Anat Cell Biol.
2024 Sep;57(3):378-383. 10.5115/acb.24.061.
Variability in the projection level of the vertebra prominens: a cadaveric study
- Affiliations
-
- 1Department of Anatomy and Surgical Anatomy, School of Medicine, Faculty of Health Sciences, Aristotle University of Thessaloniki, Thessaloniki, Greece
- 2Österreichische Arbeitsgemeinschaft für Manuelle Medizin, Graz, Austria
- 3Ordination Dr. Sammer, Raaba/Grambach, Austria
- 4Department of Anatomy, School of Medicine, Faculty of Health Sciences, National and Kapodistrian University of Athens, Athens, Greece
- 5Institute for Anatomy and Clinical Morphology, Witten/Herdecke University, Witten, Germany
- 6Institute of Clinical Morphology, Medical University of Graz, Graz, Austria
- KMID: 2559752
- DOI: http://doi.org/10.5115/acb.24.061
Abstract
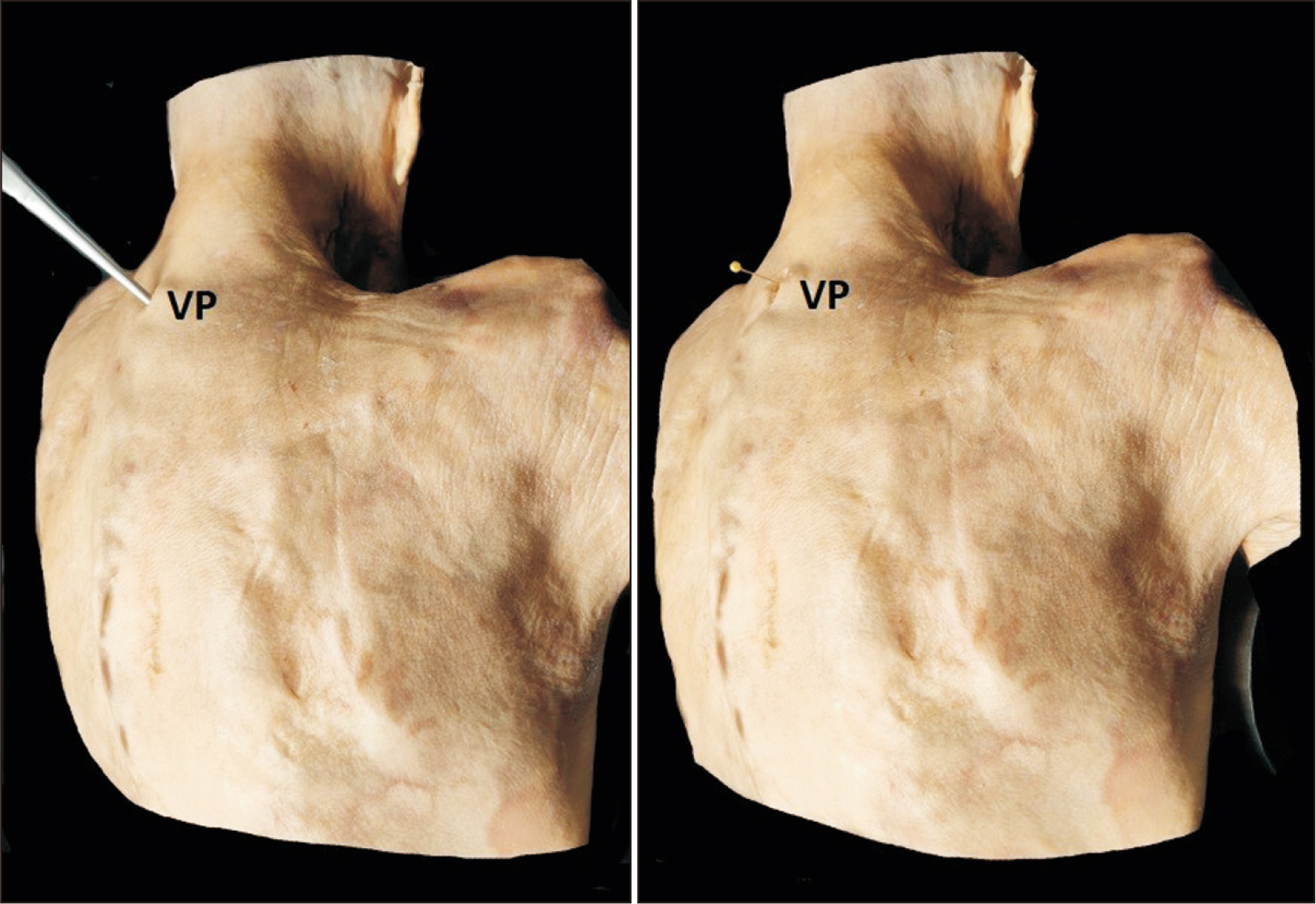
- The 7th cervical vertebra (C7) is described as having the most prominent spinous process (SP) and is characterized as the “vertebra prominens” (VP) of the cervical spine in anatomy textbooks. The VP is an important anatomical landmark of the neck for clinical examination and therapeutic intervention. The present study identifies the level of the most prominent SP of the cervical and uppermost thoracic vertebrae in a cadaveric cohort. Thirty-nine (23 female and 16 male) cadavers of a mean age of 77.5 years were investigated in a prone position and a certain cervical kyphotic bending. The most prominent SP, at the base of the neck, was palpated and marked with a wedging nail into the SP of the vertebra. The cervical region was dissected, and a blind investigator examined whether the nail was placed into the SP of C7 or the SP of another upper or lower vertebra. In 19 out of 39 cadavers (48.7%), the C7 was identified as the VP (typical anatomy), followed by the C6 (in 14 cadavers, 35.9%), C5 (in 4 cadavers, 10.3%). In 2 cadavers (5.1%) the first thoracic vertebra was identified as having the most prominent SP. Although C7 is described as the VP, in the present study the SP of C7 was the most prominent in less than 50%. The high variable projection level of the most prominent SP of the cervical vertebra holds great clinical significance for spine examination, neck surgery, and spinal anesthesia.
Figure
Reference
-
References
1. Standring S. Gray's Anatomy: the anatomical basis of clinical practice. 40th ed. Elsevier;2008.2. Stonelake PS, Burwell RG, Webb JK. 1988; Variation in vertebral levels of the vertebra prominens and sacral dimples in subjects with scoliosis. J Anat. 159:165–72. PMID: 3248964. PMCID: PMC1262019.3. Zhang L, Luo Z, Wang H, Ren L, Yu F, Guan T, Fu S. 2018; An anatomical study of the spinous process of the seventh cervical vertebrae based on the three-dimensional computed tomography reconstruction. Exp Ther Med. 16:511–6. DOI: 10.3892/etm.2018.6245. PMID: 30116309. PMCID: PMC6090245.4. Kothe R, Rüther W, Schneider E, Linke B. 2004; Biomechanical analysis of transpedicular screw fixation in the subaxial cervical spine. Spine (Phila Pa 1976). 29:1869–75. DOI: 10.1097/01.brs.0000137287.67388.0b. PMID: 15534407.5. Cramer GD, Darby SA. Clinical anatomy of the spine, spinal cord, and ANS. 3rd ed. Elsevier;2014.6. Günter U. 2019; Neural therapy for neck and tension headaches. Erfahrungsheilkunde. 68:140–7. German. DOI: 10.1055/a-0898-2256.7. Dehoust N. 2023; Symptomatic pathologic hypermobility in the differential diagnosis of chronic cervical spine complaints. Manual diagnostic techniques and treatment options using proliferation therapy. Man Med. 61:95–103. German. DOI: 10.1007/s00337-023-00962-x.8. Drerup B, Hierholzer E. 1985; Objective determination of anatomical landmarks on the body surface: measurement of the vertebra prominens from surface curvature. J Biomech. 18:467–74. DOI: 10.1016/0021-9290(85)90282-9. PMID: 4030803.9. Thiel W. 1992; An arterial substance for subsequent injection during the preservation of the whole corpse. Ann Anat. 174:197–200. German. DOI: 10.1016/S0940-9602(11)80347-X. PMID: 1503237.10. Thiel W. 2002; Supplement to the conservation of an entire cadaver according to W. Thiel. Ann Anat. 184:267–9. German. DOI: 10.1016/S0940-9602(02)80121-2. PMID: 12061344.11. Benkhadra M, Bouchot A, Gérard J, Genelot D, Trouilloud P, Martin L, Girard C, Danino A, Anderhuber F, Feigl G. 2011; Flexibility of Thiel's embalmed cadavers: the explanation is probably in the muscles. Surg Radiol Anat. 33:365–8. DOI: 10.1007/s00276-010-0703-8. PMID: 20632174.12. Benkhadra M, Faust A, Ladoire S, Trost O, Trouilloud P, Girard C, Anderhuber F, Feigl G. 2009; Comparison of fresh and Thiel's embalmed cadavers according to the suitability for ultrasound-guided regional anesthesia of the cervical region. Surg Radiol Anat. 31:531–5. DOI: 10.1007/s00276-009-0477-z.13. Feigl G, Benkhadra M, Lenfant F, Trouilloud P, Anderhuber F, Bonniaud P, Fasel JH, Nemetz W. 2008; Bronchoscopy and cricothyrotomy: results from cadavers embalmed with Thiel's method compared to other embalming methods and living subjects. Acta Med-Biotech. 1:25–36. DOI: 10.18690/actabiomed.5.14. Windisch G, Ulz H, Feigl G. 2009; Reliability of Tuffier's line evaluated on cadaver specimens. Surg Radiol Anat. 31:627–30. DOI: 10.1007/s00276-009-0493-z. PMID: 19308303.15. Grivas T, Tsilimidos G, Verras C, Botsios K, Chatzisaroglou M. 2013; Which is the most prominent spinous process in the cervico-thoracic spinal junction? A radiological study in a Mediterranean population sample. Scoliosis. 8(Suppl 2):O40. DOI: 10.1186/1748-7161-8-S2-O40.16. Liertzer H. Weinschenk S, editor. [Cervical spine syndrome, Cervical syndrom]. [Neural therapy manual]. Thieme Verlag;2020. p. 727–9. German.17. Groeben H. 2006; Epidural anesthesia and pulmonary function. J Anesth. 20:290–9. DOI: 10.1007/s00540-006-0425-6. PMID: 17072694.18. Arzola C, Avramescu S, Tharmaratnam U, Chin KJ, Balki M. 2011; Identification of cervicothoracic intervertebral spaces by surface landmarks and ultrasound. Can J Anaesth. 58:1069–74. DOI: 10.1007/s12630-011-9587-2. PMID: 21971740.19. Reichert B. Anatomie in vivo. Georg Thieme Verlag;2007.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Variability in the Length of Stay and Daily Medical Expenses in Inpatient Care in Korea, 2010–2019: Hypertension and Pneumonia
- HbA1c Variability and Micro- and Macrovascular Complications of Diabetes
- A radiological study on normal variations of abdominal aorta and its major branches
- Intrapatient variability of tacrolimus trough level may be not the cause, but an indirect parameter of comorbidities: Editorial on “Optimal tacrolimus levels for reducing CKD risk and the impact of intrapatient variability on CKD and ESRD development following liver transplantation”
- Deceased Male with a Cigarette In Situ : Is This a Cadaveric Spasm?