Ann Hepatobiliary Pancreat Surg.
2024 Aug;28(3):337-343. 10.14701/ahbps.24-020.
Donor body mass index over 30 is no barrier for pure laparoscopic donor right hepatectomy
- Affiliations
-
- 1Department of Surgery, Seoul National University College of Medicine, Seoul, Korea
- KMID: 2558657
- DOI: http://doi.org/10.14701/ahbps.24-020
Abstract
- Backgrounds/Aims
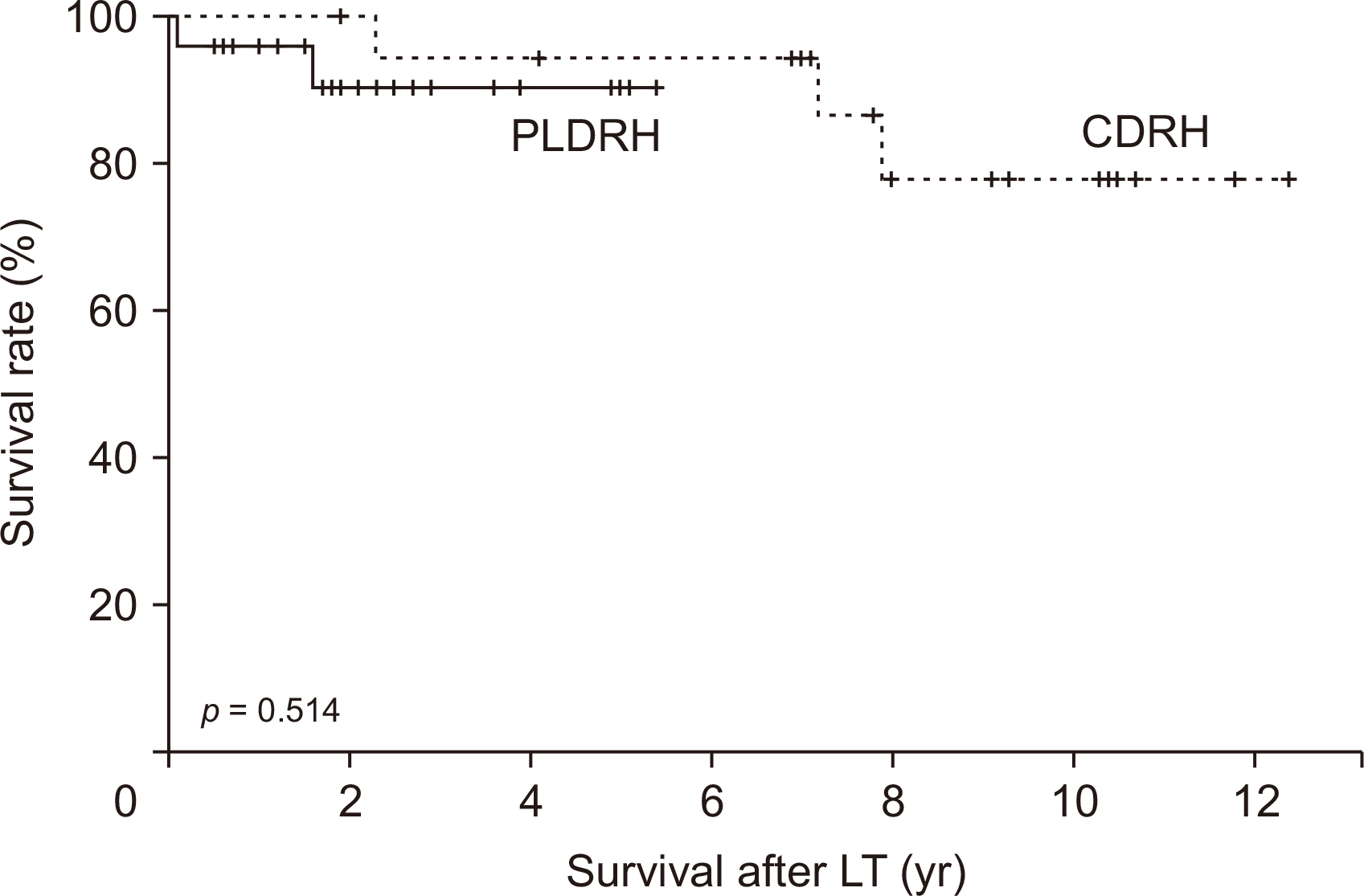
Challenges arise when translating pure laparoscopic donor right hepatectomy (PLDRH) results from Asian to Western donors, due to differences in body mass index (BMI). This study compares the outcomes of PLDRH and conventional open donor right hepatectomy (CDRH) in donors with BMI over 30.
Methods
Medical records of live liver donors (BMI > 30) undergoing right hepatectomy (2010−2021) were compared: 25 PLDRH cases vs. 19 CDRH cases. Donor and recipient demographics, operative details, and outcomes were analyzed.
Results
PLDRH and CDRH had similar donor and recipient characteristics. PLDRH had longer liver removal and warm ischemic times, but a shorter post-liver removal duration than CDRH. Donor complication rates were comparable, with the highest complication being grade IIIa in PLDRH, necessitating needle aspiration for biloma on postoperative day 11. Fortunately, this donor fully recovered without additional treatment. No complications exceeding Clavien–Dindo grade IIIa occurred in either group. Recipient outcomes between the groups were similar.
Conclusions
This study supports PLDRH as a viable option for donors with BMI over 30, challenging the notion that high BMI should deter considering PLDRH. The findings provide valuable insights into the safety and feasibility of PLDRH, encouraging further exploration of this technique in diverse donor populations.
Keyword
Figure
Reference
-
References
1. Cherqui D, Soubrane O, Husson E, Barshasz E, Vignaux O, Ghimouz M, et al. 2002; Laparoscopic living donor hepatectomy for liver transplantation in children. Lancet. 359:392–396. DOI: 10.1016/S0140-6736(02)07598-0. PMID: 11844509.2. Rotellar F, Pardo F, Benito A, Martí-Cruchaga P, Zozaya G, Lopez L, et al. 2013; Totally laparoscopic right-lobe hepatectomy for adult living donor liver transplantation: useful strategies to enhance safety. Am J Transplant. 13:3269–3273. DOI: 10.1111/ajt.12471. PMID: 24266975.3. Samstein B, Cherqui D, Rotellar F, Griesemer A, Halazun KJ, Kato T, et al. 2013; Totally laparoscopic full left hepatectomy for living donor liver transplantation in adolescents and adults. Am J Transplant. 13:2462–2466. DOI: 10.1111/ajt.12360. PMID: 24034709.4. Soubrane O, Perdigao Cotta F, Scatton O. 2013; Pure laparoscopic right hepatectomy in a living donor. Am J Transplant. 13:2467–2471. DOI: 10.1111/ajt.12361. PMID: 23865716.5. Buell JF, Cherqui D, Geller DA, O'Rourke N, Iannitti D, Dagher I, et al. 2008; The international position on laparoscopic liver surgery: the Louisville statement, 2008. Ann Surg. 2009; 250:825–830. DOI: 10.1097/SLA.0b013e3181b3b2d8. PMID: 19916210.6. Wakabayashi G, Cherqui D, Geller DA, Buell JF, Kaneko H, Han HS, et al. 2015; Recommendations for laparoscopic liver resection. Ann Surg. 261:619–629.7. Abu Hilal M, Aldrighetti L, Dagher I, Edwin B, Troisi RI, Alikhanov R, et al. 2018; The southampton consensus guidelines for laparoscopic liver surgery: from indication to implementation. Ann Surg. 268:11–18. DOI: 10.1097/SLA.0000000000002524. PMID: 29064908.8. Cherqui D, Ciria R, Kwon CHD, Kim KH, Broering D, Wakabayashi G, et al. 2021; Expert consensus guidelines on minimally invasive donor hepatectomy for living donor liver transplantation from innovation to implementation: a joint initiative from the International Laparoscopic Liver Society (ILLS) and the Asian-Pacific Hepato-Pancreato- Biliary Association (A-PHPBA). Ann Surg. 273:96–108. DOI: 10.1097/SLA.0000000000004475. PMID: 33332874.9. Suh KS, Hong SK, Lee KW, Yi NJ, Kim HS, Ahn SW, et al. 2018; Pure laparoscopic living donor hepatectomy: focus on 55 donors undergoing right hepatectomy. Am J Transplant. 18:434–443. DOI: 10.1111/ajt.14455. PMID: 28787763.10. Hong SK, Tan MY, Worakitti L, Lee JM, Cho JH, Yi NJ, et al. 2022; Pure laparoscopic versus open right hepatectomy in live liver donors: a propensity score-matched analysis. Ann Surg. 275:e206–e212. DOI: 10.1097/SLA.0000000000003914. PMID: 32324692.11. Hong SK, Kim JY, Lee J, Kim J, Choi HH, Lee S, et al. 2024; Pure laparoscopic donor hepatectomy: experience of 556 cases at Seoul National University Hospital. Am J Transplant. 24:222–238. DOI: 10.1016/j.ajt.2023.06.007. PMID: 37321453.12. Hong SK, Lee KW, Choi Y, Kim HS, Ahn SW, Yoon KC, et al. 2018; Initial experience with purely laparoscopic living-donor right hepatectomy. Br J Surg. 105:751–759. DOI: 10.1002/bjs.10777. PMID: 29579333.13. Lee KW, Hong SK, Suh KS, Kim HS, Ahn SW, Yoon KC, et al. 2018; One hundred and fifteen cases of pure laparoscopic living donor right hepatectomy at a single center. Transplantation. 102:1878–1884. DOI: 10.1097/TP.0000000000002229. PMID: 29684001.14. Cho HD, Samstein B, Chaundry S, Kim KH. 2020; Minimally invasive donor hepatectomy, systemic review. Int J Surg. 82:187–191. DOI: 10.1016/j.ijsu.2020.06.023. PMID: 32615320.15. Rhu J, Choi GS, Kim JM, Kwon CHD, Joh JW. 2022; Complete transition from open surgery to laparoscopy: 8-year experience with more than 500 laparoscopic living donor hepatectomies. Liver Transplant. 28:1158–1172. DOI: 10.1002/lt.26429. PMID: 35138684.16. Hong SK, Choi GS, Han J, Cho HD, Kim JM, Han YS, et al. 2021; Pure laparoscopic donor hepatectomy: a multicenter experience. Liver Transpl. 27:67–76. DOI: 10.1002/lt.25848. PMID: 32679612.17. Lee JG, Lee KW, Kwon CHD, Chu CW, Kim BW, Choi DL, et al. 2017; Donor safety in living donor liver transplantation: the Korean organ transplantation registry study. Liver Transpl. 23:999–1006. DOI: 10.1002/lt.24778. PMID: 28431203.18. Lin JS, Muhammad H, Lin T, Kamel I, Baghdadi A, Rizkalla N, et al. 2023; Donor BMI and post-living donor liver transplantation outcomes: a preliminary report. Transplant Direct. 9:e1431. DOI: 10.1097/TXD.0000000000001431. PMID: 36700065. PMCID: PMC9835892.19. Kwong AJ, Ebel NH, Kim WR, Lake JR, Smith JM, Schladt DP, et al. 2023; OPTN/SRTR 2021 annual data report: liver. Am J Transplant. 23:S178–S263. DOI: 10.1016/j.ajt.2023.02.006. PMID: 37132348.20. Moss J, Lapointe-Rudow D, Renz JF, Kinkhabwala M, Dove LM, Gaglio PJ, et al. 2005; Select utilization of obese donors in living donor liver transplantation: implications for the donor pool. Am J Transplant. 5:2974–2981. DOI: 10.1111/j.1600-6143.2005.01124.x. PMID: 16303013.21. Dirican A, Ozsoy M, Ates M, Ersan V, Gonultas F, Isik B, et al. 2015; Consequences of the use of extended criteria donors in living donor liver transplantation. Ann Transplant. 20:211–217. DOI: 10.12659/AOT.892454. PMID: 25877045.22. Knaak M, Goldaracena N, Doyle A, Cattral MS, Greig PD, Lilly L, et al. 2017; Donor BMI >30 is not a contraindication for live liver donation. Am J Transplant. 17:754–760. DOI: 10.1111/ajt.14019. PMID: 27545327.23. Jin YJ, Kim KM, Hwang S, Lee SG, Ha TY, Song GW, et al. 2012; Exercise and diet modification in non-obese non-alcoholic fatty liver disease: analysis of biopsies of living liver donors. J Gastroenterol Hepatol. 27:1341–1347. DOI: 10.1111/j.1440-1746.2012.07165.x. PMID: 22554085.24. Ryan CK, Johnson LA, Germin BI, Marcos A. 2002; One hundred consecutive hepatic biopsies in the workup of living donors for right lobe liver transplantation. Liver Transpl. 8:1114–1122. DOI: 10.1053/jlts.2002.36740. PMID: 12474149.25. Hong SK, Suh KS, Cho JH, Lee JM, Yi NJ, Lee KW. 2020; Influence of body mass index ≥30 on pure laparoscopic donor right hepatectomy. Ann Transplant. 25:e923094. DOI: 10.12659/AOT.923094.26. Suh KS, Suh SW, Lee JM, Choi Y, Yi NJ, Lee KW. 2015; Recent advancements in and views on the donor operation in living donor liver transplantation: a single-center study of 886 patients over 13 years. Liver Transpl. 21:329–338. DOI: 10.1002/lt.24061. PMID: 25488794.27. Nugroho A, Kim OK, Lee KW, Song S, Kim H, Hong SK, et al. 2017; Evaluation of donor workups and exclusions in a single-center experience of living donor liver transplantation. Liver Transpl. 23:614–624. DOI: 10.1002/lt.24762. PMID: 28294533.28. Suh KS, Hong SK, Yi NJ, Lee KW, Kim HS, Yoon KC, et al. 2016; Pure 3-dimensional laparoscopic extended right hepatectomy in a living donor. Liver Transpl. 22:1431–1436. DOI: 10.1002/lt.24504. PMID: 27347847.29. Hong SK, Suh KS, Yoon KC, Lee JM, Cho JH, Yi NJ, et al. 2019; The learning curve in pure laparoscopic donor right hepatectomy: a cumulative sum analysis. Surg Endosc. 33:3741–3748. DOI: 10.1007/s00464-019-06668-3. PMID: 30771071.30. Yi NJ, Suh KS, Suh SW, Chang YR, Hong G, Yoo T, et al. 2013; Excellent outcome in 238 consecutive living donor liver transplantations using the right liver graft in a large volume single center. World J Surg. 37:1419–1429. DOI: 10.1007/s00268-013-1976-y. PMID: 23467924.31. Hong SK, Lee KW, Kim HS, Yoon KC, Ahn SW, Choi JY, et al. 2017; Optimal bile duct division using real-time indocyanine green near-infrared fluorescence cholangiography during laparoscopic donor hepatectomy. Liver Transpl. 23:847–852. DOI: 10.1002/lt.24686. PMID: 27935193.32. Kim J, Hong SK, Lim J, Lee JM, Cho JH, Choi Y, et al. 2021; Demarcating the exact midplane of the liver using indocyanine green near-infrared fluorescence imaging during laparoscopic donor hepatectomy. Liver Transpl. 27:830–839. DOI: 10.1002/lt.26019. PMID: 33583130.33. Lapisatepun W, Hong SK, Hong K, Han ES, Lee JM, Yi NJ, et al. 2021; Influence of large grafts weighing ≥ 1000 g on outcome of pure laparoscopic donor right hepatectomy. J Gastrointest Surg. 25:1980–1988. DOI: 10.1007/s11605-020-04837-7. PMID: 33104954.34. Tjeertes EK, Hoeks SE, Beks SB, Valentijn TM, Hoofwijk AG, Stolker RJ. 2015; Obesity--a risk factor for postoperative complications in general surgery? BMC Anesthesiol. 15:112. DOI: 10.1186/s12871-015-0096-7. PMID: 26228844. PMCID: PMC4520073.35. Bergqvist D. 2007; Risk of venous thromboembolism in patients undergoing cancer surgery and options for thromboprophylaxis. J Surg Oncol. 95:167–174. DOI: 10.1002/jso.20625. PMID: 17262765.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Single Center Experience for a Feasibility of Totally Laparoscopic Living Donor Right Hepatectomy
- The outcomes of pure laparoscopic living donor hepatectomy at small volume center
- Pure laparoscopic donor right hepatectomy for adult living donor liver transplantation: initial report from Southeast Asia liver transplant center
- Safety of pure laparoscopic donor hepatectomy for adult living donor liver transplant: comparison with laparoscopic non-donor hepatectomy
- Pure laparoscopic hepatectomy and robotic graft implantation in living donor liver transplantation: a case report