Korean Circ J.
2024 Aug;54(8):485-496. 10.4070/kcj.2024.0046.
Discordance Between Angiographic Assessment and Fractional Flow Reserve or Intravascular Ultrasound in Intermediate Coronary Lesions: A Post-hoc Analysis of the FLAVOUR Trial
- Affiliations
-
- 1Division of Cardiology, Department of Internal Medicine, Wonju Severance Christian Hospital, Yonsei University Wonju College of Medicine, Wonju, Korea
- 2Division of Cardiology, Department of Internal Medicine, The Second Affiliated Hospital Zhejiang University School of Medicine, Hangzhou, China
- 3Division of Cardiology, Department of Internal Medicine, Samsung Medical Center, Seoul, Korea
- 4Division of Cardiology, Department of Internal Medicine, Keimyung University Dongsan Medical Center, Daegu, Korea
- 5Division of Cardiology, Department of Internal Medicine, Inje University Ilsan Paik Hospital, Goyang, Korea
- 6Division of Cardiology, Department of Internal Medicine, Kangwon National University Hospital, Chuncheon, Korea
- 7Division of Cardiology, Department of Internal Medicine, Kyung Hee University Hospital, Seoul, Korea
- 8Division of Cardiology, Department of Internal Medicine, Affiliated Hangzhou First People’s Hospital, Zhejiang University School of Medicine, Hangzhou, China
- 9Division of Cardiology, Department of Internal Medicine, Hangzhou Normal University Affiliated Hospital, Hangzhou, China
- 10Division of Cardiology, Department of Internal Medicine, The 1st Affiliated Hospital of Wenzhou Medical University, Wenzhou, China
- 11Division of Cardiology, Department of Internal Medicine, The 2nd Affiliated Hospital of Wenzhou Medical University, Wenzhou, China
- 12Division of Cardiology, Department of Internal Medicine, Zhejiang Hospital, Hangzhou, China
- 13Division of Cardiology, Department of Internal Medicine, The Third Clinical Institute Affiliated To Wenzhou Medical University, Wenzhou, China
- 14Division of Cardiology, Department of Internal Medicine, Ningbo First Hospital, Ningbo, China
- 15Division of Cardiology, Department of Internal Medicine, The Affiliated Hospital of Medical School of Ningbo University, Ningbo, China
- 16Division of Cardiology, Department of Internal Medicine, Ajou University Hospital, Suwon, Korea
- 17Division of Cardiology, Department of Internal Medicine, Yeungnam University Medical Center, Daegu, Korea
- 18Division of Cardiology, Department of Internal Medicine, Uijeongbu Eulji Medical Center, Uijeongbu, Korea
- 19Division of Cardiology, Department of Internal Medicine, Ulsan University Hospital, University of Ulsan College of Medicine, Ulsan, Korea
- 20Division of Cardiology, Department of Internal Medicine, Seoul National University Hospital, Seoul, Korea
- KMID: 2558540
- DOI: http://doi.org/10.4070/kcj.2024.0046
Abstract
- Background and Objectives
Angiographic assessment of coronary stenosis severity using quantitative coronary angiography (QCA) is often inconsistent with that based on fractional flow reserve (FFR) or intravascular ultrasound (IVUS). We investigated the incidence of discrepancies between QCA and FFR or IVUS, and the outcomes of FFR- and IVUS-guided strategies in discordant coronary lesions.
Methods
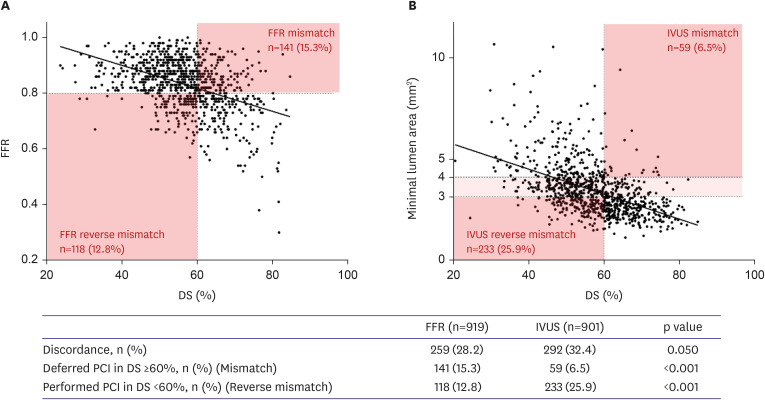
This study was a post-hoc analysis of the FLAVOUR study. We used a QCA-derived diameter stenosis (DS) of 60% or greater, the highest tertile, to classify coronary lesions as concordant or discordant with FFR or IVUS criteria for percutaneous coronary intervention (PCI). The patient-oriented composite outcome (POCO) was defined as a composite of death, myocardial infarction, or revascularization at 24 months.
Results
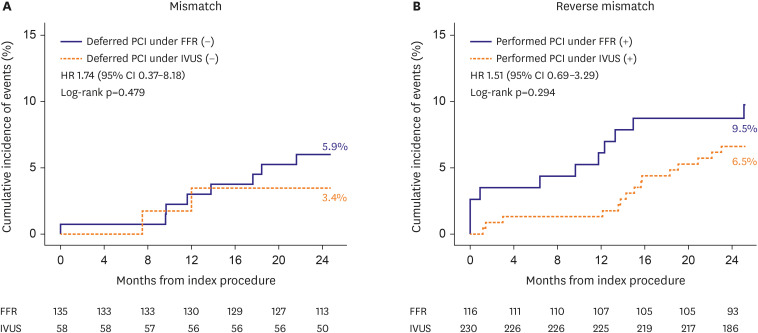
The discordance rate between QCA and FFR or IVUS was 30.2% (n=551). The QCAFFR discordance rate was numerically lower than the QCA-IVUS discordance rate (28.2% vs. 32.4%, p=0.050). In 200 patients with ≥60% DS, PCI was deferred according to negative FFR (n=141) and negative IVUS (n=59) (15.3% vs. 6.5%, p<0.001). The POCO incidence was comparable between the FFR- and IVUS-guided deferral strategies (5.9% vs. 3.4%, p=0.479). Conversely, 351 patients with DS <60% underwent PCI according to positive FFR (n=118) and positive IVUS (n=233) (12.8% vs. 25.9%, p<0.001). FFR- and IVUS-guided PCI did not differ in the incidence of POCO (9.5% vs. 6.5%, p=0.294).
Conclusions
The proportion of QCA-FFR or IVUS discordance was approximately one third for intermediate coronary lesions. FFR- or IVUS-guided strategies for these lesions were comparable with respect to POCO at 24 months.
Keyword
Figure
Reference
-
1. Ahn SG, Lee SJ. Dose coronary angiography suffice for assessment of intermediate coronary stenosis? Korean Circ J. 2019; 49:1033–1034. PMID: 31456370.2. Pijls NH, De Bruyne B, Peels K, et al. Measurement of fractional flow reserve to assess the functional severity of coronary-artery stenoses. N Engl J Med. 1996; 334:1703–1708. PMID: 8637515.3. Tonino PA, De Bruyne B, Pijls NH, et al. Fractional flow reserve versus angiography for guiding percutaneous coronary intervention. N Engl J Med. 2009; 360:213–224. PMID: 19144937.4. Lee JM, Kim HK, Park KH, et al. Fractional flow reserve versus angiography-guided strategy in acute myocardial infarction with multivessel disease: a randomized trial. Eur Heart J. 2023; 44:473–484. PMID: 36540034.5. Briguori C, Anzuini A, Airoldi F, et al. Intravascular ultrasound criteria for the assessment of the functional significance of intermediate coronary artery stenoses and comparison with fractional flow reserve. Am J Cardiol. 2001; 87:136–141. PMID: 11152827.6. Koo BK, Yang HM, Doh JH, et al. Optimal intravascular ultrasound criteria and their accuracy for defining the functional significance of intermediate coronary stenoses of different locations. JACC Cardiovasc Interv. 2011; 4:803–811. PMID: 21777890.7. Hong SJ, Kim BK, Shin DH, et al. Effect of intravascular ultrasound-guided vs angiography-guided everolimus-eluting stent implantation: the IVUS-XPL randomized clinical trial. JAMA. 2015; 314:2155–2163. PMID: 26556051.8. Zhang J, Gao X, Kan J, et al. Intravascular ultrasound versus angiography-guided drug-eluting stent implantation: the ULTIMATE trial. J Am Coll Cardiol. 2018; 72:3126–3137. PMID: 30261237.9. Lee JM, Choi KH, Song YB, et al. Intravascular imaging-guided or angiography-guided complex PCI. N Engl J Med. 2023; 388:1668–1679. PMID: 36876735.10. Koo BK, Hu X, Kang J, et al. Fractional flow reserve or intravascular ultrasonography to guide PCI. N Engl J Med. 2022; 387:779–789. PMID: 36053504.11. Tonino PA, Fearon WF, De Bruyne B, et al. Angiographic versus functional severity of coronary artery stenoses in the FAME study fractional flow reserve versus angiography in multivessel evaluation. J Am Coll Cardiol. 2010; 55:2816–2821. PMID: 20579537.12. Park SJ, Kang SJ, Ahn JM, et al. Visual-functional mismatch between coronary angiography and fractional flow reserve. JACC Cardiovasc Interv. 2012; 5:1029–1036. PMID: 23078732.13. Phan TQ, Nguyen LH, Nguyen LV, et al. Imaging characteristics of mismatch lesions: an angiographic and intravascular ultrasound analysis of 1369 coronary lesions. Angiology. 2019; 70:756–764. PMID: 30665308.14. Kang J, Koo BK, Hu X, et al. Comparison of fractional FLow Reserve And Intravascular ultrasound-guided Intervention Strategy for Clinical OUtcomes in Patients with InteRmediate Stenosis (FLAVOUR): rationale and design of a randomized clinical trial. Am Heart J. 2018; 199:7–12. PMID: 29754669.15. Jang HJ, Koo BK, Lee HS, et al. Safety and efficacy of a novel hyperaemic agent, intracoronary nicorandil, for invasive physiological assessments in the cardiac catheterization laboratory. Eur Heart J. 2013; 34:2055–2062. PMID: 23396491.16. Xaplanteris P, Fournier S, Pijls NH, et al. Five-year outcomes with PCI guided by fractional flow reserve. N Engl J Med. 2018; 379:250–259. PMID: 29785878.17. Waksman R, Legutko J, Singh J, et al. FIRST: Fractional Flow Reserve and Intravascular Ultrasound Relationship Study. J Am Coll Cardiol. 2013; 61:917–923. PMID: 23352786.18. Calvert PA, Obaid DR, O’Sullivan M, et al. Association between IVUS findings and adverse outcomes in patients with coronary artery disease: the VIVA (VH-IVUS in Vulnerable Atherosclerosis) study. JACC Cardiovasc Imaging. 2011; 4:894–901. PMID: 21835382.19. Garcia-Garcia HM, McFadden EP, Farb A, et al. Standardized end point definitions for coronary intervention trials: the academic research consortium-2 consensus document. Circulation. 2018; 137:2635–2650. PMID: 29891620.20. Neumann FJ, Sousa-Uva M, Ahlsson A, et al. 2018 ESC/EACTS guidelines on myocardial revascularization. Eur Heart J. 2019; 40:87–165. PMID: 30165437.21. Lawton JS, Tamis-Holland JE, Bangalore S, et al. 2021 ACC/AHA/SCAI guideline for coronary artery revascularization: executive summary: a report of the American College of Cardiology/American Heart Association joint committee on clinical practice guidelines. Circulation. 2022; 145:e4–e17. PMID: 34882436.22. Ciccarelli G, Barbato E, Toth GG, et al. Angiography versus hemodynamics to predict the natural history of coronary stenoses: fractional flow reserve versus angiography in multivessel evaluation 2 substudy. Circulation. 2018; 137:1475–1485. PMID: 29162610.23. Ahn SG, Suh J, Hung OY, et al. Discordance between fractional flow reserve and coronary flow reserve: insights from intracoronary imaging and physiological assessment. JACC Cardiovasc Interv. 2017; 10:999–1007. PMID: 28521932.24. Li J, Elrashidi MY, Flammer AJ, et al. Long-term outcomes of fractional flow reserve-guided vs. angiography-guided percutaneous coronary intervention in contemporary practice. Eur Heart J. 2013; 34:1375–1383. PMID: 23344979.25. Lee JM, Kim H, Hong D, et al. Clinical outcomes of deferred lesions by IVUS versus FFR-guided treatment decision. Circ Cardiovasc Interv. 2023; 16:e013308. PMID: 38018840.26. Burzotta F, Leone AM, Aurigemma C, et al. Fractional flow reserve or optical coherence tomography to guide management of angiographically intermediate coronary stenosis: a single-center trial. JACC Cardiovasc Interv. 2020; 13:49–58. PMID: 31918942.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Cost-effectiveness of Fractional Flow Reserve Versus Intravascular Ultrasound to Guide Percutaneous Coronary Intervention: Results From the FLAVOUR Study
- Fractional Flow Reserve in Coronary Artery Disease: Comparison with Intravascular Ultrasound
- Physiologic Assessment of Coronary Artery Disease: Past, Present and Future
- Comparison between Fractinal Flow Reserve and Intravascular Ultrasound for Evaluation of Optimal Coronary Angioplasty
- Funtional significance of the intermediate lesion in a single coronary artery assessed by fractional flow reserve