Clin Endosc.
2024 Sep;57(5):610-619. 10.5946/ce.2023.236.
Timed barium esophagography to predict recurrent achalasia after peroral endoscopic myotomy: a retrospective study in Thailand
- Affiliations
-
- 1Minimally Invasive Surgery Unit, Department of Surgery, Faculty of Medicine Siriraj Hospital, Mahidol University, Bangkok, Thailand
- 2Graduate School of Medical and Dental Sciences, Tokyo Medical and Dental University, Tokyo, Japan
- 3Division of Gastroenterology, Department of Medicine, Faculty of Medicine Siriraj Hospital, Mahidol University, Bangkok, Thailand
- 4Department of Radiology, Faculty of Medicine Siriraj Hospital, Mahidol University, Bangkok, Thailand
- KMID: 2559212
- DOI: http://doi.org/10.5946/ce.2023.236
Abstract
- Background/Aims
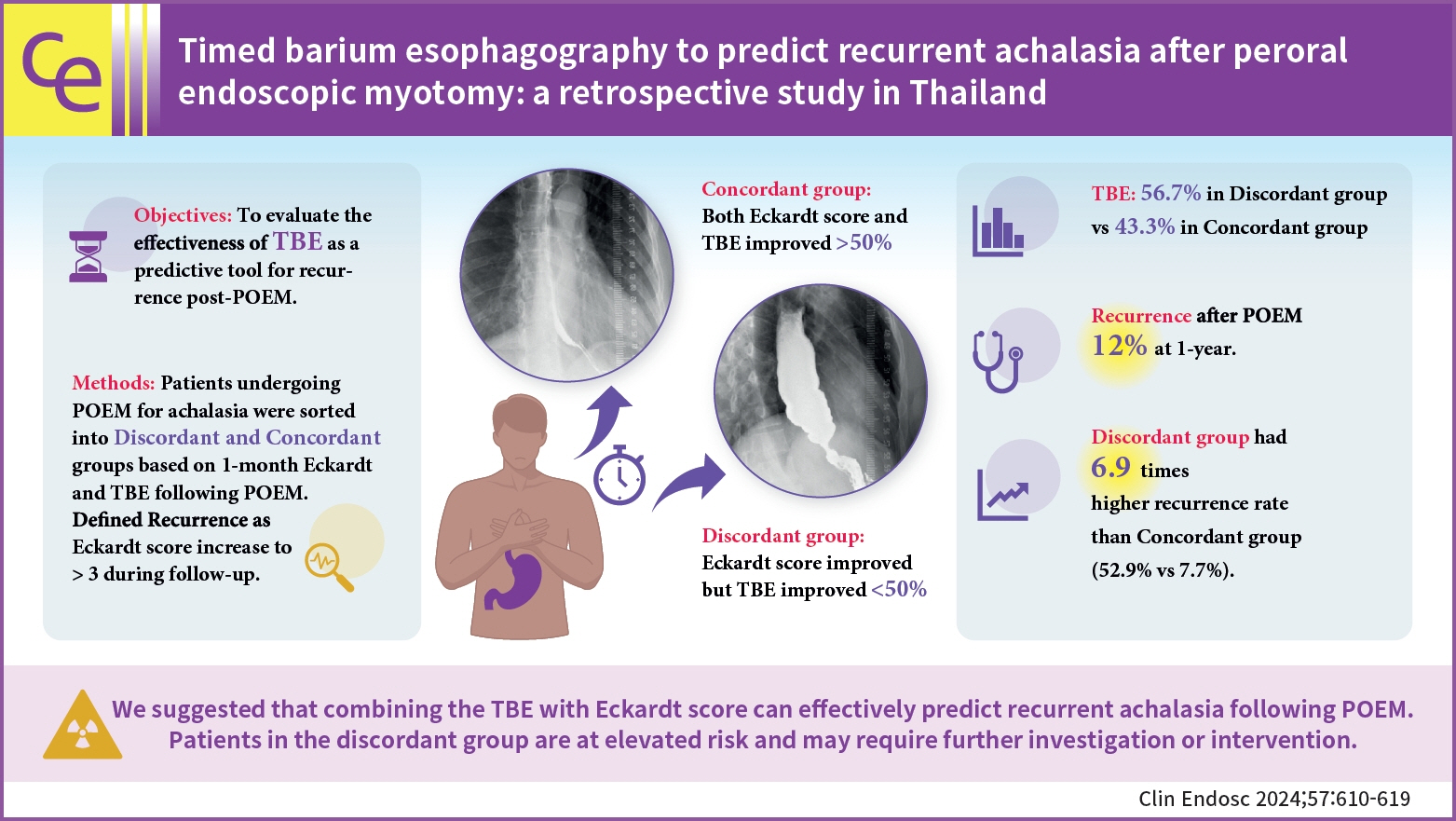
Achalasia is a rare esophageal motility disease, for which peroral endoscopic myotomy (POEM) has emerged as a promising treatment option; however, recurrence remains a challenge. Timed barium esophagography (TBE) is a useful diagnostic tool and potential outcome predictor of achalasia. This study aimed to determine predictive tools for recurrence after POEM.
Methods
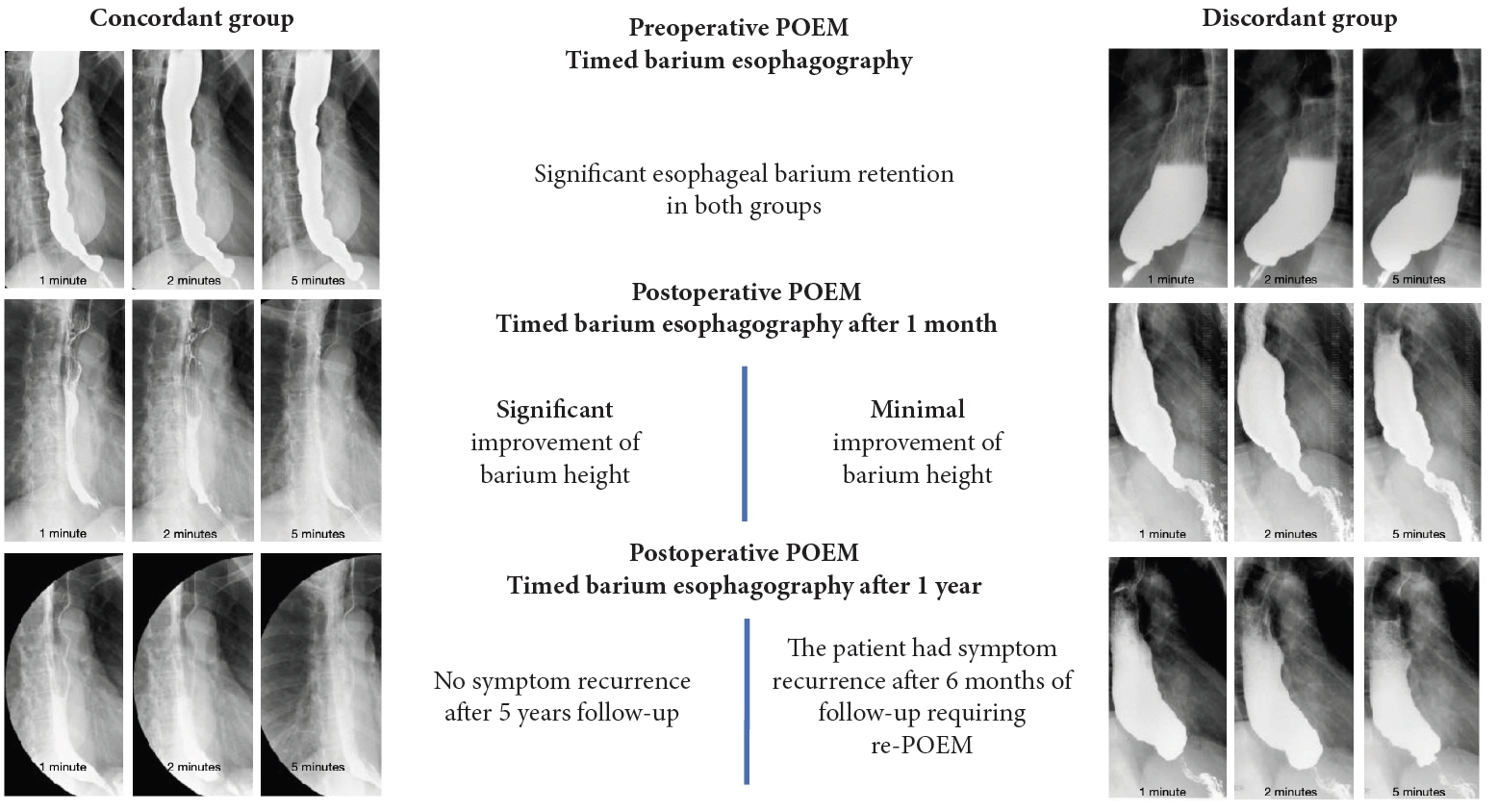
This retrospective study enrolled achalasia patients who underwent POEM between January 2015 and December 2021. Patients were categorized into two groups using the 1-month post-POEM Eckardt scores and TBE: the discordant group (Eckardt score improved >50%, TBE decreased <50%) and the concordant group (both Eckardt score and TBE improved >50%). Recurrence was defined as a reincrease in the Eckardt score to more than three during follow-up.
Results
Complete medical records were available in 30 patients who underwent POEM. Seventeen patients (56.7%) were classified into the discordant group, while 13 patients (43.3%) were in the concordant group. The overall recurrence rate was 11.9% at 1-year, increasing to 23.8% during the extended follow-up. The discordant group had a 6.87 fold higher recurrence rate than the concordant group (52.9% vs. 7.7%, p=0.017).
Conclusions
These results strongly suggest that combining the Eckardt score with TBE can effectively predict recurrent achalasia after POEM. Patients in the discordant group had an elevated risk.
Keyword
Figure
Reference
-
1. Duffield JA, Hamer PW, Heddle R, et al. Incidence of achalasia in south Australia based on esophageal manometry findings. Clin Gastroenterol Hepatol. 2017; 15:360–365.2. Riccio F, Costantini M, Salvador R. Esophageal achalasia: diagnostic evaluation. World J Surg. 2022; 46:1516–1521.3. Vaezi MF, Baker ME, Achkar E, et al. Timed barium oesophagram: better predictor of long term success after pneumatic dilation in achalasia than symptom assessment. Gut. 2002; 50:765–770.4. Eckardt VF, Aignherr C, Bernhard G. Predictors of outcome in patients with achalasia treated by pneumatic dilation. Gastroenterology. 1992; 103:1732–1738.5. Blonski W, Kumar A, Feldman J, et al. Timed barium swallow: diagnostic role and predictive value in untreated achalasia, esophagogastric junction outflow obstruction, and non-achalasia dysphagia. Am J Gastroenterol. 2018; 113:196–203.6. Swanström LL. Achalasia: treatment, current status and future advances. Korean J Intern Med. 2019; 34:1173–1180.7. Vaezi MF, Pandolfino JE, Yadlapati RH, et al. ACG Clinical Guidelines: diagnosis and management of achalasia. Am J Gastroenterol. 2020; 115:1393–1411.8. Jung HK, Hong SJ, Lee OY, et al. 2019 Seoul consensus on esophageal achalasia guidelines. J Neurogastroenterol Motil. 2020; 26:180–203.9. Oude Nijhuis RA, Zaninotto G, Roman S, et al. European guidelines on achalasia: United European Gastroenterology and European Society of Neurogastroenterology and Motility recommendations. United European Gastroenterol J. 2020; 8:13–33.10. Khashab MA, Vela MF, Thosani N, et al. ASGE guideline on the management of achalasia. Gastrointest Endosc. 2020; 91:213–227.11. Inoue H, Shiwaku H, Iwakiri K, et al. Clinical practice guidelines for peroral endoscopic myotomy. Dig Endosc. 2018; 30:563–579.12. van Hoeij FB, Ponds FA, Werner Y, et al. Management of recurrent symptoms after per-oral endoscopic myotomy in achalasia. Gastrointest Endosc. 2018; 87:95–101.13. Wang L, Li YM. Recurrent achalasia treated with Heller myotomy: a review of the literature. World J Gastroenterol. 2008; 14:7122–7126.14. Bonatti H, Hinder RA, Klocker J, et al. Long-term results of laparoscopic Heller myotomy with partial fundoplication for the treatment of achalasia. Am J Surg. 2005; 190:874–878.15. Milito P, Siboni S, Lovece A, et al. Revisional therapy for recurrent symptoms after Heller myotomy for achalasia. J Gastrointest Surg. 2022; 26:64–69.16. Neyaz Z, Gupta M, Ghoshal UC. How to perform and interpret timed barium esophagogram. J Neurogastroenterol Motil. 2013; 19:251–256.17. Boonsomjint W, Maneerattanaporn M, Charoensak A. Correlation between timed barium esophagogram and the Eckardt stage in achalasia. Siriraj Med J. 2018; 70:60–65.18. DeWitt JM, Siwiec RM, Perkins A, et al. Evaluation of timed barium esophagram after per-oral endoscopic myotomy to predict clinical response. Endosc Int Open. 2021; 9:E1692–E1701.19. Kachala SS, Rice TW, Baker ME, et al. Value of routine timed barium esophagram follow-up in achalasia after myotomy. J Thorac Cardiovasc Surg. 2018; 156:871–877.20. Alderliesten J, Conchillo JM, Leeuwenburgh I, et al. Predictors for outcome of failure of balloon dilatation in patients with achalasia. Gut. 2011; 60:10–16.21. Eckardt AJ, Eckardt VF. Treatment and surveillance strategies in achalasia: an update. Nat Rev Gastroenterol Hepatol. 2011; 8:311–319.22. Urakami S, Abe H, Tanaka S, et al. Development of a preoperative risk-scoring system for predicting poor responders to peroral endoscopic myotomy. Gastrointest Endosc. 2021; 93:398–405.23. Phalanusitthepha C, Inoue H, Ikeda H, et al. Peroral endoscopic myotomy for esophageal achalasia. Ann Transl Med. 2014; 2:31.24. Schlottmann F, Luckett DJ, Fine J, et al. Laparoscopic Heller myotomy versus peroral endoscopic myotomy (POEM) for achalasia: a systematic review and meta-analysis. Ann Surg. 2018; 267:451–460.25. Abe H, Tanaka S, Sato H, et al. Risk scoring system for the preprocedural prediction of the clinical failure of peroral endoscopic myotomy: a multicenter case-control study. Endoscopy. 2023; 55:217–224.26. Ates F, Vaezi MF. The pathogenesis and management of achalasia: current status and future directions. Gut Liver. 2015; 9:449–463.27. Katsumata R, Manabe N, Sakae H, et al. Clinical characteristics and manometric findings of esophageal achalasia-a systematic review regarding differences among three subtypes. J Smooth Muscle Res. 2023; 59:14–27.28. Li MY, Wang QH, Chen RP, et al. Pathogenesis, clinical manifestations, diagnosis, and treatment progress of achalasia of cardia. World J Clin Cases. 2023; 11:1741–1752.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Never judge a book by its cover: the role of timed barium esophagography in patients with complete symptom relief after peroral endoscopic myotomy
- Perspective on Peroral Endoscopic Myotomy for Achalasia: Zhongshan Experience
- Two-Stage Peroral Endoscopic Myotomy for Sigmoid-Type Achalasia
- Current Status of Peroral Endoscopic Myotomy
- Achalasia