Korean Circ J.
2024 Jul;54(7):398-406. 10.4070/kcj.2024.0084.
Optimal Dose of Edoxaban for Very Elderly Atrial Fibrillation Patients at High Risk of Bleeding: The LEDIOS Registry
- Affiliations
-
- 1Division of Cardiology, Department of Internal Medicine, Heart Vascular and Stroke Institute, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea
- 2Division of Cardiology, Hallym University Sacred Heart Hospital, Anyang, Korea
- 3Department of Cardiology, Busan Paik Hospital, Inje University College of Medicine, Busan, Korea
- 4Division of Cardiology, Department of Internal Medicine, Gachon University Gil Medical Center, Incheon, Korea
- 5Division of Cardiology, Department of Internal Medicine, Kangbuk Samsung Hospital, Sungkyunkwan University College of Medicine, Seoul, Korea
- 6Department of Cardiology, Dong-A University Hospital, Busan, Korea
- KMID: 2557979
- DOI: http://doi.org/10.4070/kcj.2024.0084
Abstract
- Background and Objectives
Optimal anticoagulation in very elderly patients is challenging due to the high risk of anticoagulant-induced bleeding. The aim of this study was to assess outcomes of on-label reduced-dose edoxaban (30 mg) in very elderly patients who had additional risk factors for bleeding.
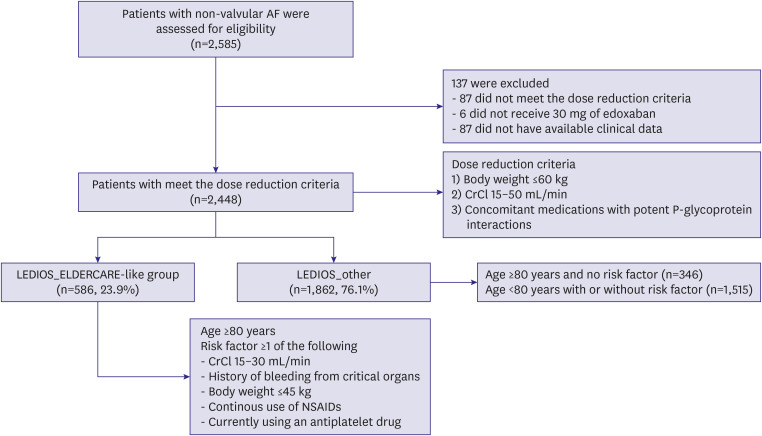
Methods
This was a multi-center, prospective, non-interventional observational study to evaluate the efficacy and safety of on-label reduced-dose edoxaban in atrial fibrillation (AF) patients 80 years of age or older and who had more than 1 risk factor for bleeding.
Results
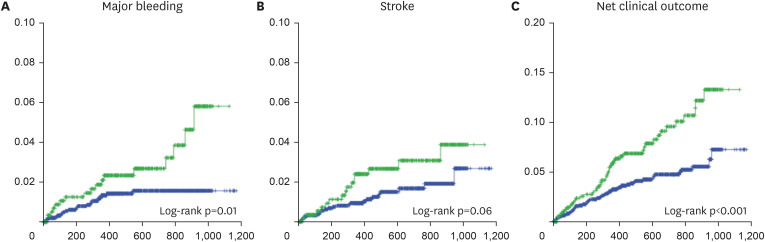
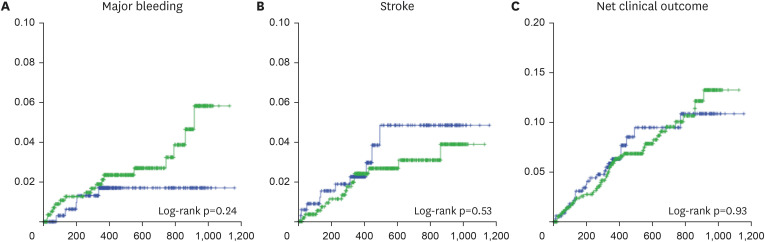
A total of 2448 patients (mean age 75.0±8.3 years, 801 [32.7%] males) was included in the present study, and 586 (23.9%) were 80 years of age or older with additional risk factors for bleeding. Major bleeding events occurred frequently among very elderly AF patients who had additional bleeding risk factors compared to other patients (unadjusted hazard ratio [HR], 2.16; 95% confidence interval [CI], 1.16–4.02); however, there were no significant differences in stroke incidence (HR, 1.86; 95% CI, 0.98–3.55). There were no significant differences for either factor after adjusting for age and sex (adjusted HR, 1.65; 95% CI, 0.75–3.62 for major bleeding; adjusted HR, 1.13; 95% CI, 0.51–2.50 for stroke).
Conclusions
In very elderly AF patients with comorbidities associated with greater risk of bleeding, the incidence of major bleeding events was significantly increased. In addition, risk of stroke showed tendency to increase in same population. Effective anticoagulation therapy might be important in these high-risk population, and close observation of bleeding events might also be required.
Keyword
Figure
Cited by 1 articles
-
What Is a Balanced Way of Anticoagulation for Efficacy and Safety in High-Risk Elderly Patients With Atrial Fibrillation?
Daehoon Kim
Korean Circ J. 2024;54(7):407-408. doi: 10.4070/kcj.2024.0170.
Reference
-
1. Yamashita T, Suzuki S, Inoue H, et al. Two-year outcomes of more than 30 000 elderly patients with atrial fibrillation: results from the All Nippon AF In the Elderly (ANAFIE) registry. Eur Heart J Qual Care Clin Outcomes. 2022; 8:202–213. PMID: 33822030.
Article2. Chao TF, Chiang CE, Liao JN, Chen TJ, Lip GY, Chen SA. Comparing the effectiveness and safety of nonvitamin k antagonist oral anticoagulants and warfarin in elderly Asian patients with atrial fibrillation: a nationwide cohort study. Chest. 2020; 157:1266–1277. PMID: 31809694.3. Henrard S, Vandenabeele C, Marien S, Boland B, Dalleur O. Underuse of anticoagulation in older patients with atrial fibrillation and CHADS2 score ≥ 2: are we doing better since the marketing of direct oral anticoagulants? Drugs Aging. 2017; 34:841–850. PMID: 29086350.4. Akao M, Chun YH, Esato M, et al. Inappropriate use of oral anticoagulants for patients with atrial fibrillation. Circ J. 2014; 78:2166–2172. PMID: 24976391.5. Okumura K, Akao M, Yoshida T, et al. Low-dose edoxaban in very elderly patients with atrial fibrillation. N Engl J Med. 2020; 383:1735–1745. PMID: 32865374.6. Giugliano RP, Ruff CT, Braunwald E, et al. Edoxaban versus warfarin in patients with atrial fibrillation. N Engl J Med. 2013; 369:2093–2104. PMID: 24251359.7. Steffel J, Ruff CT, Yin O, et al. Randomized, double-blind comparison of half-dose versus full-dose edoxaban in 14,014 patients with atrial fibrillation. J Am Coll Cardiol. 2021; 77:1197–1207. PMID: 33663737.8. Kim JY, Choi EK, Lim HE, Oh YS, Cho Y, On YK. Outcomes of on-label reduced-dose edoxaban in patients with atrial fibrillation: the LEDIOS registry. J Korean Med Sci. 2022; 37:e335. PMID: 36513051.
Article9. Schulman S, Kearon C. Subcommittee on Control of Anticoagulation of the Scientific and Standardization Committee of the International Society on Thrombosis and Haemostasis. Definition of major bleeding in clinical investigations of antihemostatic medicinal products in non-surgical patients. J Thromb Haemost. 2005; 3:692–694. PMID: 15842354.
Article10. Steffel J, Collins R, Antz M, et al. 2021 European Heart Rhythm Association practical guide on the use of non-vitamin k antagonist oral anticoagulants in patients with atrial fibrillation. Europace. 2021; 23:1612–1676. PMID: 33895845.11. Lee SR, Lee YS, Park JS, et al. Label adherence for non-vitamin K antagonist oral anticoagulants in a prospective cohort of Asian patients with atrial fibrillation. Yonsei Med J. 2019; 60:277–284. PMID: 30799590.12. Vranckx P, Valgimigli M, Eckardt L, et al. Edoxaban-based versus vitamin K antagonist-based antithrombotic regimen after successful coronary stenting in patients with atrial fibrillation (ENTRUST-AF PCI): a randomised, open-label, phase 3b trial. Lancet. 2019; 394:1335–1343. PMID: 31492505.13. Chao TF, Chiang CE, Chan YH, et al. Oral anticoagulants in extremely-high-risk, very elderly (>90 years) patients with atrial fibrillation. Heart Rhythm. 2021; 18:871–877. PMID: 33640447.
Article14. Tsai CT, Liao JN, Chen SJ, Jiang YR, Chen TJ, Chao TF. Non-vitamin K antagonist oral anticoagulants versus warfarin in AF patients ≥ 85 years. Eur J Clin Invest. 2021; 51:e13488. PMID: 33420738.
Article15. Chan YH, Lee HF, See LC, et al. Effectiveness and safety of four direct oral anticoagulants in Asian patients with nonvalvular atrial fibrillation. Chest. 2019; 156:529–543. PMID: 31103697.
Article16. Brønnum Nielsen P, Larsen TB, Gorst-Rasmussen A, Skjøth F, Rasmussen LH, Lip GY. Intracranial hemorrhage and subsequent ischemic stroke in patients with atrial fibrillation: a nationwide cohort study. Chest. 2015; 147:1651–1658. PMID: 25412369.
Article17. Chao TF, Liu CJ, Liao JN, et al. Use of oral anticoagulants for stroke prevention in patients with atrial fibrillation who have a history of intracranial hemorrhage. Circulation. 2016; 133:1540–1547. PMID: 26969761.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Outcomes of On-Label Reduced-Dose Edoxaban in Patients With Atrial Fibrillation: The LEDIOS Registry
- Hemoptysis in Quadriplegia with Atrial Fibrillation Who Was Taking Edoxaban: a Case Report
- Is Lower-Dose Edoxaban Sufficiently Effective and Safe for the Treatment of Korean Patients With Atrial Fibrillation?
- Increasing Very Low-Dose Edoxaban Prescription: Effectiveness and Safety Data of Korean AF Patients
- Managing high‑risk atrial fibrillation patients with multiple comorbidities