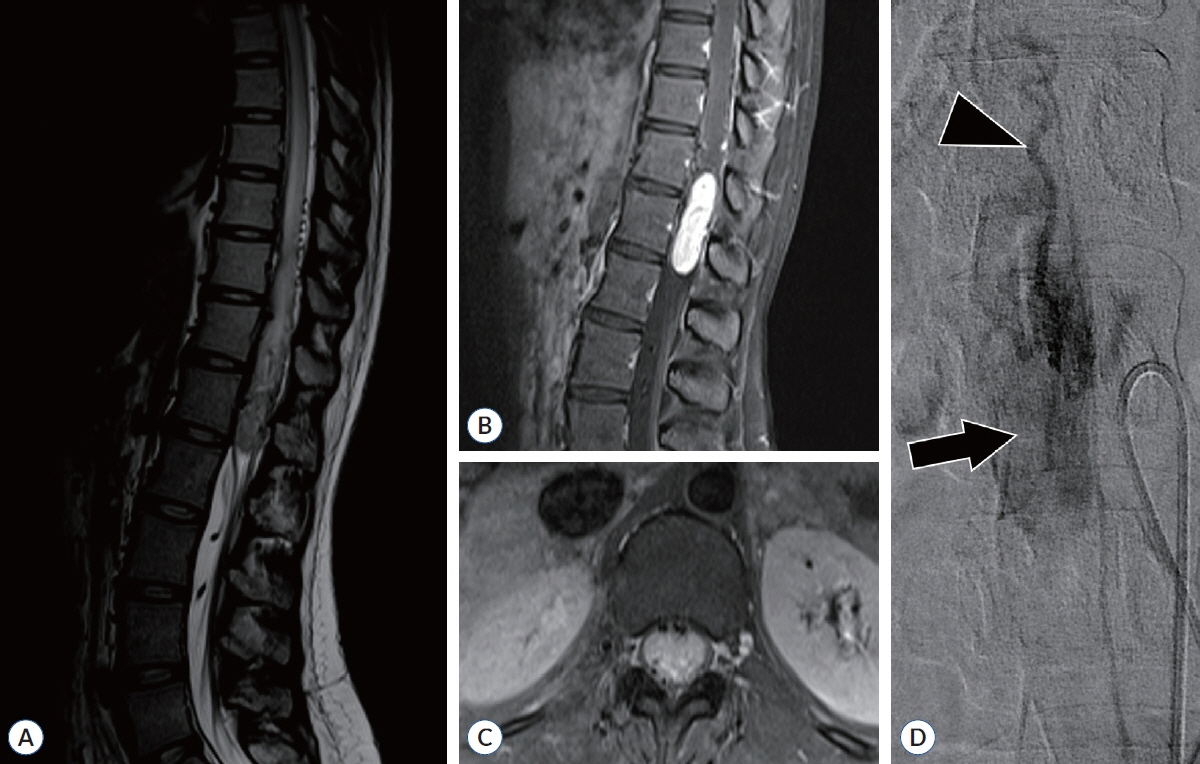
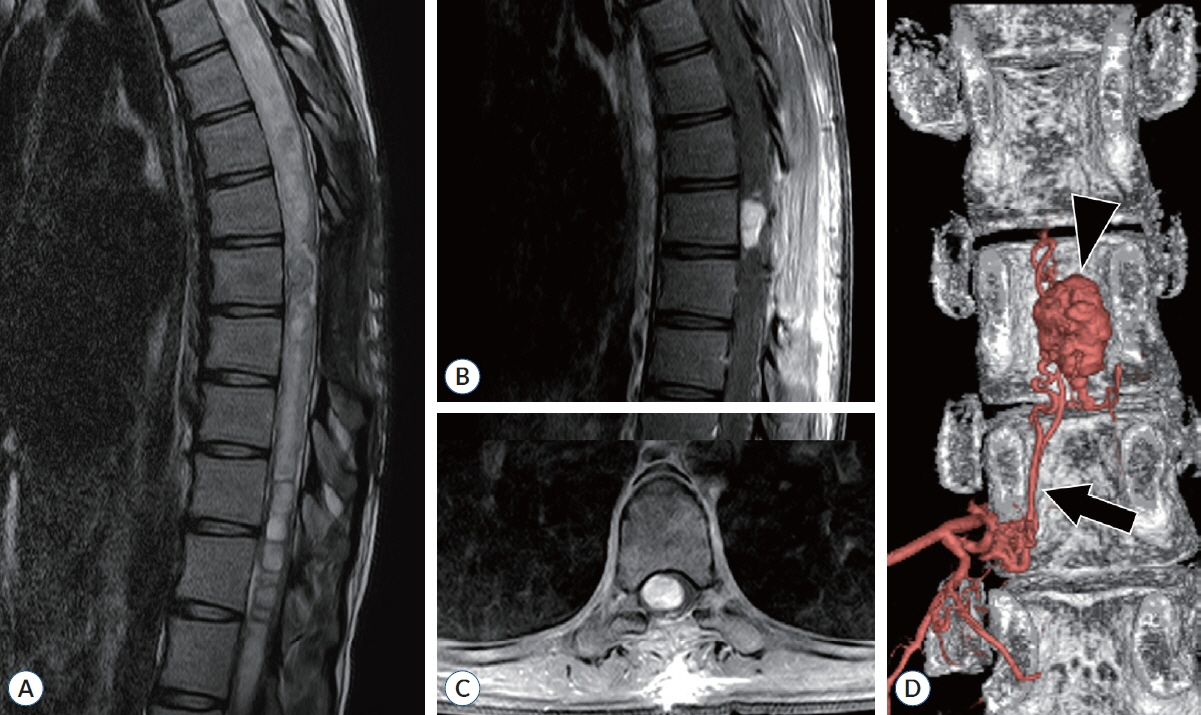
: This study included 25 cases. One-year after surgery, neurological deterioration was observed in five cases (20.0%), and neurological improvement was found in nine cases (36.0%). Five cases were ventrally located, and twelve cases were dorsally located. Ventrally located cases were larger in tumor axial size (p=0.029) than dorsal location tumors, resulting in poorer follow-up MMCS and a higher prevalence of von Hippel-Lindau syndrome (VHL) (p=0.042). Three of them were confirmed to be supplied by the anterior spinal artery. In the case of dorsally located cases, there was no neurologic deterioration.
Conclusion
: In intramedullary spinal cord hemangioblastomas, cases located ventrally had a higher incidence of neurological deterioration following surgery than those located dorsally or in intramedullary extramedullary cases. Ventrally located hemangioblastomas were larger than those in other locations. They were mainly supplied by the anterior spinal artery in VHL patients.
Figure
Cited by 1 articles
-
Editors’ Pick in November 2024
Bum-Tae Kim
J Korean Neurosurg Soc. 2024;67(6):593-594. doi: 10.3340/jkns.2024.0190.
Reference
-
References
1. Ampie L, Choy W, Khanna R, Smith ZA, Dahdaleh NS, Parsa AT, et al. Role of preoperative embolization for intradural spinal hemangioblastomas. J Clin Neurosci. 24:83–87. 2016.
Article2. Bellut D, Burkhardt JK, Mannion AF, Porchet F. Assessment of outcome in patients undergoing surgery for intradural spinal tumor using the multidimensional patient-rated core outcome measures index and the modified McCormick scale. Neurosurg Focus. 39:E2. 2015.
Article3. Boström A, Hans FJ, Reinacher PC, Krings T, Bürgel U, Gilsbach JM, et al. Intramedullary hemangioblastomas: timing of surgery, microsurgical technique and follow-up in 23 patients. Eur Spine J. 17:882–886. 2008.
Article4. Bridges KJ, Jaboin JJ, Kubicky CD, Than KD. Stereotactic radiosurgery versus surgical resection for spinal hemangioblastoma: a systematic review. Clin Neurol Neurosurg. 154:59–66. 2017.
Article5. Conway JE, Chou D, Clatterbuck RE, Brem H, Long DM, Rigamonti D. Hemangioblastomas of the central nervous system in von Hippel-Lindau syndrome and sporadic disease. Neurosurgery. 48:55–63. discussion 62-63. 2001.
Article6. Cristante L, Herrmann HD. Surgical management of intramedullary hemangioblastoma of the spinal cord. Acta Neurochir (Wien). 141:333–339. discussion 339-340. 1999.
Article7. Daly ME, Choi CY, Gibbs IC, Adler JR Jr, Chang SD, Lieberson RE, et al. Tolerance of the spinal cord to stereotactic radiosurgery: insights from hemangioblastomas. Int J Radiat Oncol Biol Phys. 80:213–220. 2011.
Article8. Foo D, Rossier AB. Anterior spinal artery syndrome and its natural history. Paraplegia. 21:1–10. 1983.
Article9. Han B, Zhang L, Jia W. Pediatric spinal hemangioblastomas: clinical features and surgical outcomes of 39 cases. Neurospine. 20:343–352. 2023.
Article10. Iwasaki Y, Koyanagi I, Hida K, Abe H. Anterior approach to intramedullary hemangioblastoma: case report. Neurosurgery. 44:655–657. 1999.
Article11. Joshi SS, Moghe VV, Choudhari KA. Spinal cord rotation by denticulate ligamental stay-sutures for anteriorly placed intradural lesions. J Spin Surg. 6:29. 2019.12. Kageyama H, Tatebayashi K, Yoshimura S, Endo T, Hida K, Mizuno M. Outcomes of intramedullary spinal cord tumor surgery in older versus younger adults: a multicenter subanalysis study by the Neurospinal Society of Japan. Neurospine. 20:678–691. 2023.
Article13. Lee J, Koyanagi I, Hida K, Seki T, Iwasaki Y, Mitsumori K. Spinal cord edema: unusual magnetic resonance imaging findings in cervical spondylosis. J Neurosurg. 99(1 Suppl):8–13. 2003.
Article14. Lonser RR, Glenn GM, Walther M, Chew EY, Libutti SK, Linehan WM, et al. von Hippel-Lindau disease. Lancet. 361:2059–2067. 2003.
Article15. Lonser RR, Weil RJ, Wanebo JE, Devroom HL, Oldfield EH. Surgical management of spinal cord hemangioblastomas in patients with von HippelLindau disease. J Neurosurg. 98:106–116. 2003.
Article16. Malis LI. Atraumatic bloodless removal of intramedullary hemangioblastomas of the spinal cord. J Neurosurg. 97(1 Suppl):1–6. 2002.
Article17. Manconi M, Mondini S, Fabiani A, Rossi P, Ambrosetto P, Cirignotta F. Anterior spinal artery syndrome complicated by the ondine curse. Arch Neurol. 60:1787–1790. 2003.
Article18. Mandigo CE, Ogden AT, Angevine PD, McCormick PC. Operative management of spinal hemangioblastoma. Neurosurgery. 65:1166–1177. 2009.
Article19. Mechtler LL, Nandigam K. Spinal cord tumors: new views and future directions. Neurol Clin. 31:241–268. 2013.20. Moss JM, Choi CY, Adler JR Jr, Soltys SG, Gibbs IC, Chang SD. Stereotactic radiosurgical treatment of cranial and spinal hemangioblastomas. Neurosurgery. 65:79–85. discussion 85. 2009.
Article21. Murota T, Symon L. Surgical management of hemangioblastoma of the spinal cord: a report of 18 cases. Neurosurgery. 25:699–707. discussion 708. 1989.
Article22. Neumann HP, Eggert HR, Scheremet R, Schumacher M, Mohadjer M, Wakhloo AK, et al. Central nervous system lesions in von Hippel-Lindau syndrome. J Neurol Neurosurg Psychiatry. 55:898–901. 1992.
Article23. Pluta RM, Iuliano B, DeVroom HL, Nguyen T, Oldfield EH. Comparison of anterior and posterior surgical approaches in the treatment of ventral spinal hemangioblastomas in patients with von Hippel-Lindau disease. J Neurosurg. 98:117–124. 2003.
Article24. Ryu SI, Kim DH, Chang SD. Stereotactic radiosurgery for hemangiomas and ependymomas of the spinal cord. Neurosurg Focus. 15:E10. 2003.
Article25. Sadashivam S, Abraham M, Kesavapisharady K, Nair SN. Long-term outcome and prognostic factors of intramedullary spinal hemangioblastomas. Neurosurg Rev. 43:169–175. 2020.
Article26. Takai K, Taniguchi M, Takahashi H, Usui M, Saito N. Comparative analysis of spinal hemangioblastomas in sporadic disease and Von Hippel-Lindau syndrome. Neurol Med Chir (Tokyo). 50:560–567. 2010.
Article27. Takeshima Y, Takami H, Endo T, Mizuno M, Hida K; Investigators of Intramedullary Spinal Cord Tumors in the Neurospinal Society of Japan. Comparison of the recurrence and surgical outcome of spinal hemangioblastoma in sporadic and von Hippel-Lindau diseases: a subanalysis of a nationwide study by the Neurospinal Society of Japan. Neurospine. 20:756–765. 2023.
Article28. Tampieri D, Leblanc R, TerBrugge K. Preoperative embolization of brain and spinal hemangioblastomas. Neurosurgery. 33:502–505. discussion 505. 1993.
Article29. Timonin SY, Konovalov NA. Surgical treatment of intramedullary hemangioblastomas: current state of problem (review). Sovrem Tekhnologii Med. 13:83–94. 2021.
Article30. Van Der Veken J, Gläsker S, Vougioukas V, Van Velthoven V. Posterior approach for anteriorly located cervical spinal cord hemangioblastomas: technical note. J Neurosurg Spine. 29:448–451. 2018.31. Visco ZR, Liu DD, Leary OP, Oyelese AA, Gokaslan ZL, Camara-Quintana JQ, et al. A transpedicular approach to complex ventrally situated thoracic intradural extramedullary tumors: technique, indications, and multiinstitutional case series. Neurosurg Focus. 50:E19. 2021.
Article32. Yasargil MG, Antic J, Laciga R, de Preux J, Fideler RW, Boone SC. The microsurgical removal of intramedullary spinal hemangioblastomas. Report of twelve cases and a review of the literature. Surg Neurol. (3):141–148. 1976.33. Zenner J, Koller H, Hempfing A, Hutter J, Hitzl W, Resch H, et al. Approach-related morbidity in transthoracic anterior spine surgery: a clinical study and review of literature. Coluna/Columna. 9:72–84. 2010.34. Zhang K, Li C, Hou K, Yu J. Role of the cervical anterior spinal artery in the endovascular treatment of vascular diseases: bystander, accomplice, victim, or friend? Front Neurol. 12:761006. 2021.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Intramedullary Spinal Hemangioblastoma Associated with Syringomyelia
- Relationship between Spinal Hemangioblastoma Location and Age
- Spinal Cord Enlargement Due to Intramedullary Hemangioblastoma: A Case Report
- A Case of Cervical Cord Hemangioblastoma
- Intramedullary Hemangioblastoma of Cervicomedullary Junction with Diffuse Spinal Cord Enlargement and Cyst Formation : A Case Report