Nutr Res Pract.
2024 Aug;18(4):511-522. 10.4162/nrp.2024.18.4.511.
Homocysteine levels are associated with diabetes mellitus in Chinese with H-type hypertension
- Affiliations
-
- 1Department of Cardiovascular, The People’s Hospital of Zigui County, Yichang 443600, China
- 2Department of Cardiovascular, Changyang Tujia Autonomous County People’s Hospital, Yichang 443000, China
- 3Department of Cardiovascular, People’s Hospital of Huantai County, Zibo 255000, China
- 4Department of Cardiovascular, The People’s Hospital of Wufeng Tujia Autonomous County, Yichang 443400, China
- 5Clinical laboratory, The People’s Hospital of Wufeng Tujia Autonomous County, Yichang 443400, China
- 6Department of Cardiovascular, Zigui County Hospital of Traditional Chinese Medicine, Yichang 443600, China
- 7Clinical laboratory, Zigui County Hospital of Traditional Chinese Medicine, Yichang 443600, China
- 8Clinical laboratory, Changyang Tujia Autonomous County People’s Hospital, Yichang 443000, China
- 9Department of Cardiovascular, Yidu Hospital of Traditional Chinese Medicine, Yidu 443300, China
- KMID: 2558489
- DOI: http://doi.org/10.4162/nrp.2024.18.4.511
Abstract
- BACKGROUND/OBJECTIVES
The study examined the association between homocysteine and diabetes mellitus in patients with H-type hypertension and assessed the possible effect modifiers.
SUBJECTS/METHODS
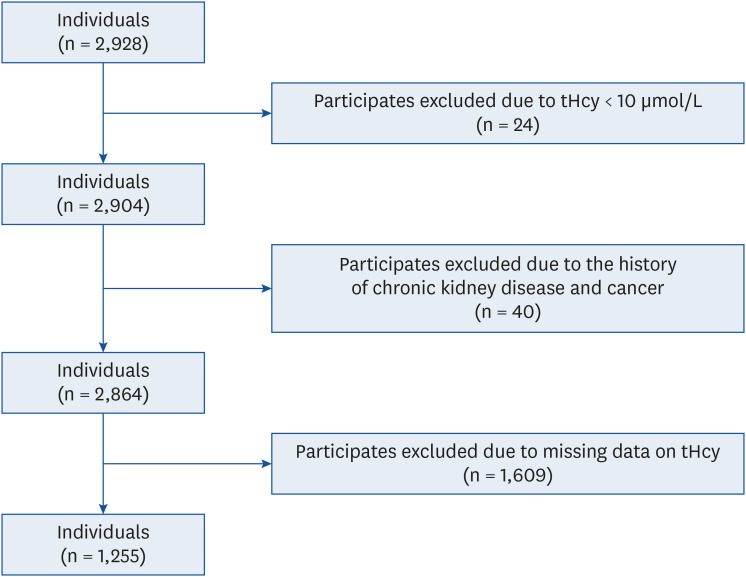
This cross-sectional study included 1,255 eligible participants in the ‘H-type Hypertension Management and Stroke Prevention Strategic International Science and Technology Innovation Cooperation Project’ among rural Chinese people with H-type hypertension. A multivariate logistic regression model was used to evaluate the relationship between homocysteine and diabetes mellitus.
RESULTS
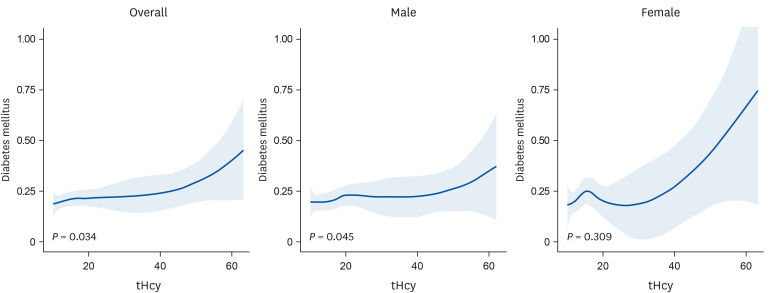
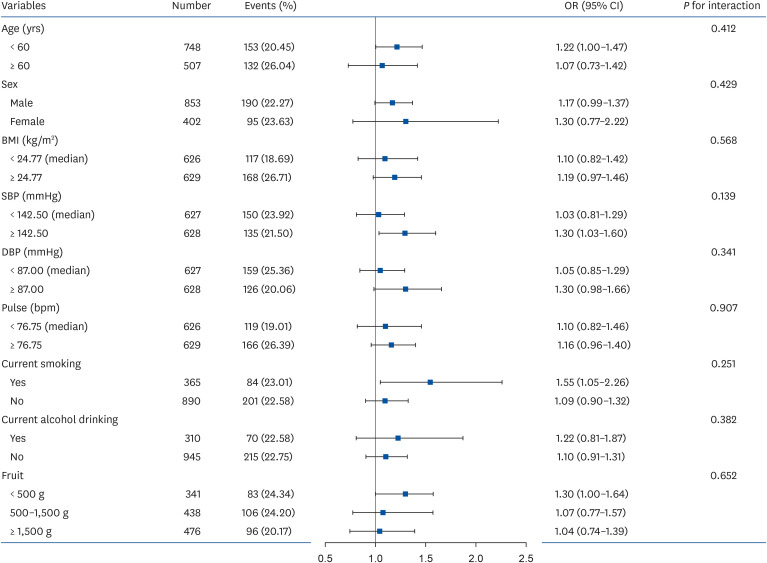
The mean level of total homocysteine (tHcy) in the diabetes mellitus population was 19.37 μmol/L, which was significantly higher than the non-diabetic patients (18.18 μmol/L). When tHcy was analyzed as a continuous variable, the odds ratio (OR) of diabetes was 1.17 (95% confidence interval [CI], 1.01–1.35; per interquartile range). When tHcy was stratified according to the quintile, the ORs for diabetes were 2.86 (95% CI, 1.22–6.69) in the highest quintile (tHcy ≥ 20.60 μmol/L) compared to the reference group (tHcy < 12.04 μmol/L). When tHcy was grouped by 15 μmol/L and 20 μmol/L, patients with tHcy ≥ 20 μmol/L had a significantly (P = 0.037) higher risk of diabetes (OR, 2.03; 95% CI, 1.04–3.96) than in those with tHcy < 15 μmol/L. Subgroup analysis showed that the tHcy-diabetes association was unaffected by other variables.
CONCLUSION
In this study of rural Chinese people with H-type hypertension, the tHcy levels showed a positive association with diabetes mellitus. This independent association is unaffected by other potential risk factors.
Figure
Reference
-
1. Chatterjee S, Khunti K, Davies MJ. Type 2 diabetes. Lancet. 2017; 389:2239–2251. PMID: 28190580.
Article2. Boushey CJ, Beresford SA, Omenn GS, Motulsky AG. A quantitative assessment of plasma homocysteine as a risk factor for vascular disease. Probable benefits of increasing folic acid intakes. JAMA. 1995; 274:1049–1057. PMID: 7563456.
Article3. Verhoef P, Stampfer MJ, Buring JE, Gaziano JM, Allen RH, Stabler SP, Reynolds RD, Kok FJ, Hennekens CH, Willett WC. Homocysteine metabolism and risk of myocardial infarction: relation with vitamins B6, B12, and folate. Am J Epidemiol. 1996; 143:845–859. PMID: 8610698.4. Emoto M, Kanda H, Shoji T, Kawagishi T, Komatsu M, Mori K, Tahara H, Ishimura E, Inaba M, Okuno Y, et al. Impact of insulin resistance and nephropathy on homocysteine in type 2 diabetes. Diabetes Care. 2001; 24:533–538. PMID: 11289481.
Article5. Hoogeveen EK, Kostense PJ, Beks PJ, Mackaay AJ, Jakobs C, Bouter LM, Heine RJ, Stehouwer CD. Hyperhomocysteinemia is associated with an increased risk of cardiovascular disease, especially in non-insulin-dependent diabetes mellitus: a population-based study. Arterioscler Thromb Vasc Biol. 1998; 18:133–138. PMID: 9445267.
Article6. Ala OA, Akintunde AA, Ikem RT, Kolawole BA, Ala OO, Adedeji TA. Association between insulin resistance and total plasma homocysteine levels in type 2 diabetes mellitus patients in south west Nigeria. Diabetes Metab Syndr. 2017; 11(Suppl 2):S803–S809. PMID: 28610915.
Article7. Ndrepepa G, Kastrati A, Braun S, Koch W, Kölling K, Mehilli J, Schömig A. Circulating homocysteine levels in patients with type 2 diabetes mellitus. Nutr Metab Cardiovasc Dis. 2008; 18:66–73. PMID: 17027242.
Article8. Passaro A, D’Elia K, Pareschi PL, Calzoni F, Carantoni M, Fellin R, Solini A. Factors influencing plasma homocysteine levels in type 2 diabetes. Diabetes Care. 2000; 23:420–421. PMID: 10868878.9. Yu C, Wang J, Wang F, Han X, Hu H, Yuan J, Miao X, Yao P, Wei S, Wang Y, et al. Inverse association between plasma homocysteine concentrations and type 2 diabetes mellitus among a middle-aged and elderly Chinese population. Nutr Metab Cardiovasc Dis. 2018; 28:278–284. PMID: 29337020.
Article10. Executive summary: standards of medical care in diabetes--2010. Diabetes Care. 2010; 33(Suppl 1):S4–10. PMID: 20042774.11. Ebesunun MO, Obajobi EO. Elevated plasma homocysteine in type 2 diabetes mellitus: a risk factor for cardiovascular diseases. Pan Afr Med J. 2012; 12:48. PMID: 22937188.12. Yuan X, Ding S, Zhou L, Wen S, Du A, Diao J. Association between plasma homocysteine levels and pancreatic islet beta-cell function in the patients with type 2 diabetes mellitus: a cross-sectional study from China. Ann Palliat Med. 2021; 10:8169–8179. PMID: 34353101.
Article13. Schaffer A, Verdoia M, Barbieri L, Cassetti E, Suryapranata H, De Luca G. Impact of diabetes on homocysteine levels and its relationship with coronary artery disease: a single-centre cohort study. Ann Nutr Metab. 2016; 68:180–188. PMID: 26950830.
Article14. Platt DE, Hariri E, Salameh P, Merhi M, Sabbah N, Helou M, Mouzaya F, Nemer R, Al-Sarraj Y, El-Shanti H, et al. Type II diabetes mellitus and hyperhomocysteinemia: a complex interaction. Diabetol Metab Syndr. 2017; 9:19. PMID: 28331553.15. Wang YS, Ye J, Yang X, Zhang GP, Cao YH, Zhang R, Dai W, Zhang Q. Association of retinol binding protein-4, cystatin C, homocysteine and high-sensitivity C-reactive protein levels in patients with newly diagnosed type 2 diabetes mellitus. Arch Med Sci. 2019; 15:1203–1216. PMID: 31572465.
Article16. Qin X, Li Y, Yuan H, Xie D, Tang G, Wang B, Wang X, Xu X, Xu X, Hou F. Relationship of MTHFR gene 677C → T polymorphism, homocysteine, and estimated glomerular filtration rate levels with the risk of new-onset diabetes. Medicine (Baltimore). 2015; 94:e563. PMID: 25700330.17. Smulders YM, Rakic M, Slaats EH, Treskes M, Sijbrands EJ, Odekerken DA, Stehouwer CD, Silberbusch J. Fasting and post-methionine homocysteine levels in NIDDM. Determinants and correlations with retinopathy, albuminuria, and cardiovascular disease. Diabetes Care. 1999; 22:125–132. PMID: 10333913.
Article18. Buysschaert M, Dramais AS, Wallemacq PE, Hermans MP. Hyperhomocysteinemia in type 2 diabetes: relationship to macroangiopathy, nephropathy, and insulin resistance. Diabetes Care. 2000; 23:1816–1822. PMID: 11128359.
Article19. Koehler KM, Baumgartner RN, Garry PJ, Allen RH, Stabler SP, Rimm EB. Association of folate intake and serum homocysteine in elderly persons according to vitamin supplementation and alcohol use. Am J Clin Nutr. 2001; 73:628–637. PMID: 11237942.20. Stickel F, Choi SW, Kim YI, Bagley PJ, Seitz HK, Russell RM, Selhub J, Mason JB. Effect of chronic alcohol consumption on total plasma homocysteine level in rats. Alcohol Clin Exp Res. 2000; 24:259–264. PMID: 10776661.
Article21. Russo GT, Di Benedetto A, Giorda C, Alessi E, Crisafulli G, Ientile R, Di Cesare E, Jacques PF, Raimondo G, Cucinotta D. Correlates of total homocysteine plasma concentration in type 2 diabetes. Eur J Clin Invest. 2004; 34:197–204. PMID: 15025678.
Article22. Wang B, Wu H, Li Y, Ban Q, Huang X, Chen L, Li J, Zhang Y, Cui Y, He M, et al. Effect of long-term low-dose folic acid supplementation on degree of total homocysteine-lowering: major effect modifiers. Br J Nutr. 2018; 120:1122–1130. PMID: 30401001.
Article23. Refsum H, Smith AD, Ueland PM, Nexo E, Clarke R, McPartlin J, Johnston C, Engbaek F, Schneede J, McPartlin C, et al. Facts and recommendations about total homocysteine determinations: an expert opinion. Clin Chem. 2004; 50:3–32. PMID: 14709635.
Article24. Thögersen AM, Nilsson TK, Dahlen G, Jansson JH, Boman K, Huhtasaari F, Hallmans G. Homozygosity for the C677-->T mutation of 5,10-methylenetetrahydrofolate reductase and total plasma homocyst(e)ine are not associated with greater than normal risk of a first myocardial infarction in northern Sweden. Coron Artery Dis. 2001; 12:85–90. PMID: 11281306.25. Friedman G, Goldschmidt N, Friedlander Y, Ben-Yehuda A, Selhub J, Babaey S, Mendel M, Kidron M, Bar-On H. A common mutation A1298C in human methylenetetrahydrofolate reductase gene: association with plasma total homocysteine and folate concentrations. J Nutr. 1999; 129:1656–1661. PMID: 10460200.
Article26. Stampfer MJ, Grodstein F. Can homocysteine be related to physical functioning? Am J Med. 2002; 113:610–611. PMID: 12459410.
Article27. Han L, Liu Y, Wang C, Tang L, Feng X, Astell-Burt T, Wen Q, Duan D, Lu N, Xu G, et al. Determinants of hyperhomocysteinemia in healthy and hypertensive subjects: a population-based study and systematic review. Clin Nutr. 2017; 36:1215–1230. PMID: 27908565.
Article28. Challa F, Getahun T, Sileshi M, Nigassie B, Geto Z, Ashibire G, Gelibo T, Teferra S, Seifu D, Sitotaw Y, et al. Prevalence of hyperhomocysteinaemia and associated factors among Ethiopian adult population in a 2015 national survey. BioMed Res Int. 2020; 2020:9210261. PMID: 32420383.
Article29. Zeng Q, Li F, Xiang T, Wang W, Ma C, Yang C, Chen H, Xiang H. Influence of food groups on plasma total homocysteine for specific MTHFR C677T genotypes in Chinese population. Mol Nutr Food Res. 2017; 61:1600351. PMID: 27515258.30. Shi C, Wang P, Airen S, Brown C, Liu Z, Townsend JH, Wang J, Jiang H. Nutritional and medical food therapies for diabetic retinopathy. Eye Vis (Lond). 2020; 7:33. PMID: 32582807.
Article31. Selhub J, Jacques PF, Rosenberg IH, Rogers G, Bowman BA, Gunter EW, Wright JD, Johnson CL. Serum total homocysteine concentrations in the third National Health and Nutrition Examination Survey (1991-1994): population reference ranges and contribution of vitamin status to high serum concentrations. Ann Intern Med. 1999; 131:331–339. PMID: 10475885.
Article32. Brattström L. Vitamins as homocysteine-lowering agents. J Nutr. 1996; 126:1276S–80S. PMID: 8642470.
Article33. Jacob RA, Wu MM, Henning SM, Swendseid ME. Homocysteine increases as folate decreases in plasma of healthy men during short-term dietary folate and methyl group restriction. J Nutr. 1994; 124:1072–1080. PMID: 8027858.
Article34. Selhub J, Jacques PF, Wilson PW, Rush D, Rosenberg IH. Vitamin status and intake as primary determinants of homocysteinemia in an elderly population. JAMA. 1993; 270:2693–2698. PMID: 8133587.35. Aydemir O, Türkçüoğlu P, Güler M, Celiker U, Ustündağ B, Yilmaz T, Metin K. Plasma and vitreous homocysteine concentrations in patients with proliferative diabetic retinopathy. Retina. 2008; 28:741–743. PMID: 18463519.
Article36. Wang T, Wang Q, Wang Z, Xiao Z, Liu L. Diagnostic value of the combined measurement of serum Hcy, serum Cys C, and urinary microalbumin in type 2 diabetes mellitus with early complicating diabetic nephropathy. ISRN Endocrinol. 2013; 2013:407452. PMID: 24159393.
Article37. Zheng LQ, Zhang HL, Guan ZH, Hu MY, Zhang T, Ge SJ. Elevated serum homocysteine level in the development of diabetic peripheral neuropathy. Genet Mol Res. 2015; 14:15365–15375. PMID: 26634502.
Article38. Hermans MP, Gala JL, Buysschaert M. The MTHFR CT polymorphism confers a high risk for stroke in both homozygous and heterozygous T allele carriers with type 2 diabetes. Diabet Med. 2006; 23:529–536. PMID: 16681562.
Article39. Ostrakhovitch EA, Tabibzadeh S. Homocysteine and age-associated disorders. Ageing Res Rev. 2019; 49:144–164. PMID: 30391754.40. Shin JY. Trends in the prevalence and management of diabetes in Korea: 2007-2017. Epidemiol Health. 2019; 41:e2019029. PMID: 31319658.
Article41. Xu R, Huang F, Wang Y, Liu Q, Lv Y, Zhang Q. Gender- and age-related differences in homocysteine concentration: a cross-sectional study of the general population of China. Sci Rep. 2020; 10:17401. PMID: 33060744.
Article42. Blom HJ. Determinants of plasma homocysteine. Am J Clin Nutr. 1998; 67:188–189. PMID: 9459363.
Article43. Choi SH, Choi-Kwon S, Kim MS, Kim JS. Poor nutrition and alcohol consumption are related to high serum homocysteine level at post-stroke. Nutr Res Pract. 2015; 9:503–510. PMID: 26425280.
Article44. Hornemann T. Serine deficiency causes complications in diabetes. Nature. 2023; 614:42–43.45. Yang M, Vousden KH. Serine and one-carbon metabolism in cancer. Nat Rev Cancer. 2016; 16:650–662. PMID: 27634448.
Article46. Davis SR, Stacpoole PW, Williamson J, Kick LS, Quinlivan EP, Coats BS, Shane B, Bailey LB, Gregory JF 3rd. Tracer-derived total and folate-dependent homocysteine remethylation and synthesis rates in humans indicate that serine is the main one-carbon donor. Am J Physiol Endocrinol Metab. 2004; 286:E272–E279. PMID: 14559726.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Plasma total homocysteine and macrovascular complications are associated with food and nutrient intake in patients with Type II diabetes mellitus
- The Relationship among Homocysteine, Bilirubin, and Diabetic Retinopathy
- Analysis of Classical Risk Factors and Homocysteine Level in Acute Myocardiac Infarction
- Effects of folic acid supplementation on serum homocysteine levels, lipid profiles, and vascular parameters in post-menopausal Korean women with type 2 diabetes mellitus
- Homocysteine as a Risk Factor for Development of Microalbuminuria in Type 2 Diabetes