J Korean Foot Ankle Soc.
2024 Sep;28(3):107-110. 10.14193/jkfas.2024.28.3.107.
Surgical Management of Neuropathic Arthropathy due to Rheumatoid Arthritis: A Case Report
- Affiliations
-
- 1Department of Orthopedic Surgery, Wonkwang University Hospital, Iksan, Korea
- KMID: 2559640
- DOI: http://doi.org/10.14193/jkfas.2024.28.3.107
Abstract
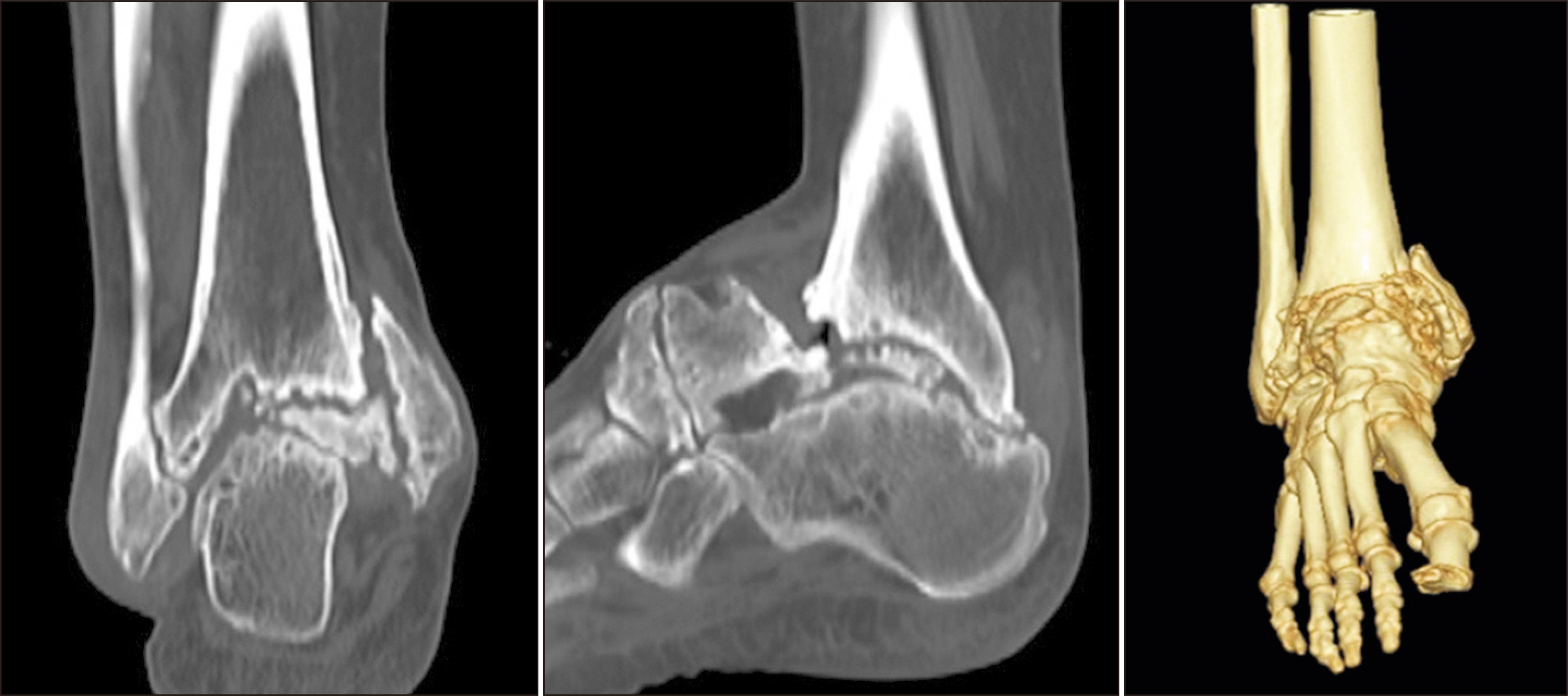
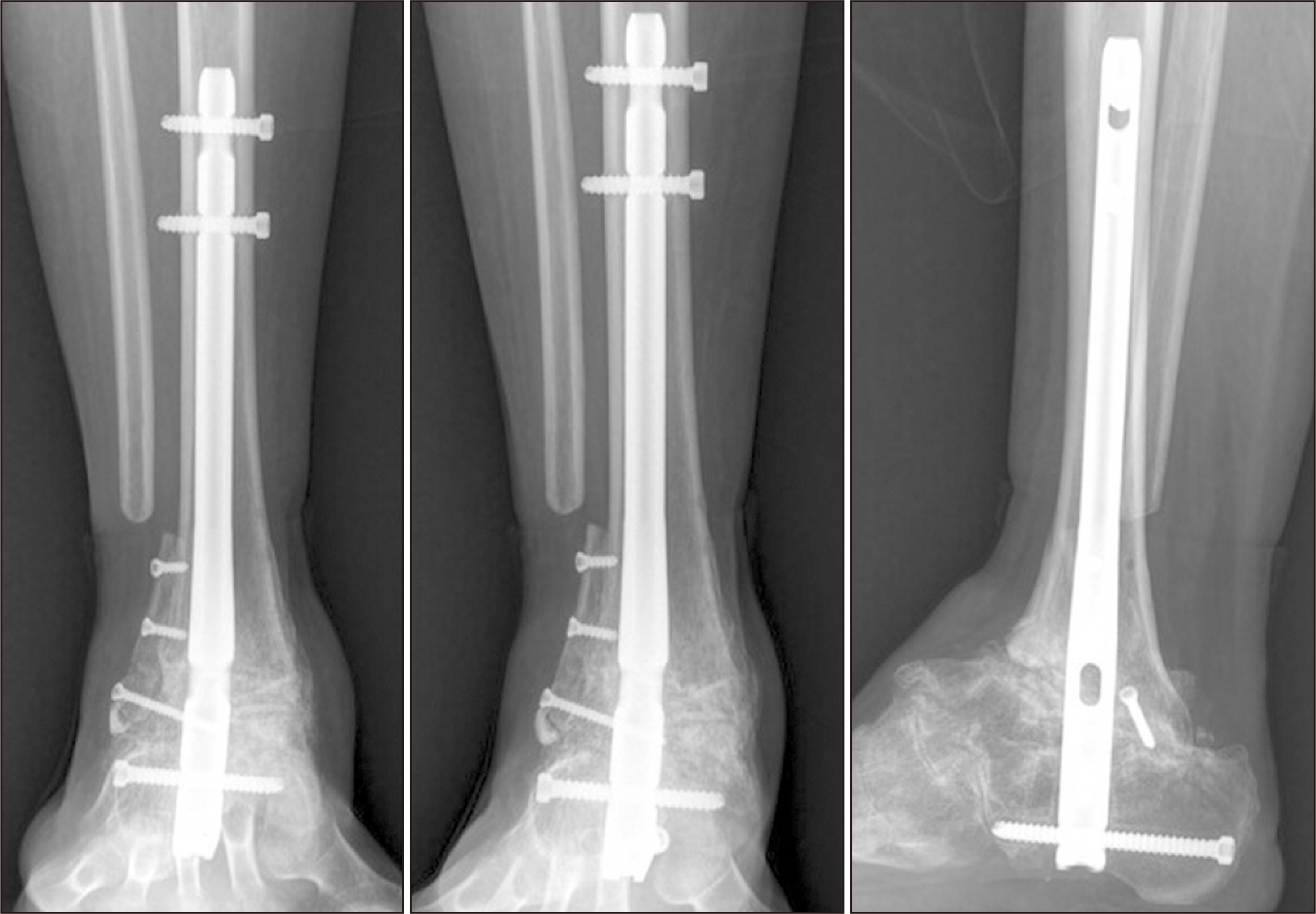
- Neuropathic arthropathy (Charcot arthropathy) is a progressive joint disease often associated with conditions such as diabetes, leading to severe joint deformity and pain. However, its occurrence in patients with rheumatoid arthritis (RA) is rare and not well documented. This case report describes a 48-year-old woman with a long history of RA who developed a severe deformity of her right ankle, identified as neuropathic arthropathy extending to the subtalar joint (Brodsky classification type 3A). After excluding other potential causes, the condition was determined to be secondary to RA-associated peripheral neuropathy. Surgery, including allograft and autograft fixation, was performed to correct the deformity. Post-operative complications, such as wound infection, were treated with negative pressure wound therapy and skin grafting. At the 18-month follow-up, the patient was able to walk without pain, demonstrating successful joint fusion.
Figure
Reference
-
1. Brower AC, Allman RM. 1981; The neuropathic joint: a neurovascular bone disorder. Radiol Clin North Am. 19:571–80. DOI: 10.1016/S0033-8389(22)01344-6.2. Waibel FWA, Böni T. 2022; Nonoperative treatment of Charcot neuro-osteoarthropathy. Foot Ankle Clin. 27:595–616. doi: 10.1016/j.fcl.2022.05.002. DOI: 10.1016/j.fcl.2022.05.002.3. Pinzur MS. 1999; Benchmark analysis of diabetic patients with neuropathic (Charcot) foot deformity. Foot Ankle Int. 20:564–7. doi: 10.1177/107110079902000905. DOI: 10.1177/107110079902000905.4. Bajuri MY, Ong SL, Das S, Mohamed IN. 2022; Charcot neuroarthropathy: current surgical management and update. A systematic review. Front Surg. 9:820826. doi: 10.3389/fsurg.2022.820826. DOI: 10.3389/fsurg.2022.820826.5. Lowery NJ, Woods JB, Armstrong DG, Wukich DK. 2012; Surgical management of Charcot neuroarthropathy of the foot and ankle: a systematic review. Foot Ankle Int. 33:113–21. doi: 10.3113/FAI.2012.0113. DOI: 10.3113/FAI.2012.0113.6. Jensen TS, Karlsson P, Gylfadottir SS, Andersen ST, Bennett DL, Tankisi H, et al. 2021; Painful and non-painful diabetic neuropathy, diagnostic challenges and implications for future management. Brain. 144:1632–45. doi: 10.1093/brain/awab079. DOI: 10.1093/brain/awab079.7. Gilbert L, He X, Farmer P, Boden S, Kozlowski M, Rubin J, et al. 2000; Inhibition of osteoblast differentiation by tumor necrosis factor-alpha. Endocrinology. 141:3956–64. doi: 10.1210/endo.141.11.7739. DOI: 10.1210/endo.141.11.7739.8. Grear BJ, Rabinovich A, Brodsky JW. 2013; Charcot arthropathy of the foot and ankle associated with rheumatoid arthritis. Foot Ankle Int. 34:1541–7. doi: 10.1177/1071100713500490. DOI: 10.1177/1071100713500490.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Neuropathic Arthropathy Induced by Syringomyelia due to Arnold-Chiari I Malformation: A case report
- A Case of CPPD Crystal Deposition Disease in a Patient with Rheumatoid Arthritis and Systemic Sclerosis
- Surgical management of the knee in rheumatoid arthritis
- Idiopathic Charcot-like Arthropathy: A case report
- Neuropathic Arthropathy of the Elbow