J Cerebrovasc Endovasc Neurosurg.
2024 Sep;26(3):260-264. 10.7461/jcen.2024.E2023.09.003.
Optimizing suction force in mechanical thrombectomy: Priming the aspiration tubing with air versus saline
- Affiliations
-
- 1Department of Neurological Surgery, University of California, San Diego, USA
- 2Department of General Surgery, University of California, San Diego, USA
- 3Program in Materials Science and Engineering, University of California, San Diego, USA
- KMID: 2559435
- DOI: http://doi.org/10.7461/jcen.2024.E2023.09.003
Abstract
Objective
We sought to investigate how priming the tube between air versus air mixed with saline ex vivo influenced suction force. We examined how priming the tube influenced peak suction force and time to achieve peak suction force between both modalities.
Methods
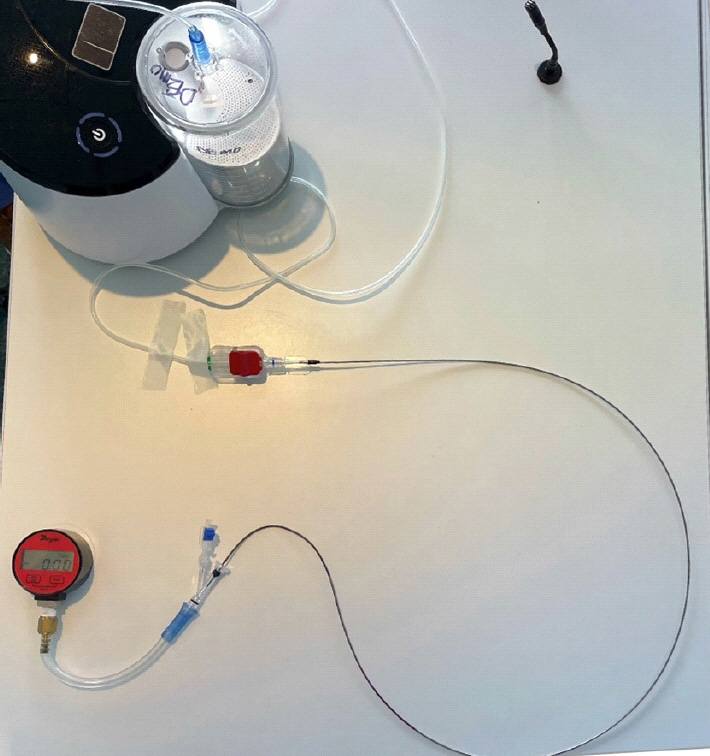
Using a Dwyer Instruments (Dwyer Instruments Inc., Michigan City, IN, USA), INC Digitial Pressure Gauge, we were able to connect a .072 inch aspiration catheter to a rotating hemostatic valve and to aspiration tubing. We recorded suction force measured in negative inches of Mercury (inHg) over 10 iterations between having the aspiration tube primed with air alone versus air mixed with saline. A test was used to compare results between both modalities.
Results
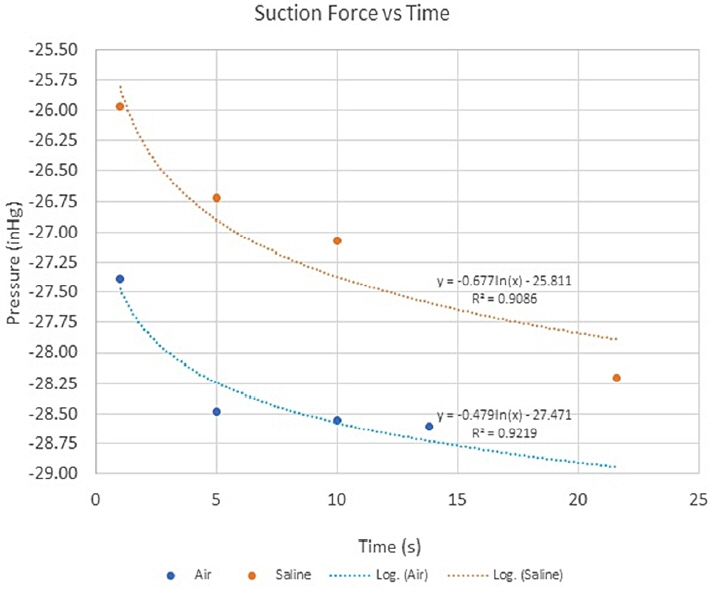
Priming the tube with air alone compared to air mixed with saline was found to have an increased average max suction force (-28.60 versus -28.20 in HG, p<0.01). We also identified a logarithmic curve of suction force across time in which time to maximal suction force was more prompt with air compared with air mixed with saline (13.8 seconds versus 21.60 seconds, p<0.01).
Conclusions
Priming the tube with air compared to air mixed with saline suggests that not only is increased maximal suction force achieved, but also the time required to achieve maximal suction force is less. This data suggests against priming the aspiration tubing with saline and suggests that the first pass aspiration primed with air may have the greatest suction force.
Keyword
Figure
Reference
-
1. Abbasi M, Liu Y, Fitzgerald S, Mereuta OM, Arturo Larco JL, Rizvi A, et al. Systematic review and meta-analysis of current rates of first pass effect by thrombectomy technique and associations with clinical outcomes. J Neurointerv Surg. 2021; Mar. 13(3):212–6.
Article2. Boisseau W, Escalard S, Fahed R, Lapergue B, Smajda S, Maier B, et al. Direct aspiration stroke thrombectomy: A comprehensive review. J Neurointerv Surg. 2020; Nov. 12(11):1099–106.3. Froehler MT. Comparison of vacuum pressures and forces generated by different catheters and pumps for aspiration thrombectomy in acute ischemic stroke. Interv Neurol. 2017; Oct. 6(3-4):199–206.4. Goyal N, Tsivgoulis G, Frei D, Turk A, Baxter B, Froehler MT, et al. Comparative safety and efficacy of modified TICI 2b and TICI 3 reperfusion in acute ischemic strokes treated with mechanical thrombectomy. Neurosurgery. 2019; Mar. 84(3):680–6.5. Jang KM, Choi HH, Nam TK, Byun JS. Clinical outcomes of first-pass effect after mechanical thrombectomy for acute ischemic stroke: A systematic review and meta-analysis. Clin Neurol Neurosurg. 2021; Dec. 211:107030.
Article6. Jeon JP, Kim SE, Kim CH. Primary suction thrombectomy for acute ischemic stroke: A meta-analysis of the current literature. Clin Neurol Neurosurg. 2017; Dec. 163:46–52.
Article7. Kim S, Lee JY. Comparison of vacuum pressures and suction forces generated by different pump systems for aspiration thrombectomy. Front Neurol. 2022; Oct. 13:978584.8. Lapergue B, Blanc R, Gory B, Labreuche J, Duhamel A, Marnat G, et al. Effect of endovascular contact aspiration vs stent retriever on revascularization in patients with acute ischemic stroke and large vessel occlusion: The ASTER randomized clinical trial. JAMA. 2017; Aug. 318(5):443–52.9. Long TD, Kallmes DF, Hanel R, Shigematsu T, Halaszyn AM, Wolter J, et al. Novel aspiration catheter design for acute stroke thrombectomy. J Neurointerv Surg. 2019; Feb. 11(2):190–5.
Article10. Nikoubashman O, Dekeyzer S, Riabikin A, Keulers A, Reich A, Mpotsaris A, et al. True first-pass effect. Stroke. 2019; Aug. 50(8):2140–6.11. Nikoubashman O, Nikoubashman A, Büsen M, Wiesmann M. Necessary catheter diameters for mechanical thrombectomy with ADAPT. AJNR Am J Neuroradiol. 2017; Dec. 38(12):2277–81.12. Rennert RC, Wali AR, Steinberg JA, Santiago-Dieppa DR, Olson SE, Pannell JS, et al. Epidemiology, natural history, and clinical presentation of large vessel ischemic stroke. Neurosurgery. 2019; Jul. 85(suppl 1):S4–8.
Article13. Simon S, Grey CP, Massenzo T, Simpson DG, Longest PW. Exploring the efficacy of cyclic vs static aspiration in a cerebral thrombectomy model: An initial proof of concept study. J Neurointerv Surg. 2014; Nov. 6(9):677–83.14. Yaeger K, Iserson A, Singh P, Wolf J, Vidal E, Oxley T, et al. A technical comparison of thrombectomy vacuum aspiration systems. J Neurointerv Surg. 2020; Jan. 12(1):72–6.15. Yoo AJ, Andersson T. Thrombectomy in acute ischemic stroke: Challenges to procedural success. J Stroke. 2017; May. 19(2):121–30.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Forced Arterial Suction Thrombectomy Using Distal Access Catheter in Acute Ischemic Stroke
- Suction thrombectomy of distal medium vessel occlusion using microcatheter during mechanical thrombectomy for acute ischemic stroke: A case series
- Pseudoaneurysm Formation after Repetitive Suction Thrombectomy Using a Penumbra Suction Catheter
- Real-Time Visualization of Thrombus during Suction Thrombectomy : Contrast-in-Stasis Technique
- Endovascular Stroke Therapy Focused on Stent Retriever Thrombectomy and Direct Clot Aspiration: Historical Review and Modern Application