Int J Stem Cells.
2024 Aug;17(3):236-252. 10.15283/ijsc23092.
The Role of Exosomes from Mesenchymal Stem Cells in Spinal Cord Injury: A Systematic Review
- Affiliations
-
- 1Department of Neurology, Affiliated Hospital of Jining Medical University, Jining Medical University, Jining, China
- 2Department of Reproduce, Affiliated Hospital of Jining Medical University, Jining Medical University, Jining, China
- 3Department of Gastrointestinal Surgery, Affiliated Hospital of Jining Medical University, Jining Medical University, Jining, China
- 4Institute of Forensic Medicine and Laboratory Medicine, Jining Medical University, Jining, China
- KMID: 2558603
- DOI: http://doi.org/10.15283/ijsc23092
Abstract
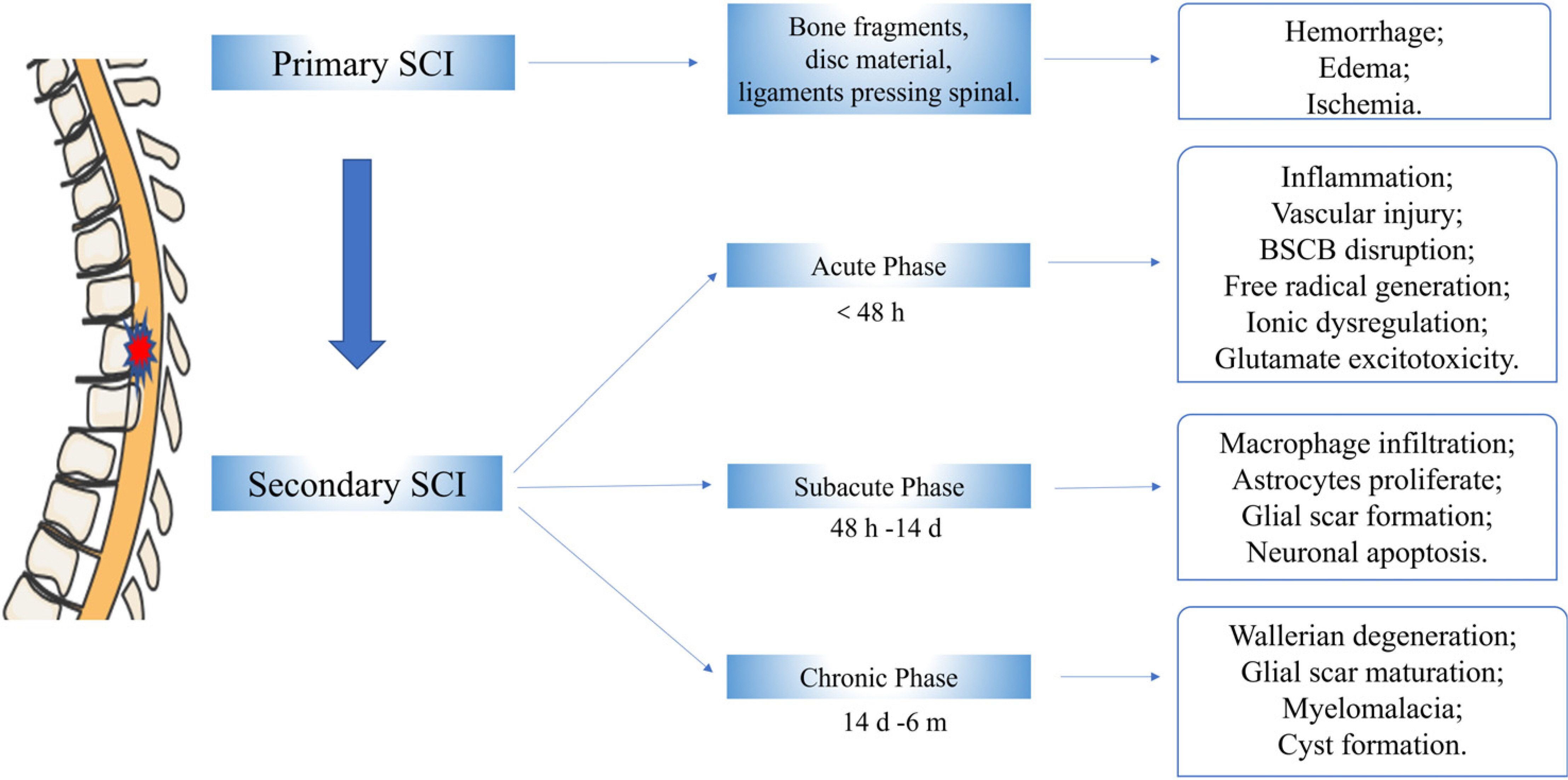
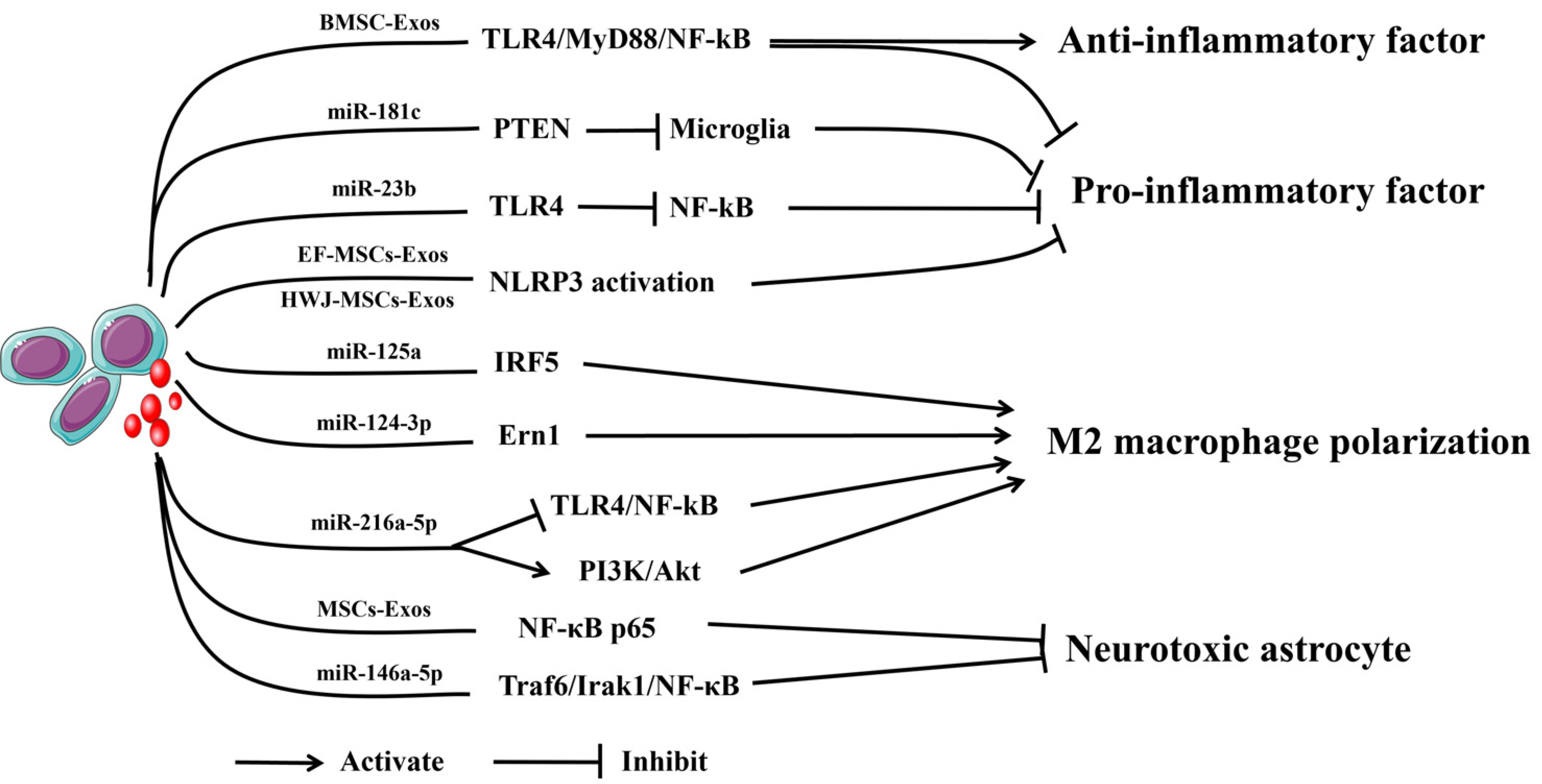
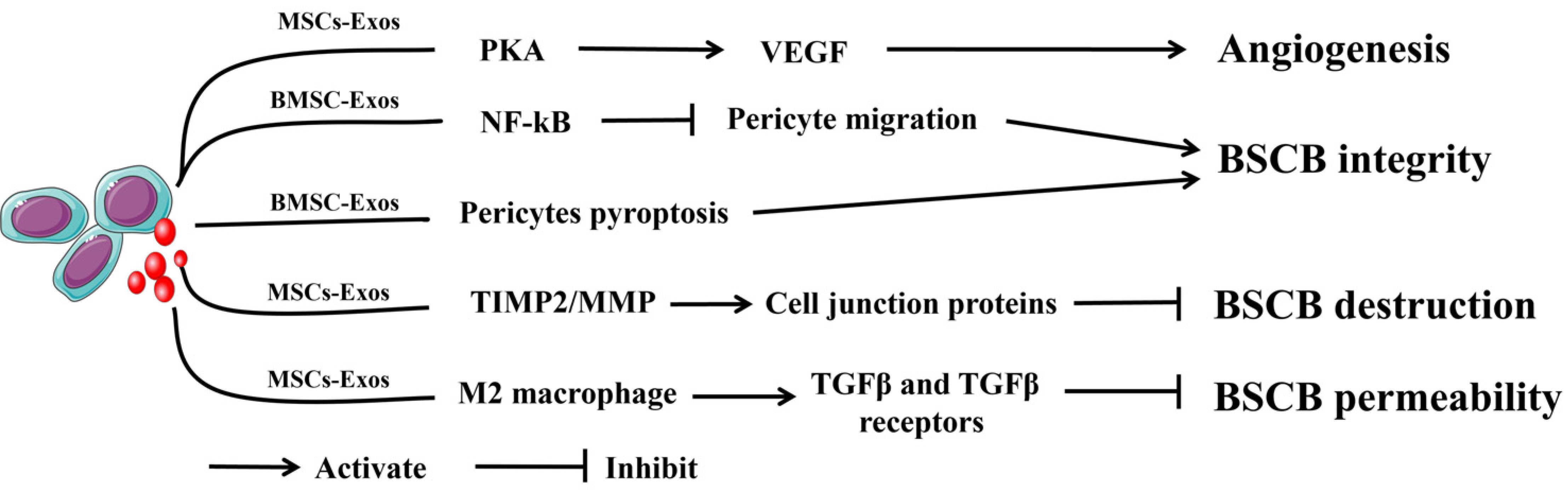
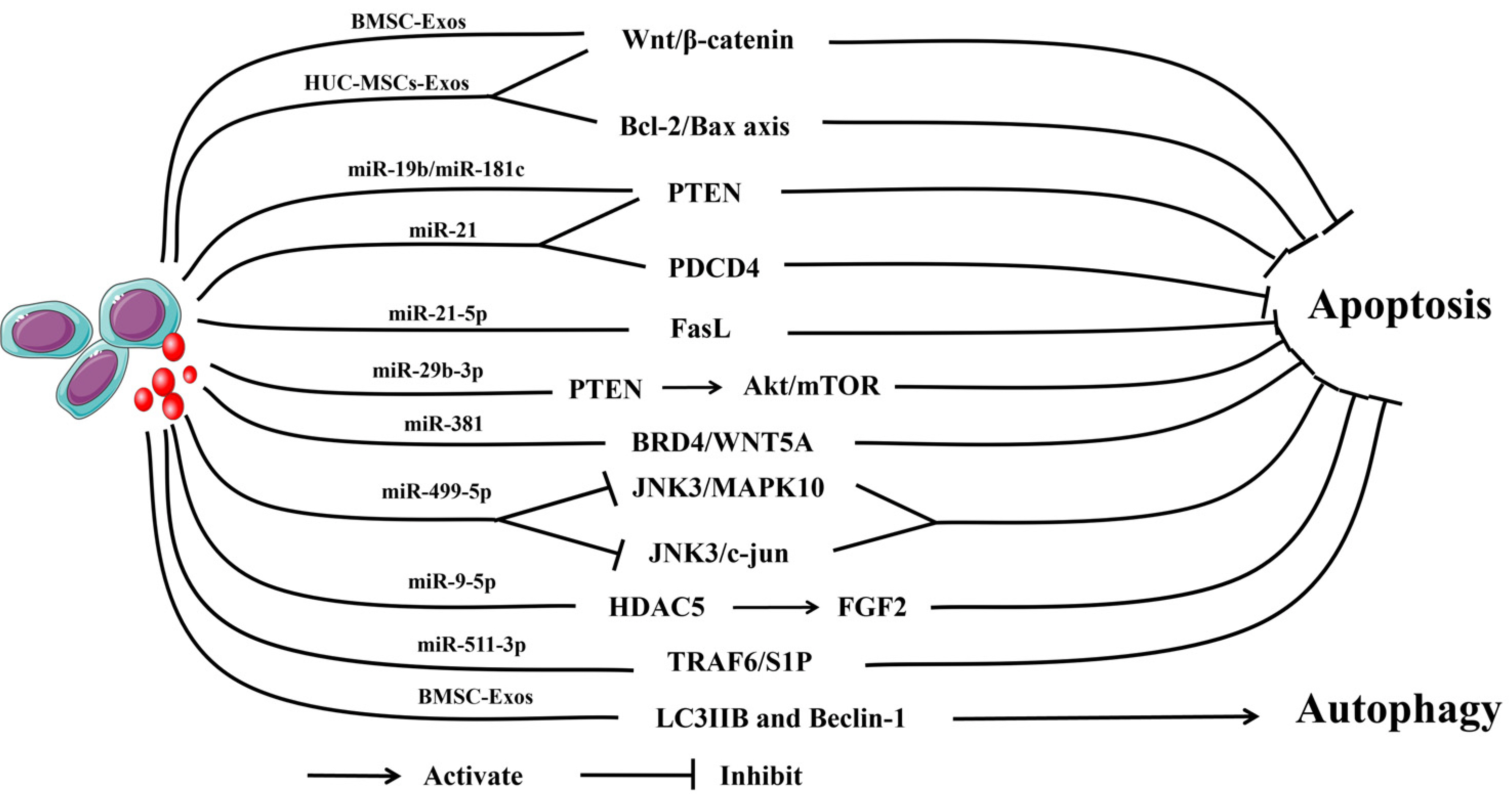
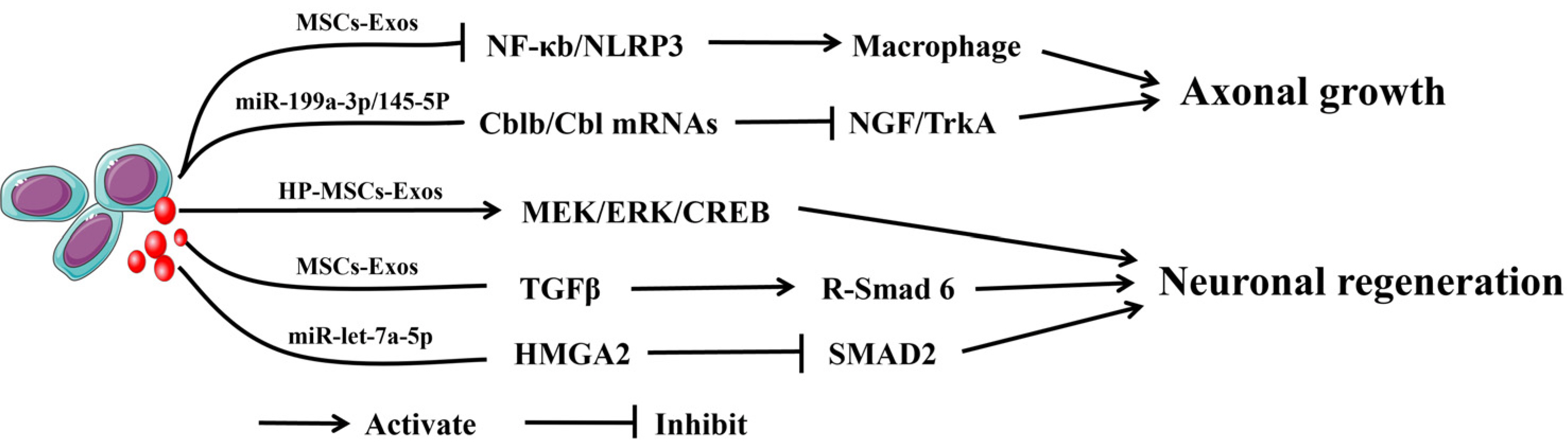
- Spinal cord injury (SCI) is a serious nervous system disease that usually leads to the impairment of the motor, sensory, and autonomic nervous functions of the spinal cord, and it places a heavy burden on families and healthcare systems every year. Due to the complex pathophysiological mechanism of SCI and the poor ability of neurons to regenerate, the current treatment scheme has very limited effects on the recovery of spinal cord function. In addition, due to their unique advantages, exosomes can be used as carriers for cargo transport. In recent years, some studies have confirmed that treatment with mesenchymal stem cells (MSCs) can promote the recovery of SCI nerve function. The therapeutic effect of MSCs is mainly related to exosomes secreted by MSCs, and exosomes may have great potential in SCI therapy. In this review, we summarized the repair mechanism of mesenchymal stem cells-derived exosomes (MSCs-Exos) in SCI treatment and discussed the microRNAs related to SCI treatment based on MSCs-Exos and their mechanism of action, which is helpful to further understand the role of exosomes in SCI.
Figure
Reference
-
References
1. GBD 2016 Traumatic Brain Injury and Spinal Cord Injury Collaborators. 2019; Global, regional, and national burden of traumatic brain injury and spinal cord injury, 1990-2016: a systematic analysis for the Global Burden of Disease Study 2016. Lancet Neurol. 18:56–87. Erratum in: Lancet Neurol 2021;20:e7. DOI: 10.3410/f.734500777.793573250. PMID: 30497965. PMCID: PMC6291456.2. GBD 2016 Neurology Collaborators. Global, regional, and national burden of neurological disorders, 1990-2016: a systematic analysis for the Global Burden of Disease Study 2016. Lancet Neurol. 18:459–480. DOI: 10.3410/f.735346535.793561284. PMID: 30879893. PMCID: PMC6459001.3. Singh A, Tetreault L, Kalsi-Ryan S, Nouri A, Fehlings MG. 2014; Global prevalence and incidence of traumatic spinal cord injury. Clin Epidemiol. 6:309–331. DOI: 10.2147/clep.s68889. PMID: 25278785. PMCID: PMC4179833.4. Eli I, Lerner DP, Ghogawala Z. 2021; Acute traumatic spinal cord injury. Neurol Clin. 39:471–488. DOI: 10.1016/j.ncl.2021.02.004. PMID: 33896529.5. Feigin VL, Vos T, Alahdab F, et al. 2021; Burden of neurological disorders across the US from 1990-2017: a global burden of disease study. JAMA Neurol. 78:165–176. DOI: 10.1001/jamaneurol.2020.4152. PMID: 33136137. PMCID: PMC7607495.6. Islam MS, Harvey LA, Hossain MS, et al. 2021; The cost of providing a community-based model of care to people with spinal cord injury, and the healthcare costs and economic burden to households of spinal cord injury in Bangladesh. Spinal Cord. 59:833–841. DOI: 10.1038/s41393-020-00600-6. PMID: 33495581.7. Bracken MB. 2012; Steroids for acute spinal cord injury. Cochrane Database Syst Rev. 1:CD001046. DOI: 10.1002/14651858.cd001046.pub2. PMID: 22258943. PMCID: PMC6513405.8. Rath N, Balain B. 2017; Spinal cord injury-the role of surgical treatment for neurological improvement. J Clin Orthop Trauma. 8:99–102. DOI: 10.1016/j.jcot.2017.06.016. PMID: 28720984. PMCID: PMC5498753.9. Wutte C, Klein B, Becker J, et al. 2019; Earlier decompression (< 8 hours) results in better neurological and functional outcome after traumatic thoracolumbar spinal cord injury. J Neurotrauma. 36:2020–2027. DOI: 10.1089/neu.2018.6146. PMID: 30489193.10. Zhang Y, Al Mamun A, Yuan Y, et al. 2021; Acute spinal cord injury: pathophysiology and pharmacological intervention (Re-view). Mol Med Rep. 23:417. DOI: 10.3892/mmr.2021.12056. PMID: 33846780. PMCID: PMC8025476.11. Silvestro S, Bramanti P, Trubiani O, Mazzon E. 2020; Stem cells therapy for spinal cord injury: an overview of clinical trials. Int J Mol Sci. 21:659. DOI: 10.3390/ijms21020659. PMID: 31963888. PMCID: PMC7013533.12. Berebichez-Fridman R, Montero-Olvera PR. 2018; Sources and clinical applications of mesenchymal stem cells: state-of-the-art review. Sultan Qaboos Univ Med J. 18:e264–e277. DOI: 10.18295/squmj.2018.18.03.002. PMID: 30607265. PMCID: PMC6307657.13. Brown C, McKee C, Bakshi S, et al. 2019; Mesenchymal stem cells: cell therapy and regeneration potential. J Tissue Eng Regen Med. 13:1738–1755. DOI: 10.1002/term.2914. PMID: 31216380.14. Musiał-Wysocka A, Kot M, Majka M. 2019; The pros and cons of mesenchymal stem cell-based therapies. Cell Transplant. 28:801–812. DOI: 10.1177/0963689719837897. PMID: 31018669. PMCID: PMC6719501.15. Qiu G, Zheng G, Ge M, et al. 2019; Functional proteins of mesenchymal stem cell-derived extracellular vesicles. Stem Cell Res Ther. 10:359. DOI: 10.1186/s13287-019-1484-6. PMID: 31779700. PMCID: PMC6883709.16. Romanelli P, Bieler L, Scharler C, et al. 2019; Extracellular vesicles can deliver anti-inflammatory and anti-scarring activities of mesenchymal stromal cells after spinal cord injury. Front Neurol. 10:1225. DOI: 10.3389/fneur.2019.01225. PMID: 31849808. PMCID: PMC6896947.17. Qiu G, Zheng G, Ge M, et al. 2018; Mesenchymal stem cell-derived extracellular vesicles affect disease outcomes via tra-nsfer of microRNAs. Stem Cell Res Ther. 9:320. DOI: 10.1186/s13287-018-1069-9. PMID: 30463593. PMCID: PMC6249826.18. Guo XD, He XG, Yang FG, et al. 2021; Research progress on the regulatory role of microRNAs in spinal cord injury. Regen Med. 16:465–476. DOI: 10.2217/rme-2020-0125. PMID: 33955796.19. Quinzaños-Fresnedo J, Sahagún-Olmos RC. 2015; Micro RNA and its role in the pathophysiology of spinal cord injury - a further step towards neuroregenerative medicine. Cir Cir. 83:442–447. Spanish. DOI: 10.2217/rme-2020-0125. PMID: 26162489.20. Yuan J, Botchway BOA, Zhang Y, Wang X, Liu X. 2020; Role of circular ribonucleic acids in the treatment of traumatic brain and spinal cord injury. Mol Neurobiol. 57:4296–4304. DOI: 10.1007/s12035-020-02027-9. PMID: 32700251.21. Lima R, Monteiro A, Salgado AJ, Monteiro S, Silva NA. 2022; Pathophysiology and therapeutic approaches for spinal cord injury. Int J Mol Sci. 23:13833. DOI: 10.3390/ijms232213833. PMID: 36430308. PMCID: PMC9698625.22. McDonald JW, Sadowsky C. 2002; Spinal-cord injury. Lancet. 359:417–425. DOI: 10.1016/s0140-6736(02)07603-1. PMID: 11844532.23. Sekhon LH, Fehlings MG. 2001; Epidemiology, demographics, and pathophysiology of acute spinal cord injury. Spine (Phila Pa 1976). 26(24 Suppl):S2–S12. DOI: 10.1097/00007632-200112151-00002. PMID: 11805601.24. Young W. 1993; Secondary injury mechanisms in acute spinal cord injury. J Emerg Med. 11 Suppl 1:13–22. PMID: 8445198.25. Rowland JW, Hawryluk GW, Kwon B, Fehlings MG. 2008; Cur-rent status of acute spinal cord injury pathophysiology and emerging therapies: promise on the horizon. Neurosurg Focus. 25:E2. DOI: 10.3171/FOC.2008.25.11.E2. PMID: 18980476.26. Tran AP, Warren PM, Silver J. 2018; The biology of regeneration failure and success after spinal cord injury. Physiol Rev. 98:881–917. DOI: 10.1152/physrev.00017.2017. PMID: 29513146. PMCID: PMC5966716.27. Alizadeh A, Dyck SM, Karimi-Abdolrezaee S. 2019; Traumatic spinal cord injury: an overview of pathophysiology, models and acute injury mechanisms. Front Neurol. 10:282. DOI: 10.3389/fneur.2019.00282. PMID: 30967837. PMCID: PMC6439316.28. Venkatesh K, Ghosh SK, Mullick M, Manivasagam G, Sen D. 2019; Spinal cord injury: pathophysiology, treatment strategies, associated challenges, and future implications. Cell Tissue Res. 377:125–151. DOI: 10.1007/s00441-019-03039-1. PMID: 31065801.29. Cocucci E, Meldolesi J. 2015; Ectosomes and exosomes: shedding the confusion between extracellular vesicles. Trends Cell Biol. 25:364–372. DOI: 10.1016/j.tcb.2015.01.004. PMID: 25683921.30. Jeppesen DK, Zhang Q, Franklin JL, Coffey RJ. 2023; Extrace-llular vesicles and nanoparticles: emerging complexities. Trends Cell Biol. 33:667–681. DOI: 10.1016/j.tcb.2023.01.002. PMID: 36737375. PMCID: PMC10363204.31. Kalluri R, LeBleu VS. 2020; The biology, function, and biomedi-cal applications of exosomes. Science. 367:eaau6977. DOI: 10.1126/science.aau6977,. PMID: 32029601. PMCID: PMC7717626.32. Caby MP, Lankar D, Vincendeau-Scherrer C, Raposo G, Bonnerot C. 2005; Exosomal-like vesicles are present in human blood plasma. Int Immunol. 17:879–887. DOI: 10.1093/intimm/dxh267. PMID: 15908444.33. Pisitkun T, Shen RF, Knepper MA. 2004; Identification and proteomic profiling of exosomes in human urine. Proc Natl Acad Sci U S A. 101:13368–13373.34. Keller S, Ridinger J, Rupp AK, Janssen JW, Altevogt P. 2011; Body fluid derived exosomes as a novel template for clinical diagnostics. J Transl Med. 9:86. DOI: 10.1186/1479-5876-9-86. PMID: 21651777. PMCID: PMC3118335.35. Zhang Y, Yu M, Tian W. 2016; Physiological and pathological impact of exosomes of adipose tissue. Cell Prolif. 49:3–13. DOI: 10.1111/cpr.12233. PMID: 26776755. PMCID: PMC6496788.36. Kowal J, Tkach M, Théry C. 2014; Biogenesis and secretion of exosomes. Curr Opin Cell Biol. 29:116–125. DOI: 10.1016/j.ceb.2014.05.004. PMID: 24959705.37. Colombo M, Moita C, van Niel G, et al. 2013; Analysis of ESCRT functions in exosome biogenesis, composition and secretion highlights the heterogeneity of extracellular vesicles. J Cell Sci. 126(Pt 24):5553–5565. DOI: 10.1242/jcs.128868. PMID: 24105262.38. Stuffers S, Sem Wegner C, Stenmark H, Brech A. 2009; Multive-sicular endosome biogenesis in the absence of ESCRTs. Traffic. 10:925–937. DOI: 10.1111/j.1600-0854.2009.00920.x. PMID: 19490536.39. van Niel G, Charrin S, Simoes S, et al. 2011; The tetraspanin CD63 regulates ESCRT-independent and -dependent endosomal sorting during melanogenesis. Dev Cell. 21:708–721. DOI: 10.1016/j.devcel.2011.08.019. PMID: 21962903. PMCID: PMC3199340.40. Mathieu M, Martin-Jaular L, Lavieu G, Théry C. 2019; Specifi-cities of secretion and uptake of exosomes and other extra-cellular vesicles for cell-to-cell communication. Nat Cell Biol. 21:9–17. DOI: 10.1038/s41556-018-0250-9. PMID: 30602770.41. Xunian Z, Kalluri R. 2020; Biology and therapeutic potential of mesenchymal stem cell-derived exosomes. Cancer Sci. 111:3100–3110. DOI: 10.1111/cas.14563. PMID: 32639675. PMCID: PMC7469857.42. Zhang Y, Liu Y, Liu H, Tang WH. 2019; Exosomes: biogenesis, biologic function and clinical potential. Cell Biosci. 9:19. DOI: 10.1186/s13578-019-0282-2. PMID: 30815248. PMCID: PMC6377728.43. Mendt M, Rezvani K, Shpall E. 2019; Mesenchymal stem cell-derived exosomes for clinical use. Bone Marrow Transplant. 54(Suppl 2):789–792. DOI: 10.1038/s41409-019-0616-z. PMID: 31431712.44. L Ramos T, Sánchez-Abarca LI, Muntión S, et al. 2016; MSC surface markers (CD44, CD73, and CD90) can identify human MSC-derived extracellular vesicles by conventional flow cyto-metry. Cell Commun Signal. 14:2. DOI: 10.1186/s12964-015-0124-8. PMID: 26754424. PMCID: PMC4709865.45. Heldring N, Mäger I, Wood MJ, Le Blanc K, Andaloussi SE. 2015; Therapeutic potential of multipotent mesenchymal stromal cells and their extracellular vesicles. Hum Gene Ther. 26:506–517. DOI: 10.1089/hum.2015.072. PMID: 26153722.46. Yang C, Guo WB, Zhang WS, et al. 2017; Comprehensive proteomics analysis of exosomes derived from human seminal plasma. Andrology. 5:1007–1015. DOI: 10.1111/andr.12412. PMID: 28914500. PMCID: PMC5639412.47. Kim HS, Choi DY, Yun SJ, et al. 2012; Proteomic analysis of microvesicles derived from human mesenchymal stem cells. J Proteome Res. 11:839–849. DOI: 10.1021/pr200682z. PMID: 22148876.48. Liang Y, Duan L, Lu J, Xia J. 2021; Engineering exosomes for targeted drug delivery. Theranostics. 11:3183–3195. DOI: 10.7150/thno.52570. PMID: 33537081. PMCID: PMC7847680.49. Bartel DP. 2004; MicroRNAs: genomics, biogenesis, mechanism, and function. Cell. 116:281–297. DOI: 10.1016/s0092-8674(04)00045-5. PMID: 14744438.50. Filipowicz W, Bhattacharyya SN, Sonenberg N. 2008; Mechanisms of post-transcriptional regulation by microRNAs: are the answers in sight? Nat Rev Genet. 9:102–114. DOI: 10.1038/nrg2290. PMID: 18197166.51. Winter J, Jung S, Keller S, Gregory RI, Diederichs S. 2009; Many roads to maturity: microRNA biogenesis pathways and their regulation. Nat Cell Biol. 11:228–234. DOI: 10.1038/ncb0309-228. PMID: 19255566.52. Tüfekci KU, Meuwissen RL, Genç S. 2014; The role of microRNAs in biological processes. Methods Mol Biol. 1107:15–31. DOI: 10.1007/978-1-62703-748-8_2. PMID: 24272429.53. Wiklander OPB, Brennan MÁ, Lötvall J, Breakefield XO, El Andaloussi S. 2019; Advances in therapeutic applications of extracellular vesicles. Sci Transl Med. 11:eaav8521. DOI: 10.1126/scitranslmed.aav8521. PMID: 31092696. PMCID: PMC7104415.54. Fan B, Wei Z, Yao X, et al. 2018; Microenvironment imbalance of spinal cord injury. Cell Transplant. 27:853–866. DOI: 10.1177/0963689718755778. PMID: 29871522. PMCID: PMC6050904.55. Liu X, Zhang Y, Wang Y, Qian T. 2021; Inflammatory response to spinal cord injury and its treatment. World Neurosurg. 155:19–31. DOI: 10.1016/j.wneu.2021.07.148. PMID: 34375779.56. Hellenbrand DJ, Quinn CM, Piper ZJ, Morehouse CN, Fixel JA, Hanna AS. 2021; Inflammation after spinal cord injury: a review of the critical timeline of signaling cues and cellular infiltration. J Neuroinflammation. 18:284. DOI: 10.1186/s12974-021-02337-2. PMID: 34876174. PMCID: PMC8653609.57. Fan L, Dong J, He X, Zhang C, Zhang T. 2021; Bone marrow mesenchymal stem cells-derived exosomes reduce apoptosis and inflammatory response during spinal cord injury by inhibiting the TLR4/MyD88/NF-κB signaling pathway. Hum Exp Toxicol. 40:1612–1623. DOI: 10.1177/09603271211003311. PMID: 33779331.58. Zhang M, Wang L, Huang S, He X. 2021; Exosomes with high level of miR-181c from bone marrow-derived mesenchymal stem cells inhibit inflammation and apoptosis to alleviate spinal cord injury. J Mol Histol. 52:301–311. DOI: 10.1007/s10735-020-09950-0. PMID: 33548000.59. Nie H, Jiang Z. 2021; Bone mesenchymal stem cell-derived extracellular vesicles deliver microRNA-23b to alleviate spinal cord injury by targeting toll-like receptor TLR4 and inhibiting NF-κB pathway activation. Bioengineered. 12:8157–8172. DOI: 10.1080/21655979.2021.1977562. PMID: 34663169. PMCID: PMC8806461.60. Sung SE, Seo MS, Kim YI, et al. 2022; Human epidural AD-MSC exosomes improve function recovery after spinal cord injury in rats. Biomedicines. 10:678. DOI: 10.3390/biomedicines10030678. PMID: 35327480. PMCID: PMC8945172.61. Zhou K, Shi L, Wang Y, Chen S, Zhang J. 2016; Recent advances of the NLRP3 inflammasome in central nervous system disorders. J Immunol Res. 2016:9238290. DOI: 10.1155/2016/9238290. PMID: 27652274. PMCID: PMC5019917.62. Zhou C, Zheng J, Fan Y, Wu J. 2022; TI: NLRP3 inflammasome-dependent pyroptosis in CNS trauma: a potential therapeu-tic target. Front Cell Dev Biol. 10:821225. DOI: 10.3389/fcell.2022.821225. PMID: 35186932. PMCID: PMC8847380.63. Rathinam VA, Fitzgerald KA. 2016; Inflammasome complexes: emerging mechanisms and effector functions. Cell. 165:792–800. DOI: 10.1016/j.cell.2016.03.046. PMID: 27153493. PMCID: PMC5503689.64. Chen J, Shen Y, Shao X, Wu W. 2023; An emerging role of inflammasomes in spinal cord injury and spinal cord tumor. Front Immunol. 14:1119591. DOI: 10.3389/fimmu.2023.1119591. PMID: 36969234. PMCID: PMC10033975.65. Majidpoor J, Khezri Z, Rostamzadeh P, et al. 2020; The expre-ssions of NLRP1, NLRP3, and AIM2 inflammasome complexes in the contusive spinal cord injury rat model and their responses to hormonal therapy. Cell Tissue Res. 381:397–410. DOI: 10.1007/s00441-020-03250-5. PMID: 32696217.66. Jiang W, Li M, He F, Zhou S, Zhu L. 2017; Targeting the NLRP3 inflammasome to attenuate spinal cord injury in mice. J Neuroinflammation. 14:207. DOI: 10.1186/s12974-017-0980-9. PMID: 29070054. PMCID: PMC5657095.67. Zhang M, Wang L, Huang S, He X. 2020; MicroRNA-223 targets NLRP3 to relieve inflammation and alleviate spinal cord injury. Life Sci. 254:117796. DOI: 10.1016/j.lfs.2020.117796. PMID: 32417375.68. Dai C, Liu B, Peng B, et al. 2021; Entinostat improves motor function and neuronal damage via downregulating NLRP3 inflammasome activation after spinal cord injury. Front Pharmacol. 12:774539. DOI: 10.3389/fphar.2021.774539. PMID: 34899337. PMCID: PMC8664236.69. Noonin C, Thongboonkerd V. 2021; Exosome-inflammasome crosstalk and their roles in inflammatory responses. Theranostics. 11:4436–4451. DOI: 10.7150/thno.54004. PMID: 33754070. PMCID: PMC7977448.70. Huang JH, Fu CH, Xu Y, Yin XM, Cao Y, Lin FY. 2020; Extra-cellular vesicles derived from epidural fat-mesenchymal stem cells attenuate NLRP3 inflammasome activation and improve functional recovery after spinal cord injury. Neu-rochem Res. 45:760–771. DOI: 10.1007/s11064-019-02950-x. PMID: 31953741.71. Noori L, Arabzadeh S, Mohamadi Y, et al. 2021; Intrathecal administration of the extracellular vesicles derived from human Wharton's jelly stem cells inhibit inflammation and attenuate the activity of inflammasome complexes after spinal cord injury in rats. Neurosci Res. 170:87–98. DOI: 10.1016/j.neures.2020.07.011. PMID: 32717259.72. Ginhoux F, Prinz M. 2015; Origin of microglia: current concepts and past controversies. Cold Spring Harb Perspect Biol. 7:a020537. DOI: 10.1101/cshperspect.a020537. PMID: 26134003. PMCID: PMC4526747.73. Alliot F, Godin I, Pessac B. 1999; Microglia derive from progenitors, originating from the yolk sac, and which proliferate in the brain. Brain Res Dev Brain Res. 117:145–152. DOI: 10.1016/s0165-3806(99)00113-3. PMID: 10567732.74. Epelman S, Lavine KJ, Randolph GJ. 2014; Origin and functions of tissue macrophages. Immunity. 41:21–35. DOI: 10.1016/j.immuni.2014.06.013. PMID: 25035951. PMCID: PMC4470379.75. Zhou X, He X, Ren Y. 2014; Function of microglia and macrophages in secondary damage after spinal cord injury. Neural Regen Res. 9:1787–1795. DOI: 10.4103/1673-5374.143423. PMID: 25422640. PMCID: PMC4239768.76. David S, Kroner A. 2011; Repertoire of microglial and macrophage responses after spinal cord injury. Nat Rev Neurosci. 12:388–399. DOI: 10.1038/nrn3053. PMID: 21673720.77. Devanney NA, Stewart AN, Gensel JC. 2020; Microglia and macrophage metabolism in CNS injury and disease: the role of immunometabolism in neurodegeneration and neuro-trauma. Exp Neurol. 329:113310. DOI: 10.1016/j.expneurol.2020.113310. PMID: 32289316. PMCID: PMC7237336.78. Martinez FO, Gordon S. 2014; The M1 and M2 paradigm of macrophage activation: time for reassessment. F1000Prime Rep. 6:13. DOI: 10.12703/p6-13. PMID: 24669294. PMCID: PMC3944738.79. Kigerl KA, Gensel JC, Ankeny DP, Alexander JK, Donnelly DJ, Popovich PG. 2009; Identification of two distinct macrophage subsets with divergent effects causing either neurotoxicity or regeneration in the injured mouse spinal cord. J Neuro-sci. 29:13435–13444. DOI: 10.1523/jneurosci.3257-09.2009. PMID: 19864556. PMCID: PMC2788152.80. Chang Q, Hao Y, Wang Y, Zhou Y, Zhuo H, Zhao G. 2021; Bone marrow mesenchymal stem cell-derived exosomal microRNA-125a promotes M2 macrophage polarization in spinal cord injury by downregulating IRF5. Brain Res Bull. 170:199–210. DOI: 10.1016/j.brainresbull.2021.02.015. PMID: 33609602.81. Li R, Zhao K, Ruan Q, Meng C, Yin F. 2020; Bone marrow mesenchymal stem cell-derived exosomal microRNA-124-3p attenuates neurological damage in spinal cord ischemia-reperfusion injury by downregulating Ern1 and promoting M2 macrophage polarization. Arthritis Res Ther. 22:75. DOI: 10.1186/s13075-020-2146-x. PMID: 32272965. PMCID: PMC7146970.82. Liu W, Rong Y, Wang J, et al. 2020; Exosome-shuttled miR-216a-5p from hypoxic preconditioned mesenchymal stem cells repair traumatic spinal cord injury by shifting microglial M1/M2 polarization. J Neuroinflammation. 17:47. DOI: 10.1186/s12974-020-1726-7. PMID: 32019561. PMCID: PMC7001326.83. Liu C, Hu F, Jiao G, et al. 2022; Dental pulp stem cell-derived exosomes suppress M1 macrophage polarization through the ROS-MAPK-NFκB P65 signaling pathway after spinal cord injury. J Nanobiotechnology. 20:65. DOI: 10.1186/s12951-022-01273-4. PMID: 35109874. PMCID: PMC8811988.84. Sofroniew MV. 2014; Astrogliosis. Cold Spring Harb Perspect Biol. 7:a020420. DOI: 10.1101/cshperspect.a020420. PMID: 25380660. PMCID: PMC4315924.85. Sofroniew MV, Vinters HV. 2010; Astrocytes: biology and patho-logy. Acta Neuropathol. 119:7–35. DOI: 10.1007/s00401-009-0619-8. PMID: 20012068. PMCID: PMC2799634.86. Liddelow SA, Guttenplan KA, Clarke LE, et al. 2017; Neurotoxic reactive astrocytes are induced by activated microglia. Nature. 541:481–487. DOI: 10.3410/f.727217936.793528237. PMID: 28099414. PMCID: PMC5404890.87. Liddelow SA, Barres BA. 2017; Reactive astrocytes: production, function, and therapeutic potential. Immunity. 46:957–967. DOI: 10.1016/j.immuni.2017.06.006. PMID: 28636962.88. Wang L, Pei S, Han L, et al. 2018; Mesenchymal stem cell-deri-ved exosomes reduce A1 astrocytes via downregulation of phosphorylated NFκB P65 subunit in spinal cord injury. Cell Physiol Biochem. 50:1535–1559. DOI: 10.1159/000494652. PMID: 30376671.89. Liu W, Wang Y, Gong F, et al. 2019; Exosomes derived from bone mesenchymal stem cells repair traumatic spinal cord injury by suppressing the activation of A1 neurotoxic reactive astro-cytes. J Neurotrauma. 36:469–484. DOI: 10.1089/neu.2018.5835. PMID: 29848167.90. Lai X, Wang Y, Wang X, Liu B, Rong L. 2022; miR-146a-5p-modified hUCMSC-derived exosomes facilitate spinal cord function recovery by targeting neurotoxic astrocytes. Stem Cell Res Ther. 13:487. DOI: 10.1186/s13287-022-03116-3. PMID: 36175984. PMCID: PMC9524140.91. Adams RH, Eichmann A. 2010; Axon guidance molecules in vascular patterning. Cold Spring Harb Perspect Biol. 2:a001875. DOI: 10.1101/cshperspect.a001875. PMID: 20452960. PMCID: PMC2857165.92. Himmels P, Paredes I, Adler H, et al. 2017; Motor neurons control blood vessel patterning in the developing spinal cord. Nat Commun. 8:14583. DOI: 10.1038/ncomms14583. PMID: 28262664. PMCID: PMC5343469.93. Oudega M. 2012; Molecular and cellular mechanisms underlying the role of blood vessels in spinal cord injury and repair. Cell Tissue Res. 349:269–288. DOI: 10.1007/s00441-012-1440-6. PMID: 22592628.94. Losey P, Young C, Krimholtz E, Bordet R, Anthony DC. 2014; The role of hemorrhage following spinal-cord injury. Brain Res. 1569:9–18. DOI: 10.1016/j.brainres.2014.04.033. PMID: 24792308.95. Tsivelekas K, Evangelopoulos DS, Pallis D, et al. 2022; Angio-genesis in spinal cord injury: progress and treatment. Cureus. 14:e25475. DOI: 10.7759/cureus.25475. PMID: 35800787. PMCID: PMC9246426.96. Zhang C, Zhang C, Xu Y, Li C, Cao Y, Li P. 2020; Exosomes derived from human placenta-derived mesenchymal stem cells improve neurologic function by promoting angiogenesis after spinal cord injury. Neurosci Lett. 739:135399. DOI: 10.1016/j.neulet.2020.135399. PMID: 32979457.97. Xue C, Shen Y, Li X, et al. 2018; Exosomes derived from hypoxia-treated human adipose mesenchymal stem cells enhance angiogenesis through the PKA signaling pathway. Stem Cells Dev. 27:456–465. DOI: 10.1089/scd.2017.0296. PMID: 29415626.98. Mu J, Li L, Wu J, et al. 2022; Hypoxia-stimulated mesenchymal stem cell-derived exosomes loaded by adhesive hydrogel for effective angiogenic treatment of spinal cord injury. Biomater Sci. 10:1803–1811. DOI: 10.1039/d1bm01722e. PMID: 35234220.99. Zhong D, Cao Y, Li CJ, et al. 2020; Neural stem cell-derived exosomes facilitate spinal cord functional recovery after injury by promoting angiogenesis. Exp Biol Med (Maywood). 245:54–65. DOI: 10.1177/1535370219895491. PMID: 31903774. PMCID: PMC6987743.100. Luo Z, Peng W, Xu Y, et al. 2021; Exosomal OTULIN from M2 macrophages promotes the recovery of spinal cord injuries via stimulating Wnt/β-catenin pathway-mediated vascular regeneration. Acta Biomater. 136:519–532. DOI: 10.1016/j.actbio.2021.09.026. PMID: 34551329.101. Peng W, Wan L, Luo Z, et al. 2021; Microglia-derived exosomes improve spinal cord functional recovery after injury via inhibiting oxidative stress and promoting the survival and function of endothelia cells. Oxid Med Cell Longev. 2021:1695087. DOI: 10.1155/2021/1695087. PMID: 34484559. PMCID: PMC8413072.102. Huang JH, Chen YN, He H, Fu CH, Xu ZY, Lin FY. 2023; Schwann cells-derived exosomes promote functional recovery after spinal cord injury by promoting angiogenesis. Front Cell Neurosci. 16:1077071.103. Wirawan E, Vanden Berghe T, Lippens S, Agostinis P, Vandenabeele P. 2012; Autophagy: for better or for worse. Cell Res. 22:43–61. DOI: 10.1038/cr.2011.152. PMID: 18336290.104. Avin-Wittenberg T. 2019; Autophagy and its role in plant abiotic stress management. Plant Cell Environ. 42:1045–1053. DOI: 10.1111/pce.13404. PMID: 29998609.105. Zhang D, Wang F, Zhai X, Li XH, He XJ. 2018; Lithium promotes recovery of neurological function after spinal cord injury by inducing autophagy. Neural Regen Res. 13:2191–2199. DOI: 10.4103/1673-5374.241473. PMID: 30323152. PMCID: PMC6199946.106. Ray SK. 2020; Modulation of autophagy for neuroprotection and functional recovery in traumatic spinal cord injury. Neural Regen Res. 15:1601–1612. DOI: 10.4103/1673-5374.276322. PMID: 32209759. PMCID: PMC7437603.107. Hao HH, Wang L, Guo ZJ, et al. 2013; Valproic acid reduces autophagy and promotes functional recovery after spinal cord injury in rats. Neurosci Bull. 29:484–492.108. Muñoz-Galdeano T, Reigada D, Del Águila Á, et al. 2018; Cell specific changes of autophagy in a mouse model of contusive spinal cord injury. Front Cell Neurosci. 12:164. DOI: 10.3389/fncel.2018.00164. PMID: 29946241. PMCID: PMC6005838.109. Shi Z, Yuan S, Shi L, et al. 2021; Programmed cell death in spinal cord injury pathogenesis and therapy. Cell Prolif. 54:e12992. DOI: 10.1111/cpr.12992. PMID: 33506613. PMCID: PMC7941236.110. Liao HY, Wang ZQ, Ran R, Zhou KS, Ma CW, Zhang HH. 2021; Biological functions and therapeutic potential of autophagy in spinal cord injury. Front Cell Dev Biol. 9:761273. DOI: 10.3389/fcell.2021.761273. PMID: 34988074. PMCID: PMC8721099.111. Al Mamun A, Wu Y, Monalisa I, et al. 2020; Role of pyroptosis in spinal cord injury and its therapeutic implications. J Adv Res. 28:97–109. DOI: 10.1016/j.jare.2020.08.004. PMID: 33364048. PMCID: PMC7753222.112. Wang ZY, Lin JH, Muharram A, Liu WG. 2014; Beclin-1-mediated autophagy protects spinal cord neurons against mecha-nical injury-induced apoptosis. Apoptosis. 19:933–945. DOI: 10.1007/s10495-014-0976-1. PMID: 24623173.113. Li W, Yao S, Li H, Meng Z, Sun X. 2021; Curcumin promotes functional recovery and inhibits neuronal apoptosis after spinal cord injury through the modulation of autophagy. J Spinal Cord Med. 44:37–45. DOI: 10.1080/10790268.2019.1616147. PMID: 31162984. PMCID: PMC7919922.114. Li C, Jiao G, Wu W, et al. 2019; Exosomes from bone marrow mesenchymal stem cells inhibit neuronal apoptosis and promote motor function recovery via the Wnt/β-catenin signaling pathway. Cell Transplant. 28:1373–1383. DOI: 10.1177/0963689719870999. PMID: 31423807. PMCID: PMC6802144.115. Kang J, Guo Y. 2022; Human umbilical cord mesenchymal stem cells derived exosomes promote neurological function reco-very in a rat spinal cord injury model. Neurochem Res. 47:1532–1540. DOI: 10.1007/s11064-022-03545-9. PMID: 35132478.116. Gu J, Jin ZS, Wang CM, Yan XF, Mao YQ, Chen S. 2020; Bone marrow mesenchymal stem cell-derived exosomes improves spinal cord function after injury in rats by activating auto-phagy. Drug Des Devel Ther. 14:1621–1631. DOI: 10.2147/DDDT.S237502. PMID: 32425507. PMCID: PMC7196809.117. Xu G, Ao R, Zhi Z, Jia J, Yu B. 2019; miR-21 and miR-19b delivered by hMSC-derived EVs regulate the apoptosis and differentiation of neurons in patients with spinal cord injury. J Cell Physiol. 234:10205–10217. DOI: 10.1002/jcp.27690. PMID: 30387159.118. Kang J, Li Z, Zhi Z, Wang S, Xu G. 2019; MiR-21 derived from the exosomes of MSCs regulates the death and differentia-tion of neurons in patients with spinal cord injury. Gene Ther. 26:491–503. DOI: 10.1038/s41434-019-0101-8. PMID: 31570818.119. Zhou X, Chu X, Yuan H, et al. 2019; Mesenchymal stem cell derived EVs mediate neuroprotection after spinal cord injury in rats via the microRNA-21-5p/FasL gene axis. Biomed Pha-rmacother. 115:108818. DOI: 10.1016/j.biopha.2019.108818. PMID: 31102912.120. Xiao X, Li W, Rong D, et al. 2021; Human umbilical cord mesenchymal stem cells-derived extracellular vesicles facilitate the repair of spinal cord injury via the miR-29b-3p/PTEN/Akt/mTOR axis. Cell Death Discov. 7:212. DOI: 10.1038/s41420-021-00572-3. PMID: 34381025. PMCID: PMC8357833.121. Jia X, Huang G, Wang S, et al. 2021; Extracellular vesicles derived from mesenchymal stem cells containing microRNA-381 protect against spinal cord injury in a rat model via the BRD4/WNT5A axis. Bone Joint Res. 10:328–339. DOI: 10.1302/2046-3758.105.BJR-2020-0020.R1. PMID: 34024119. PMCID: PMC8160032.122. Liang Y, Wu JH, Zhu JH, Yang H. 2022; Exosomes secreted by hypoxia-pre-conditioned adipose-derived mesenchymal stem cells reduce neuronal apoptosis in rats with spinal cord injury. J Neurotrauma. 39:701–714. DOI: 10.1089/neu.2021.0290. PMID: 35018814.123. He X, Zhang J, Guo Y, Yang X, Huang Y, Hao D. 2022; Exosomal miR-9-5p derived from BMSCs alleviates apoptosis, inflam-mation and endoplasmic reticulum stress in spinal cord injury by regulating the HDAC5/FGF2 axis. Mol Immunol. 145:97–108. DOI: 10.1016/j.molimm.2022.03.007. PMID: 35316648.124. Huang T, Jia Z, Fang L, et al. 2022; Extracellular vesicle-derived miR-511-3p from hypoxia preconditioned adipose mesenchy-mal stem cells ameliorates spinal cord injury through the TRAF6/S1P axis. Brain Res Bull. 180:73–85. DOI: 10.1016/j.brainresbull.2021.12.015. PMID: 34974133.125. Bartanusz V, Jezova D, Alajajian B, Digicaylioglu M. 2011; The blood-spinal cord barrier: morphology and clinical implica-tions. Ann Neurol. 70:194–206. DOI: 10.1002/ana.22421. PMID: 21674586.126. Reinhold AK, Rittner HL. 2017; Barrier function in the peripheral and central nervous system-a review. Pflugers Arch. 469:123–134. DOI: 10.1007/s00424-016-1920-8. PMID: 27957611.127. Jin LY, Li J, Wang KF, et al. 2021; Blood-spinal cord barrier in spinal cord injury: a review. J Neurotrauma. 38:1203–1224. DOI: 10.1089/neu.2020.7413. PMID: 33292072.128. Jo DH, Kim JH, Heo JI, Kim JH, Cho CH. 2013; Interaction between pericytes and endothelial cells leads to formation of tight junction in hyaloid vessels. Mol Cells. 36:465–471. DOI: 10.1007/s10059-013-0228-1. PMID: 24213675. PMCID: PMC3887934.129. Lu Y, Zhou Y, Zhang R, et al. 2019; Bone mesenchymal stem cell-derived extracellular vesicles promote recovery following spinal cord injury via improvement of the integrity of the blood-spinal cord barrier. Front Neurosci. 13:209. DOI: 10.3389/fnins.2019.00209. PMID: 30914918. PMCID: PMC6423165.130. Zhou Y, Wen LL, Li YF, et al. 2022; Exosomes derived from bone marrow mesenchymal stem cells protect the injured spinal cord by inhibiting pericyte pyroptosis. Neural Regen Res. 17:194–202. DOI: 10.4103/1673-5374.314323. PMID: 34100456. PMCID: PMC8451579.131. Xin W, Qiang S, Jianing D, et al. 2021; Human bone marrow mesenchymal stem cell-derived exosomes attenuate blood-spinal cord barrier disruption via the TIMP2/MMP pathway after acute spinal cord injury. Mol Neurobiol. 58:6490–6504. DOI: 10.1007/s12035-021-02565-w. PMID: 34554399.132. Nakazaki M, Morita T, Lankford KL, Askenase PW, Kocsis JD. 2021; Small extracellular vesicles released by infused mesenchymal stromal cells target M2 macrophages and promote TGF-β upregulation, microvascular stabilization and functional recovery in a rodent model of severe spinal cord injury. J Extracell Vesicles. 10:e12137. DOI: 10.1002/jev2.12137. PMID: 34478241. PMCID: PMC8408371.133. de Freria CM, Van Niekerk E, Blesch A, Lu P. 2021; Neural stem cells: promoting axonal regeneration and spinal cord connec-tivity. Cells. 10:3296. DOI: 10.3390/cells10123296. PMID: 34943804. PMCID: PMC8699545.134. Zhang Y, Chopp M, Liu XS, et al. 2017; Exosomes derived from mesenchymal stromal cells promote axonal growth of cortical neurons. Mol Neurobiol. 54:2659–2673. DOI: 10.1007/s12035-016-9851-0. PMID: 26993303. PMCID: PMC5028236.135. Lopez-Verrilli MA, Caviedes A, Cabrera A, Sandoval S, Wyneken U, Khoury M. 2016; Mesenchymal stem cell-derived exosomes from different sources selectively promote neuritic outgrowth. Neuroscience. 320:129–139. DOI: 10.1016/j.neuroscience.2016.01.061. PMID: 26851773.136. Zhou W, Silva M, Feng C, et al. 2021; Exosomes derived from human placental mesenchymal stem cells enhanced the recovery of spinal cord injury by activating endogenous neurogenesis. Stem Cell Res Ther. 12:174. DOI: 10.1186/s13287-021-02248-2. PMID: 33712072. PMCID: PMC7953814.137. Li C, Li X, Shi Z, et al. 2022; Exosomes from LPS-preconditioned bone marrow MSCs accelerated peripheral nerve regeneration via M2 macrophage polarization: involvement of TSG-6/NF-κB/NLRP3 signaling pathway. Exp Neurol. 356:114139. DOI: 10.1016/j.expneurol.2022.114139. PMID: 35690131.138. Wang Y, Lai X, Wu D, Liu B, Wang N, Rong L. 2021; Umbilical mesenchymal stem cell-derived exosomes facilitate spinal cord functional recovery through the miR-199a-3p/145-5p-mediated NGF/TrkA signaling pathway in rats. Stem Cell Res Ther. 12:117. DOI: 10.1186/s13287-021-02148-5. PMID: 33579361. PMCID: PMC7879635.139. Han T, Song P, Wu Z, et al. 2022; MSC secreted extracellular vesi-cles carrying TGF-beta upregulate Smad 6 expression and promote the regrowth of neurons in spinal cord injured rats. Stem Cell Rev Rep. 18:1078–1096. DOI: 10.1007/s12015-021-10219-6. PMID: 34449013. PMCID: PMC8942898.140. Wang Y, Han T, Guo R, et al. 2022; Micro-RNA let-7a-5p derived from mesenchymal stem cell-derived extracellular vesicles promotes the regrowth of neurons in spinal-cord-injured rats by targeting the HMGA2/SMAD2 axis. Front Mol Neurosci. 15:850364. DOI: 10.3389/fnmol.2022.850364. PMID: 35401112. PMCID: PMC8990843.141. Batrakova EV, Kim MS. 2015; Using exosomes, naturally-equipped nanocarriers, for drug delivery. J Control Release. 219:396–405. DOI: 10.1016/j.jconrel.2015.07.030. PMID: 26241750. PMCID: PMC4656109.142. Mondal J, Pillarisetti S, Junnuthula V, et al. 2023; Hybrid exosomes, exosome-like nanovesicles and engineered exosomes for therapeutic applications. J Control Release. 353:1127–1149. DOI: 10.1016/j.jconrel.2022.12.027. PMID: 36528193.143. Luan X, Sansanaphongpricha K, Myers I, Chen H, Yuan H, Sun D. 2017; Engineering exosomes as refined biological nanoplatforms for drug delivery. Acta Pharmacol Sin. 38:754–763. DOI: 10.1038/aps.2017.12. PMID: 28392567. PMCID: PMC5520184.144. Li C, Li X, Zhao B, Wang C. 2020; Exosomes derived from miR-544-modified mesenchymal stem cells promote recovery after spinal cord injury. Arch Physiol Biochem. 126:369–375. DOI: 10.1080/13813455.2019.1691601. PMID: 32141339.145. Li D, Zhang P, Yao X, et al. 2018; Exosomes derived from miR-133b-modified mesenchymal stem cells promote recovery after spinal cord injury. Front Neurosci. 12:845. DOI: 10.3389/fnins.2018.00845. PMID: 30524227. PMCID: PMC6262643.146. Huang JH, Xu Y, Yin XM, Lin FY. 2020; Exosomes derived from miR-126-modified MSCs promote angiogenesis and neurogenesis and attenuate apoptosis after spinal cord injury in rats. Neuroscience. 424:133–145. DOI: 10.1016/j.neuroscience.2019.10.043. PMID: 31704348.147. Ren ZW, Zhou JG, Xiong ZK, Zhu FZ, Guo XD. 2019; Effect of exosomes derived from MiR-133b-modified ADSCs on the recovery of neurological function after SCI. Eur Rev Med Pharmacol Sci. 23:52–60. DOI: 10.26355/eurrev_201901_16747. PMID: 30657546.148. Yu T, Zhao C, Hou S, Zhou W, Wang B, Chen Y. 2019; Exo-somes secreted from miRNA-29b-modified mesenchymal stem cells repaired spinal cord injury in rats. Braz J Med Biol Res. 52:e8735. DOI: 10.1590/1414-431X20198735. PMID: 31826179. PMCID: PMC6903804.149. Zhang A, Bai Z, Yi W, Hu Z, Hao J. 2021; Overexpression of miR-338-5p in exosomes derived from mesenchymal stromal cells provides neuroprotective effects by the Cnr1/Rap1/Akt pathway after spinal cord injury in rats. Neurosci Lett. 761:136124. DOI: 10.1016/j.neulet.2021.136124. PMID: 34302891.150. Chen J, Zhu C, Jia W, Wang J, Gu L. 2020; MiR-455-5p attenuates cerebral ischemic reperfusion injury by targeting FLT3. J Cardiovasc Pharmacol. 76:627–634. DOI: 10.1097/fjc.0000000000000898. PMID: 32833902.151. Liu B, Zheng W, Dai L, Fu S, Shi E. 2022; Bone marrow mesenchymal stem cell derived exosomal miR-455-5p protects against spinal cord ischemia reperfusion injury. Tissue Cell. 74:101678. DOI: 10.1016/j.tice.2021.101678. PMID: 34823099.152. Chen Y, Tian Z, He L, et al. 2021; Exosomes derived from miR-26a-modified MSCs promote axonal regeneration via the PTEN/AKT/mTOR pathway following spinal cord injury. Stem Cell Res Ther. 12:224. DOI: 10.1186/s13287-021-02282-0. PMID: 33820561. PMCID: PMC8022427.153. Sheng Y, Zhou X, Wang J, et al. 2021; MSC derived EV loaded with miRNA-22 inhibits the inflammatory response and nerve fun-ction recovery after spinal cord injury in rats. J Cell Mol Med. 25:10268–10278. DOI: 10.1111/jcmm.16965. PMID: 34609045. PMCID: PMC8572783.154. Huang W, Lin M, Yang C, et al. 2021; Rat bone mesenchymal stem cell-derived exosomes loaded with miR-494 promoting neurofilament regeneration and behavioral function recovery after spinal cord injury. Oxid Med Cell Longev. 2021:1634917. DOI: 10.1155/2021/1634917. PMID: 34635862. PMCID: PMC8501401.155. Jiang Z, Zhang J. 2021; Mesenchymal stem cell-derived exosomes containing miR-145-5p reduce inflammation in spinal cord injury by regulating the TLR4/NF-κB signaling pathway. Cell Cycle. 20:993–1009. DOI: 10.1080/15384101.2021.1919825. PMID: 33945431. PMCID: PMC8172161.156. Ren Z, Qi Y, Sun S, Tao Y, Shi R. 2020; Mesenchymal stem cell-derived exosomes: hope for spinal cord injury repair. Stem Cells Dev. 29:1467–1478. DOI: 10.1089/scd.2020.0133. PMID: 33045910.157. Rao D, Huang D, Sang C, Zhong T, Zhang Z, Tang Z. 2022; Adva-nces in mesenchymal stem cell-derived exosomes as drug deli-very vehicles. Front Bioeng Biotechnol. 9:797359. DOI: 10.3389/fbioe.2021.797359. PMID: 35186913. PMCID: PMC8854766.158. Li Q, Fu X, Kou Y, Han N. 2023; Engineering strategies and optimized delivery of exosomes for theranostic application in nerve tissue. Theranostics. 13:4266–4286. DOI: 10.7150/thno.84971. PMID: 37554270. PMCID: PMC10405842.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Clinical Response of 277 Patients with Spinal Cord Injury to Stem Cell Therapy in Iraq
- Current Concept and Future of the Management of Spinal Cord Injury: A Systematic Review
- Current Concept of Stem Cell Therapy for Spinal Cord Injury: A Review
- Inhibition of Ferroptosis by Mesenchymal Stem Cell-Derived Exosomes in Acute Spinal Cord Injury: Role of Nrf2/GCH1/BH4 Axis
- Stem cell exosomes: new hope and future potential for relieving liver fibrosis