Clin Endosc.
2024 Jul;57(4):542-546. 10.5946/ce.2022.209.
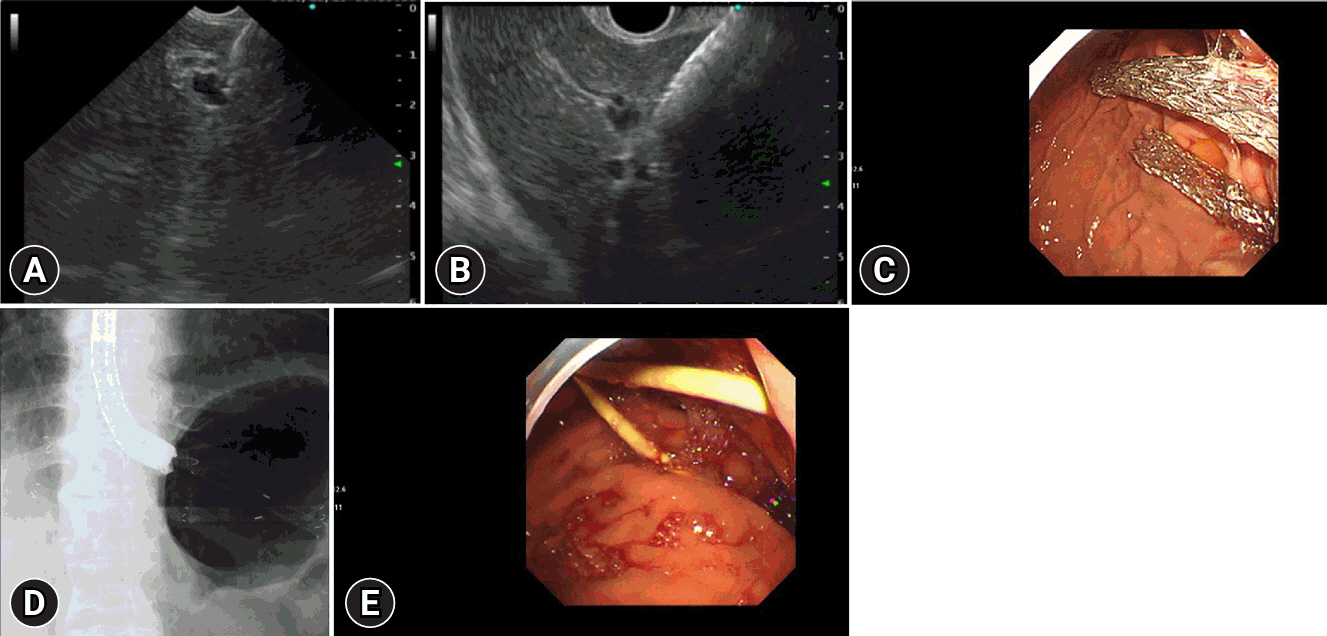
Endoscopic ultrasound-guided hepaticogastrostomy by puncturing both B2 and B3: a single center experience
- Affiliations
-
- 1Department of Gastroenterology, Aichi Cancer Center Hospital, Nagoya, Japan
- 2Department of Hepatology, Gastroenterology and Infectious Diseases, Faculty of Medicine, Al-Azhar University, Cairo, Egypt
- 3Department of Hepatology, Gastroenterology and Infectious Diseases, Faculty of Medicine for Girls, Al-Azhar University, Cairo, Egypt
- KMID: 2558112
- DOI: http://doi.org/10.5946/ce.2022.209
Abstract
- Endoscopic ultrasound-guided hepaticogastrostomy (EUS-HGS) through ducts B2 or B3 is effective in most patients with biliary obstruction, because B2 and B3 commonly join together. However, in some patients, B2 and B3 do not join each other due to invasive hilar tumors; therefore, single-route drainage is insufficient. Here, we investigated the feasibility and efficacy of EUS-HGS through both B2 and B3 simultaneously in seven patients. We decided to perform EUS-HGS through both B2 and B3 to achieve adequate biliary drainage because these two ducts were separate from each other. Here, we report a 100% technical and overall clinical success rate. Early adverse effects were closely monitored. Minimal bleeding was reported in one patient (1/7) and mild peritonitis in one patient (1/7). None of the patients experienced stent dysfunction, fever, or bile leakage after the procedure. EUS-HGS through both B2 and B3 simultaneously is safe, feasible, and effective for biliary drainage in patients with separated ducts.
Keyword
Figure
Reference
-
1. Park DH, Jang JW, Lee SS, et al. EUS-guided biliary drainage with transluminal stenting after failed ERCP: predictors of adverse events and long-term results. Gastrointest Endosc. 2011; 74:1276–1284.
Article2. Teoh AY, Dhir V, Kida M, et al. Consensus guidelines on the optimal management in interventional EUS procedures: results from the Asian EUS group RAND/UCLA expert panel. Gut. 2018; 67:1209–1228.
Article3. Okuno N, Hara K, Mizuno N, et al. Efficacy of the 6-mm fully covered self-expandable metal stent during endoscopic ultrasound-guided hepaticogastrostomy as a primary biliary drainage for the cases estimated difficult endoscopic retrograde cholangiopancreatography: a prospective clinical study. J Gastroenterol Hepatol. 2018; 33:1413–1421.4. Ogura T, Higuchi K. Technical tips for endoscopic ultrasound-guided hepaticogastrostomy. World J Gastroenterol. 2016; 22:3945–3951.
Article5. Hara K, Okuno N, Haba S, et al. How to perform EUS-guided hepaticogastrostomy easier and safer. J Hepatobiliary Pancreat Sci. 2020; 27:563–564.
Article6. Hara K, Yamao K, Mizuno N, et al. Endoscopic ultrasonography-guided biliary drainage: who, when, which, and how? World J Gastroenterol. 2016; 22:1297–1303.
Article7. Isayama H, Nakai Y, Itoi T, et al. Clinical practice guidelines for safe performance of endoscopic ultrasound/ultrasonography-guided biliary drainage: 2018. J Hepatobiliary Pancreat Sci. 2019; 26:249–269.
Article8. Sarawagi R, Sundar S, Raghuvanshi S, et al. Common and uncommon anatomical variants of intrahepatic bile ducts in magnetic resonance cholangiopancreatography and its clinical implication. Pol J Radiol. 2016; 81:250–255.
Article9. Giovannini M. EUS-guided hepaticogastrostomy. Endosc Ultrasound. 2019; 8(Suppl 1):S35–S39.
Article10. Elshair M, Hara K, Haba S, et al. Combined duodenal stenting and endoscopic ultrasound-guided hepaticogastrostomy using forward-viewing echoendoscope: a one-scope technique. Endoscopy. 2022; 54:E516–E517.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Safety and efficacy of novel oblique-viewing scope for B2-endoscopic ultrasound-guided hepaticogastrostomy
- Recent development of endoscopic ultrasound-guided biliary drainage
- Follow-up computed tomography can prevent stent migration after endoscopic ultrasound-guided hepaticogastrostomy
- Technical Review of Developments in Endoscopic Ultrasound-Guided Hepaticogastrostomy
- Endoscopic Ultrasound-Guided Hepaticogastrostomy: Technical Review and Tips to Prevent Adverse Events