Diabetes Metab J.
2024 Sep;48(5):993-1002. 10.4093/dmj.2023.0410.
Prognostic Value of Plasma Endothelin-1 in Predicting Worse Outcomes in Patients with Prediabetes and Diabetes and Stable Coronary Artery Diseases
- Affiliations
-
- 1Cardiometabolic Center, Fuwai Hospital, National Center for Cardiovascular Diseases, Chinese Academy of Medical Sciences and Peking Union Medical College, Beijing, China
- 2Department of Cardiology, Fuwai Hospital, National Center for Cardiovascular Diseases, Chinese Academy of Medical Sciences and Peking Union Medical College, Beijing, China
- KMID: 2559008
- DOI: http://doi.org/10.4093/dmj.2023.0410
Abstract
- Background
Endothelin-1 (ET-1) is an endogenous vasoconstrictor implicated in coronary artery disease (CAD) and diabetes. This study aimed to determine the prognostic value of ET-1 in the patients with stable CAD under different glucose metabolism states.
Methods
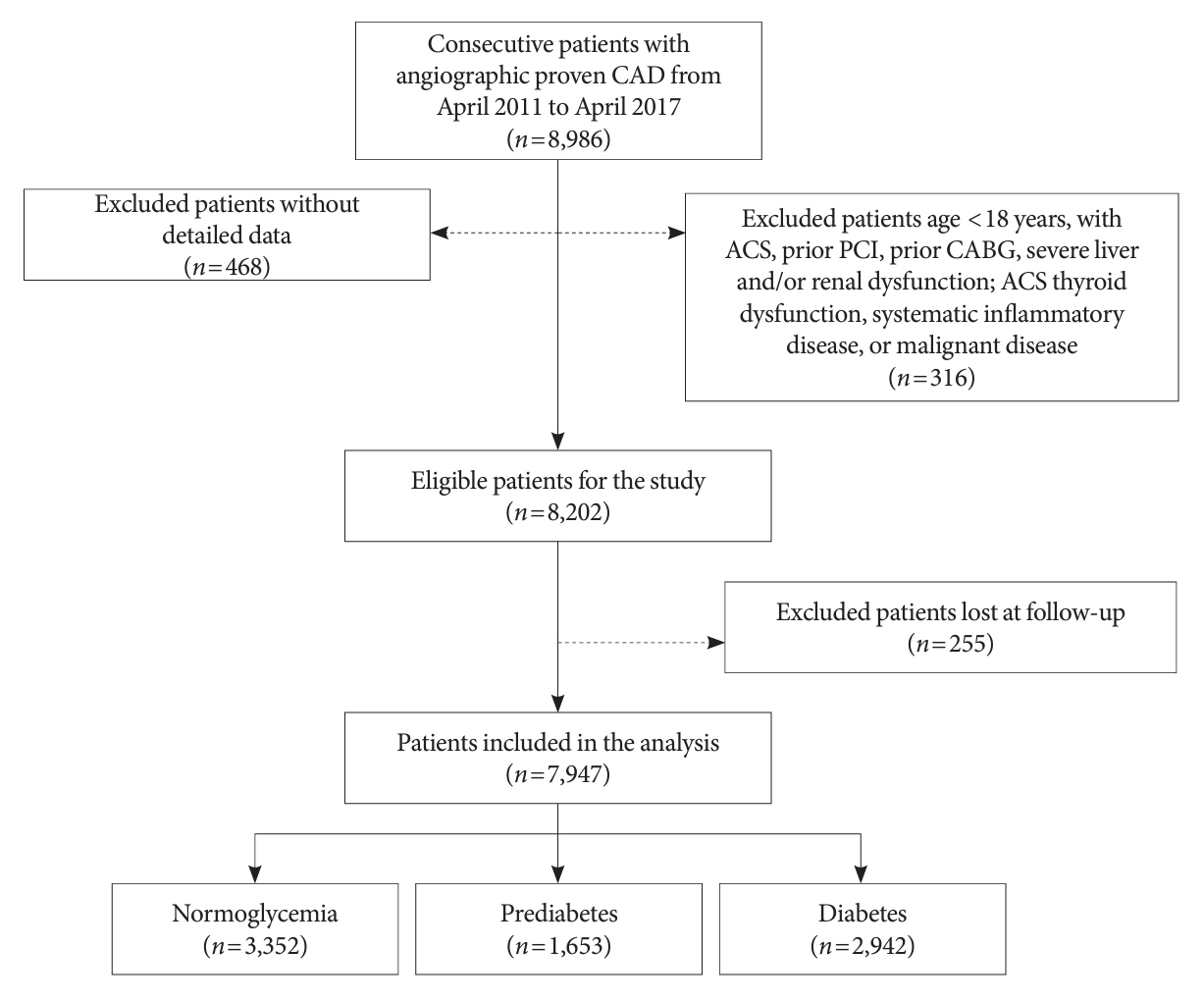
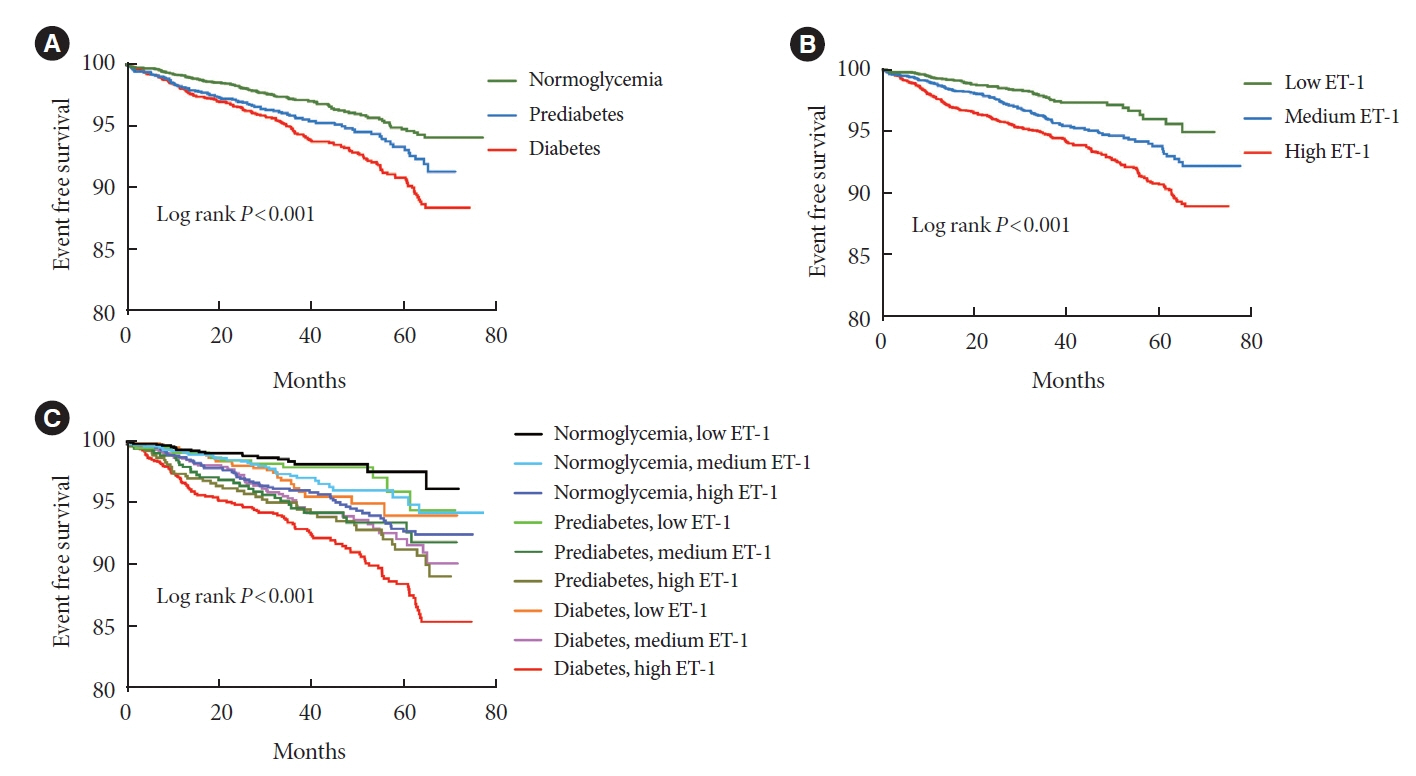
In this prospective, large-cohort study, we consecutively enrolled 7,947 participants with angiography-diagnosed stable CAD from April 2011 to April 2017. Patients were categorized by baseline glycemic status into three groups (normoglycemia, prediabetes, and diabetes) and further divided into nine groups by circulating ET-1 levels. Patients were followed for the occurrence of cardiovascular events (CVEs), including nonfatal myocardial infarction, stroke, and cardiovascular mortality.
Results
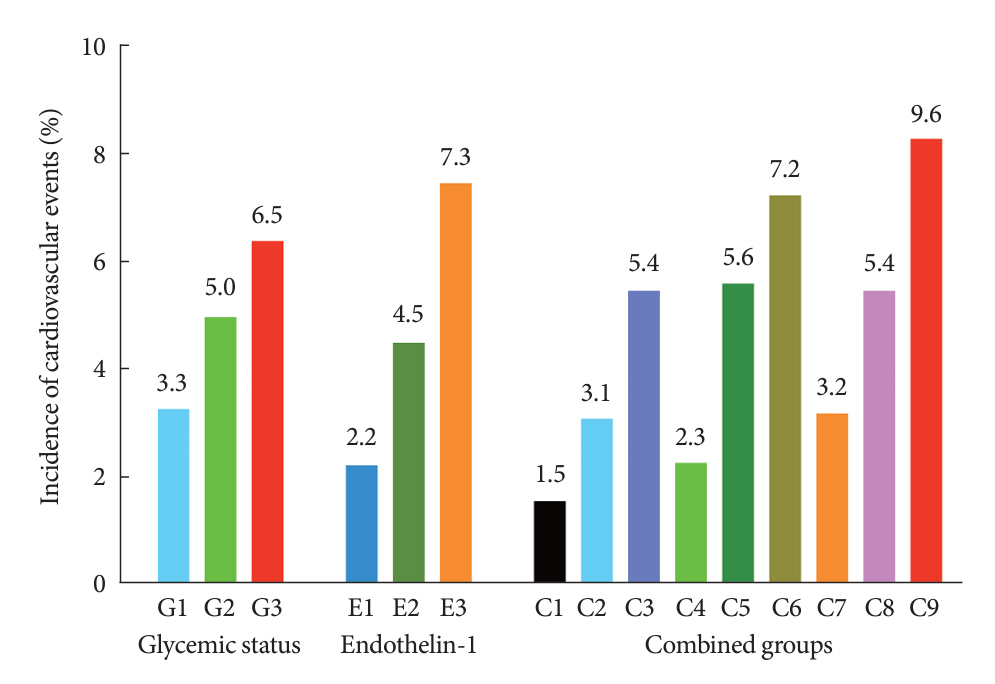
Of the 7,947 subjects, 3,352, 1,653, and 2,942 had normoglycemia, prediabetes, and diabetes, respectively. Over a median follow-up of 37.5 months, 381 (5.1%) CVEs occurred. The risk for CVEs was significantly higher in patients with elevated ET-1 levels after adjustment for potential confounders. When patients were categorized by both status of glucose metabolism and plasma ET-1 levels, the high ET-1 levels were associated with higher risk of CVEs in prediabetes (adjusted hazard ratio [HR], 2.089; 95% confidence interval [CI], 1.151 to 3.793) and diabetes (adjusted HR, 2.729; 95% CI, 1.623 to 4.588; both P<0.05).
Conclusion
The present study indicated that baseline plasma ET-1 levels were associated with the prognosis in prediabetic and diabetic patients with stable CAD, suggesting that ET-1 may be a valuable predictor in CAD patients with impaired glucose metabolism.
Figure
Reference
-
1. GBD 2019 Risk Factors Collaborators. Global burden of 87 risk factors in 204 countries and territories, 1990-2019: a systematic analysis for the Global Burden of Disease Study 2019. Lancet. 2020; 396:1223–49.2. Roth GA, Mensah GA, Johnson CO, Addolorato G, Ammirati E, Baddour LM, et al. Global burden of cardiovascular diseases and risk factors, 1990-2019: update from the GBD 2019 Study. J Am Coll Cardiol. 2020; 76:2982–3021.3. Fox CS, Golden SH, Anderson C, Bray GA, Burke LE, de Boer IH, et al. Update on prevention of cardiovascular disease in adults with type 2 diabetes mellitus in light of recent evidence: a scientific statement from the American Heart Association and the American Diabetes Association. Circulation. 2015; 132:691–718.
Article4. Kelsey MD, Nelson AJ, Green JB, Granger CB, Peterson ED, McGuire DK, et al. Guidelines for cardiovascular risk reduction in patients with type 2 diabetes: JACC guideline comparison. J Am Coll Cardiol. 2022; 79:1849–57.5. Liu Y, Yang YM, Zhu J, Tan HQ, Liang Y, Li JD. Prognostic significance of hemoglobin A1c level in patients hospitalized with coronary artery disease: a systematic review and meta-analysis. Cardiovasc Diabetol. 2011; 10:98.
Article6. Paneni F, Beckman JA, Creager MA, Cosentino F. Diabetes and vascular disease: pathophysiology, clinical consequences, and medical therapy: part I. Eur Heart J. 2013; 34:2436–43.
Article7. Tabak AG, Herder C, Rathmann W, Brunner EJ, Kivimaki M. Prediabetes: a high-risk state for diabetes development. Lancet. 2012; 379:2279–90.
Article8. Echouffo-Tcheugui JB, Perreault L, Ji L, Dagogo-Jack S. Diagnosis and management of prediabetes: a review. JAMA. 2023; 329:1206–16.
Article9. Sun H, Saeedi P, Karuranga S, Pinkepank M, Ogurtsova K, Duncan BB, et al. IDF Diabetes Atlas: global, regional and country-level diabetes prevalence estimates for 2021 and projections for 2045. Diabetes Res Clin Pract. 2022; 183:109119.
Article10. Huang Y, Cai X, Mai W, Li M, Hu Y. Association between pre-diabetes and risk of cardiovascular disease and all cause mortality: systematic review and meta-analysis. BMJ. 2016; 355:i5953.
Article11. Cai X, Zhang Y, Li M, Wu JH, Mai L, Li J, et al. Association between prediabetes and risk of all cause mortality and cardiovascular disease: updated meta-analysis. BMJ. 2020; 370:m2297.
Article12. Yanagisawa M, Kurihara H, Kimura S, Tomobe Y, Kobayashi M, Mitsui Y, et al. A novel potent vasoconstrictor peptide produced by vascular endothelial cells. Nature. 1988; 332:411–5.
Article13. Schooling CM, Kodali H, Li S, Borrell LN. ET (endothelin)-1 and ischemic heart disease: a mendelian randomization study. Circ Genom Precis Med. 2018; 11:e002026.14. Ergul A. Endothelin-1 and diabetic complications: focus on the vasculature. Pharmacol Res. 2011; 63:477–82.
Article15. Kohan DE, Barton M. Endothelin and endothelin antagonists in chronic kidney disease. Kidney Int. 2014; 86:896–904.
Article16. Perez AL, Grodin JL, Wu Y, Hernandez AF, Butler J, Metra M, et al. Increased mortality with elevated plasma endothelin-1 in acute heart failure: an ASCEND-HF biomarker substudy. Eur J Heart Fail. 2016; 18:290–7.
Article17. Sabatine MS, Morrow DA, de Lemos JA, Omland T, Sloan S, Jarolim P, et al. Evaluation of multiple biomarkers of cardiovascular stress for risk prediction and guiding medical therapy in patients with stable coronary disease. Circulation. 2012; 125:233–40.
Article18. Zhou BY, Guo YL, Wu NQ, Zhu CG, Gao Y, Qing P, et al. Plasma big endothelin-1 levels at admission and future cardiovascular outcomes: a cohort study in patients with stable coronary artery disease. Int J Cardiol. 2017; 230:76–9.
Article19. Schnabel RB, Schulz A, Messow CM, Lubos E, Wild PS, Zeller T, et al. Multiple marker approach to risk stratification in patients with stable coronary artery disease. Eur Heart J. 2010; 31:3024–31.
Article20. American Diabetes Association. Diagnosis and classification of diabetes mellitus. Diabetes Care. 2011; 34(Suppl 1):S62–9.21. Kawanabe Y, Nauli SM. Endothelin. Cell Mol Life Sci. 2011; 68:195–203.
Article22. Dhaun N, Webb DJ. Endothelins in cardiovascular biology and therapeutics. Nat Rev Cardiol. 2019; 16:491–502.
Article23. Sakurai T, Yanagisawa M, Takuwa Y, Miyazaki H, Kimura S, Goto K, et al. Cloning of a cDNA encoding a non-isopeptide-selective subtype of the endothelin receptor. Nature. 1990; 348:732–5.
Article24. Jain A. Endothelin-1-induced endoplasmic reticulum stress in disease. J Pharmacol Exp Ther. 2013; 346:163–72.
Article25. Eroglu E, Kocyigit I, Lindholm B. The endothelin system as target for therapeutic interventions in cardiovascular and renal disease. Clin Chim Acta. 2020; 506:92–106.
Article26. GBD 2017 Causes of Death Collaborators. Global, regional, and national age-sex-specific mortality for 282 causes of death in 195 countries and territories, 1980-2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet. 2018; 392:1736–88.27. Vaduganathan M, Mensah GA, Turco JV, Fuster V, Roth GA. The global burden of cardiovascular diseases and risk: a compass for future health. J Am Coll Cardiol. 2022; 80:2361–71.28. Barton M, Yanagisawa M. Endothelin: 30 years from discovery to therapy. Hypertension. 2019; 74:1232–65.
Article29. Hu DY, Pan CY, Yu JM; China Heart Survey Group. The relationship between coronary artery disease and abnormal glucose regulation in China: the China Heart Survey. Eur Heart J. 2006; 27:2573–9.
Article30. Ding D, Qiu J, Li X, Li D, Xia M, Li Z, et al. Hyperglycemia and mortality among patients with coronary artery disease. Diabetes Care. 2014; 37:546–54.
Article31. Færch K, Johansen NB, Witte DR, Lauritzen T, Jorgensen ME, Vistisen D. Relationship between insulin resistance and β-cell dysfunction in subphenotypes of prediabetes and type 2 diabetes. J Clin Endocrinol Metab. 2015; 100:707–16.
Article32. Lorenzo C, Wagenknecht LE, Hanley AJ, Rewers MJ, Karter AJ, Haffner SM. A1C between 5.7 and 6.4% as a marker for identifying pre-diabetes, insulin sensitivity and secretion, and cardiovascular risk factors: the Insulin Resistance Atherosclerosis Study (IRAS). Diabetes Care. 2010; 33:2104–9.33. Einarson TR, Acs A, Ludwig C, Panton UH. Prevalence of cardiovascular disease in type 2 diabetes: a systematic literature review of scientific evidence from across the world in 2007-2017. Cardiovasc Diabetol. 2018; 17:83.
Article34. Schneider JG, Tilly N, Hierl T, Sommer U, Hamann A, Dugi K, et al. Elevated plasma endothelin-1 levels in diabetes mellitus. Am J Hypertens. 2002; 15:967–72.
Article35. Matsumoto T, Ozawa Y, Taguchi K, Kobayashi T, Kamata K. Diabetes-associated changes and role of N epsilon-(carboxym ethyl)lysine in big ET-1-induced coronary vasoconstriction. Peptides. 2010; 31:346–53.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Pain and Associated Symptoms in Patients with Acute Coronary Syndrome and Stable Coronary Artery Diseases: A Comparative Study
- Long-term association of pericardial adipose tissue with incident diabetes and prediabetes: the Coronary Artery Risk Development in Young Adults Study
- Changes of Plasma Endothelin-1 Concentration after Percutaneous Mitral Commissurotomy
- Serum Cystatin C as a Biomarker for Predicting Coronary Artery Disease in Diabetes
- Effects of Halothane on Endothelin-1 Production in coronary Circulation following Myocardial Ischemia-Reperfusion in Dogs