Clin Endosc.
2021 Sep;54(5):651-659. 10.5946/ce.2021.020-KDDW.
Technical Review of Developments in Endoscopic Ultrasound-Guided Hepaticogastrostomy
- Affiliations
-
- 12nd Department of Internal Medicine, Osaka Medical College, Osaka, Japan
- KMID: 2520547
- DOI: http://doi.org/10.5946/ce.2021.020-KDDW
Abstract
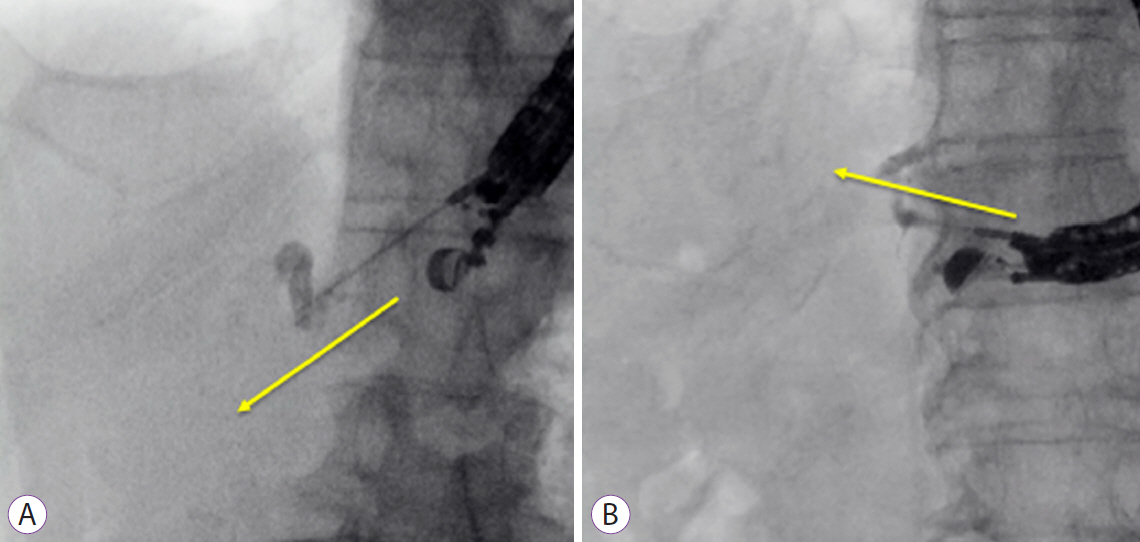
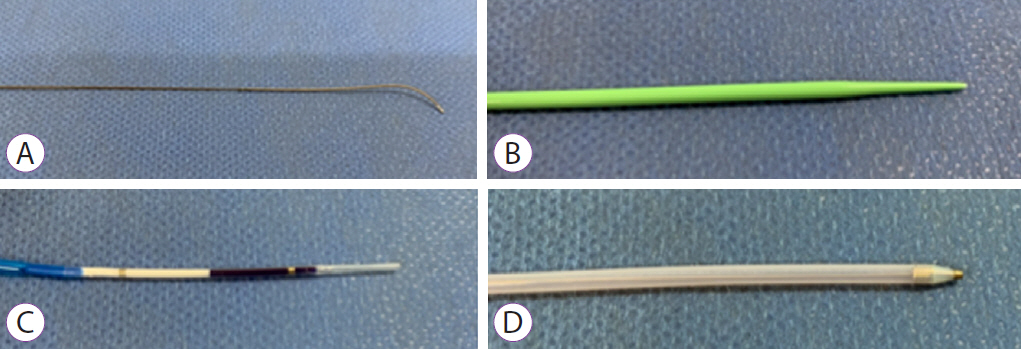
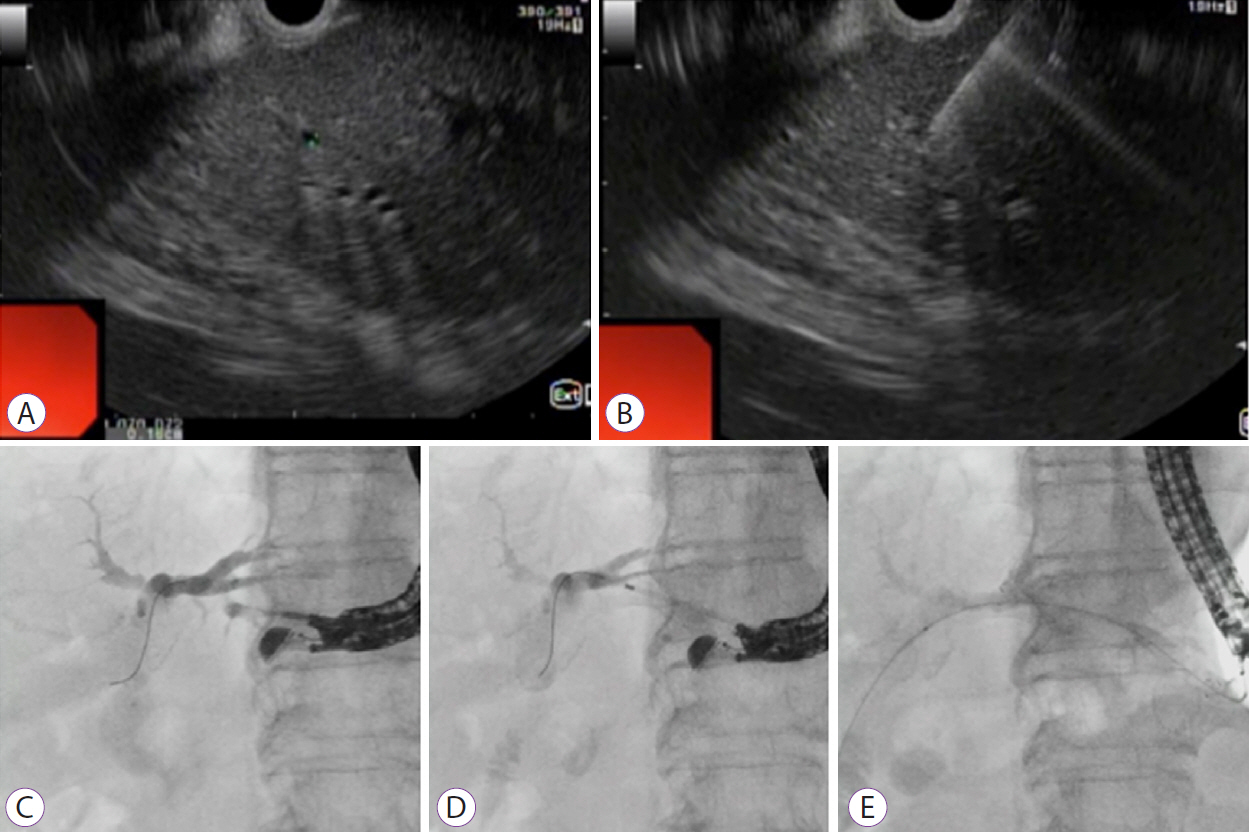
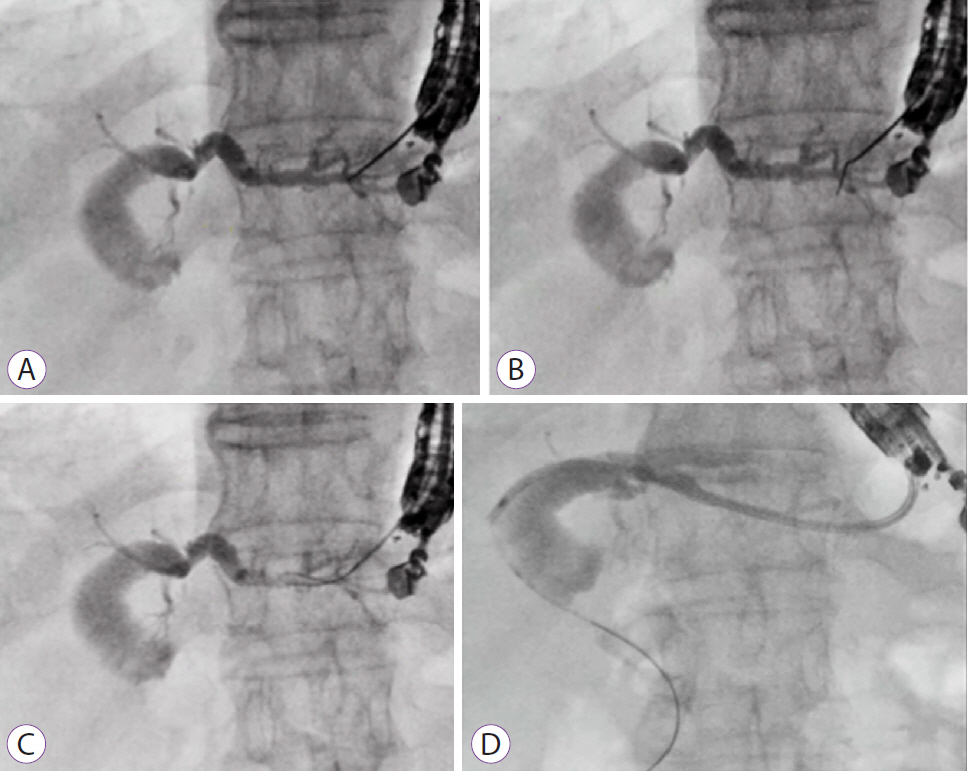
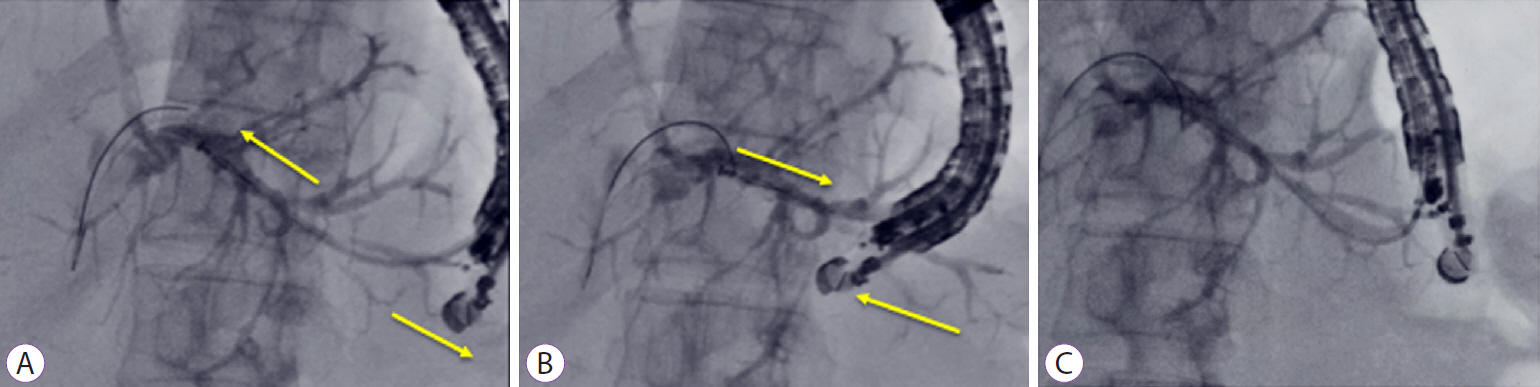
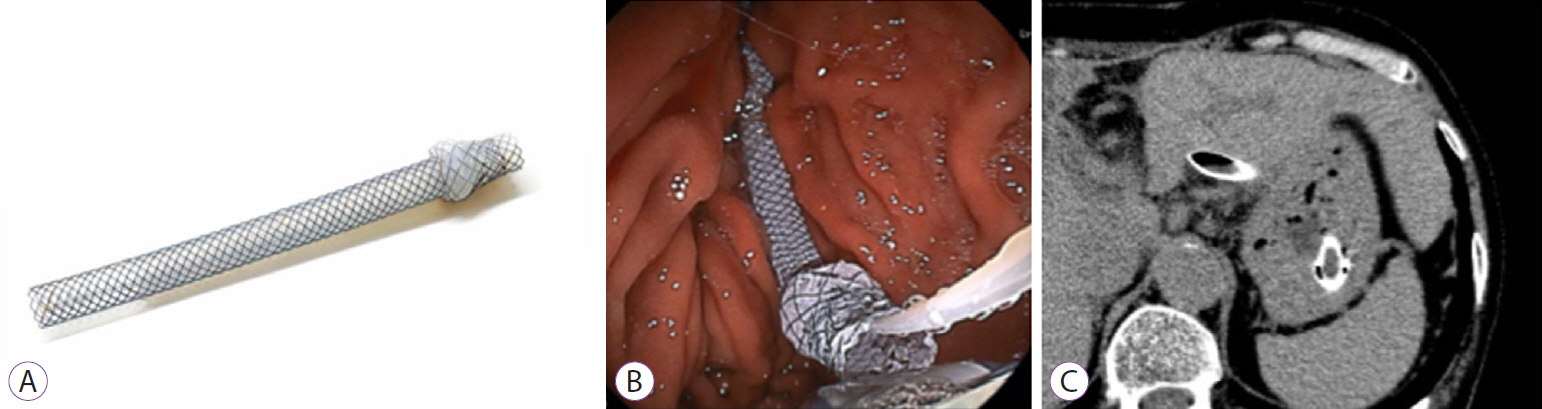
- Endoscopic ultrasound-guided biliary drainage has been developed as an alternative method for biliary drainage. EUS-guided hepaticogastrostomy (EUS-HGS) can be attempted via the trans-gastric route. These procedures are technically complex for two reasons. First, puncture of the intrahepatic bile duct via the trans-gastric route can be more difficult than that by other approaches because of the small diameter of the target site, and guidewire insertion or manipulation is challenging during EUS-HGS. Second, critical adverse events, such as stent migration into the abdominal cavity, could occur because of the greater mobility of the stomach compared to the duodenum. Therefore, endoscopists should be cautious when performing EUS-HGS. An advantage of EUS-HGS is that it can be performed in patients with complications such as duodenal bulb obstruction or surgically altered anatomy. Recent advances in technique and improvements in devices and stents for EUS-HGS have shown promise for improving the technical success rate of EUS-HGS and reducing the rate of adverse events. However, endoscopists should remain aware of the possibility of critical adverse events such as stent migration.
Keyword
Figure
Cited by 2 articles
-
The writing on the wall: self-expandable stents for endoscopic ultrasound-guided hepaticogastrostomy?
Hyung Ku Chon, Shayan Irani, Tae Hyeon Kim
Clin Endosc. 2023;56(6):741-743. doi: 10.5946/ce.2023.207.Hepatobiliary scintigraphy of bile excretion after endoscopic ultrasound-guided hepaticogastrostomy for malignant biliary obstruction: a retrospective study in Japan
Masanori Yamada, Kazuo Hara, Shin Haba, Takamichi Kuwahara, Nozomi Okuno, Yasuhiro Kuraishi, Takafumi Yanaidani, Sho Ishikawa, Tsukasa Yasuda, Toshitaka Fukui
Clin Endosc. 2024;57(6):798-806. doi: 10.5946/ce.2023.291.
Reference
-
1. Park DH, Jang JW, Lee SS, Seo DW, Lee SK, Kim MH. EUS-guided biliary drainage with transluminal stenting after failed ERCP: predictors of adverse events and long-term results. Gastrointest Endosc. 2011; 74:1276–1284.
Article2. Vila JJ, Pérez-Miranda M, Vazquez-Sequeiros E, et al. Initial experience with EUS-guided cholangiopancreatography for biliary and pancreatic duct drainage: a Spanish national survey. Gastrointest Endosc. 2012; 76:1133–1141.
Article3. Poincloux L, Rouquette O, Buc E, et al. Endoscopic ultrasound-guided biliary drainage after failed ERCP: cumulative experience of 101 procedures at a single center. Endoscopy. 2015; 47:794–801.
Article4. Khashab MA, Messallam AA, Penas I, et al. International multicenter comparative trial of transluminal EUS-guided biliary drainage via hepatogastrostomy vs. choledochoduodenostomy approaches. Endosc Int Open. 2016; 4:E175–E181.
Article5. Nakai Y, Isayama H, Yamamoto N, et al. Safety and effectiveness of a long, partially covered metal stent for endoscopic ultrasound-guided hepaticogastrostomy in patients with malignant biliary obstruction. Endoscopy. 2016; 48:1125–1128.
Article6. Minaga K, Takenaka M, Kitano M, et al. Rescue EUS-guided intrahepatic biliary drainage for malignant hilar biliary stricture after failed transpapillary re-intervention. Surg Endosc. 2017; 31:4764–4772.
Article7. Sportes A, Camus M, Greget M, et al. Endoscopic ultrasound-guided hepaticogastrostomy versus percutaneous transhepatic drainage for malignant biliary obstruction after failed endoscopic retrograde cholangiopancreatography: a retrospective expertise-based study from two centers. Therap Adv Gastroenterol. 2017; 10:483–493.
Article8. Oh D, Park DH, Song TJ, et al. Optimal biliary access point and learning curve for endoscopic ultrasound-guided hepaticogastrostomy with transmural stenting. Therap Adv Gastroenterol. 2017; 10:42–53.
Article9. Honjo M, Itoi T, Tsuchiya T, et al. Safety and efficacy of ultra-tapered mechanical dilator for EUS-guided hepaticogastrostomy and pancreatic duct drainage compared with electrocautery dilator (with video). Endosc Ultrasound. 2018; 7:376–382.
Article10. Paik WH, Lee TH, Park DH, et al. EUS-guided biliary drainage versus ERCP for the primary palliation of malignant biliary obstruction: a multicenter randomized clinical trial. Am J Gastroenterol. 2018; 113:987–997.
Article11. Nakai Y, Sato T, Hakuta R, et al. Long-term outcomes of a long, partially covered metal stent for EUS-guided hepaticogastrostomy in patients with malignant biliary obstruction (with video). Gastrointest Endosc. 2020; 92:623–631.e1.
Article12. Krishnamoorthi R, Dasari CS, Thoguluva Chandrasekar V, et al. Effectiveness and safety of EUS-guided choledochoduodenostomy using lumen-apposing metal stents (LAMS): a systematic review and meta-analysis. Surg Endosc. 2020; 34:2866–2877.
Article13. Ogura T, Nishioka N, Ueno S, et al. Effect of echoendoscope angle on success of guidewire manipulation during endoscopic ultrasound-guided hepaticogastrostomy. Endoscopy. 2021; 53:369–375.
Article14. Ma KW, So H, Cho DH, Oh JS, Cheung TT, Park DH. Durability and outcome of endoscopic ultrasound-guided hepaticoduodenostomy using a fully covered metal stent for segregated right intrahepatic duct dilatation. J Gastroenterol Hepatol. 2020; 35:1753–1760.
Article15. Ogura T, Kitano M, Takenaka M, et al. Multicenter prospective evaluation study of endoscopic ultrasound-guided hepaticogastrostomy combined with antegrade stenting (with video). Dig Endosc. 2018; 30:252–259.
Article16. Amano M, Ogura T, Onda S, et al. Prospective clinical study of endoscopic ultrasound-guided biliary drainage using novel balloon catheter (with video). J Gastroenterol Hepatol. 2017; 32:716–720.
Article17. Ogura T, Nakai Y, Iwashita T, Higuchi K, Itoi T. Novel fine gauge electrocautery dilator for endoscopic ultrasound-guided biliary drainage: experimental and clinical evaluation study (with video). Endosc Int Open. 2019; 7:E1652–E1657.
Article18. Ogura T, Masuda D, Takeuchi T, Fukunishi S, Higuchi K. Liver impaction technique to prevent shearing of the guidewire during endoscopic ultrasound-guided hepaticogastrostomy. Endoscopy. 2015; 47:E583–E584.
Article19. Kwon CI, Koh DH, Song TJ, Park WS, Lee DH, Jeong S. Technical reports of endoscopic retrograde cholangiopancreatography guidewires on the basis of physical properties. Clin Endosc. 2020; 53:65–72.
Article20. Ryou M, Benias PC, Kumbhari V. Initial clinical experience of a steerable access device for EUS-guided biliary drainage. Gastrointest Endosc. 2020; 91:178–184.
Article21. Miyano A, Ogura T, Yamamoto K, Okuda A, Nishioka N, Higuchi K. Clinical impact of the intra-scope channel stent release technique in preventing stent migration during EUS-guided hepaticogastrostomy. J Gastrointest Surg. 2018; 22:1312–1318.
Article22. Cho DH, Lee SS, Oh D, et al. Long-term outcomes of a newly developed hybrid metal stent for EUS-guided biliary drainage (with videos). Gastrointest Endosc. 2017; 85:1067–1075.
Article23. Maehara K, Hijioka S, Sakamoto T, et al. Novel biliary drainage of a choledochojejunal anastomotic stenosis using a double-balloon endoscope and forward-viewing endoscopic ultrasound. Endoscopy. 2021; 53:E242–E244.
Article24. Ogura T, Yamada M, Nishioka N, Yamada T, Higuchi K. One-step stent deployment of EUS-guided hepaticogastrostomy using a novel covered metal stent with a fine-gauge stent delivery system (with video). Endosc Ultrasound. 2020; 9:267–269.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Endoscopic Ultrasound-Guided Hepaticogastrostomy: Technical Review and Tips to Prevent Adverse Events
- Recent development of endoscopic ultrasound-guided biliary drainage
- Follow-up computed tomography can prevent stent migration after endoscopic ultrasound-guided hepaticogastrostomy
- Endoscopic ultrasound-guided hepaticogastrostomy by puncturing both B2 and B3: a single center experience
- Endoscopic Ultrasound-Guided Biliary Drainage