Obstet Gynecol Sci.
2024 Jul;67(4):380-392. 10.5468/ogs.24005.
The influence of advanced maternal age on congenital malformations, short- and long-term outcomes in offspring of nulligravida: a Korean National Cohort Study over 15 years
- Affiliations
-
- 1Department of Obstetrics and Gynecology, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea
- 2Department of Clinical Research Design and Evaluation, Samsung Advanced Institute for Health Science and Technology, Sungkyunkwan University, Seoul, Korea
- 3Center for Clinical Epidemiology, Samsung Medical Center, Seoul, Korea
- KMID: 2557855
- DOI: http://doi.org/10.5468/ogs.24005
Abstract
Objective
To assess the influence of advanced maternal age on congenital malformations, short- and long-term outcomes in offspring of nulligravida.
Methods
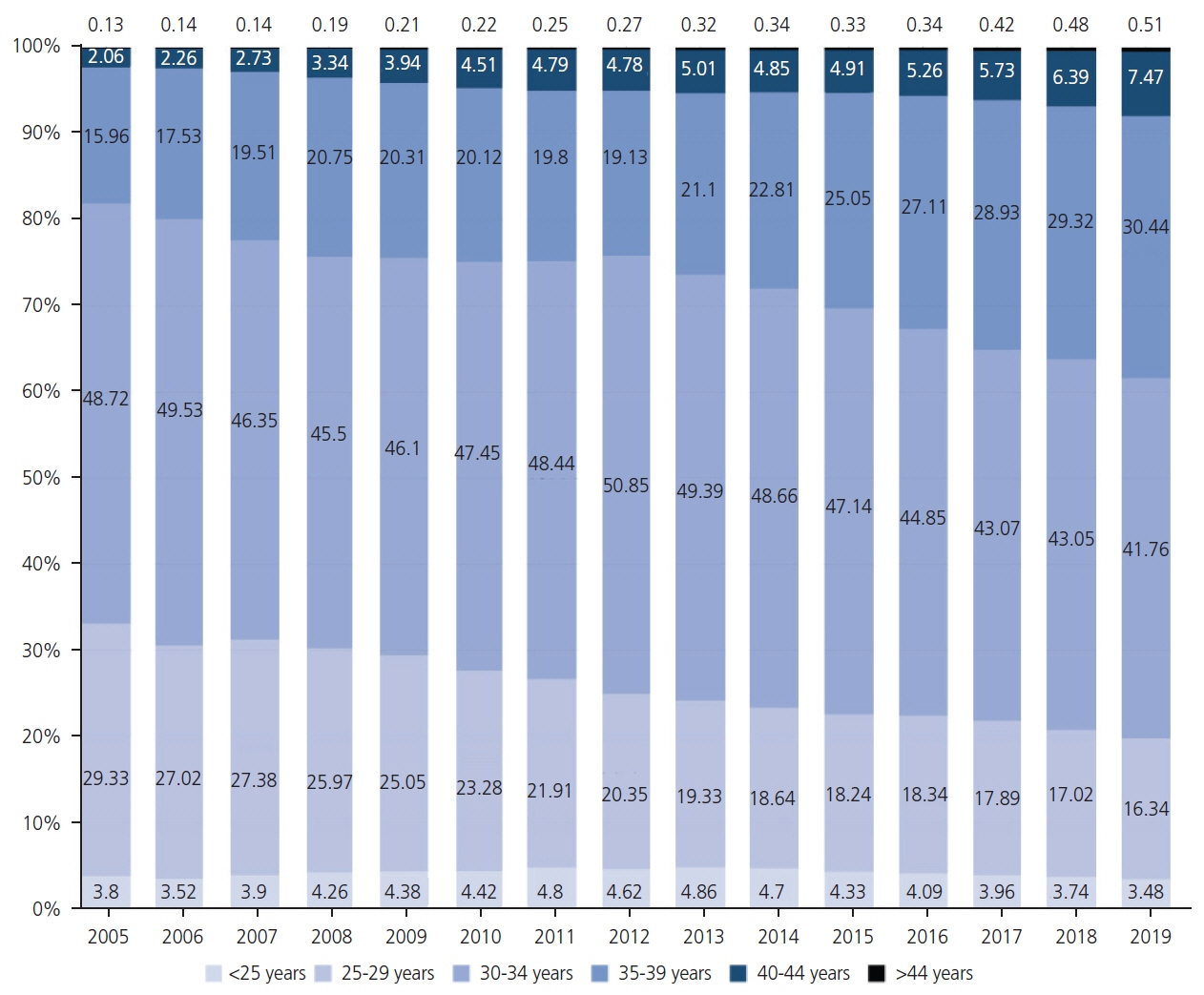
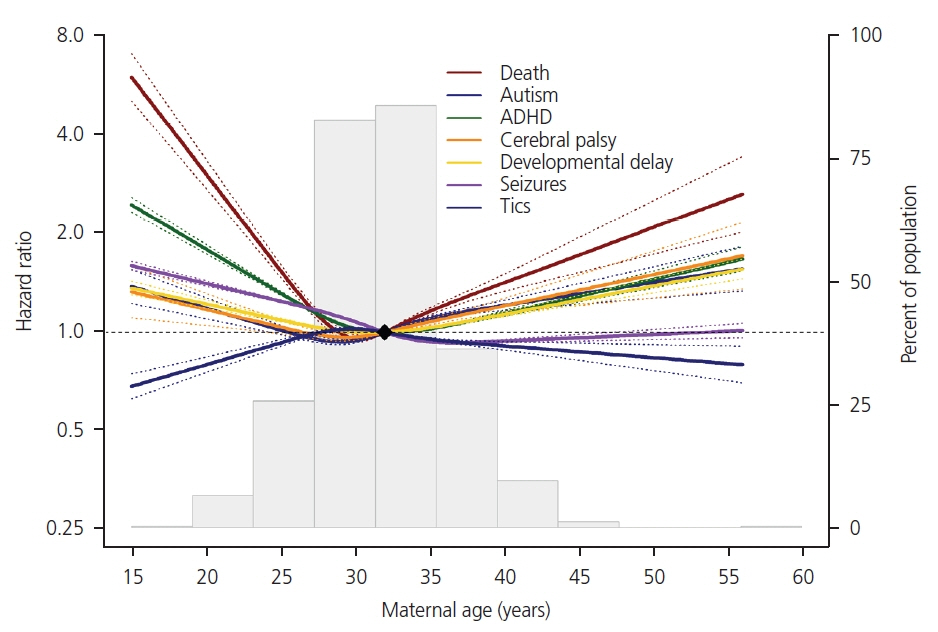
A retrospective study was conducted using the Korean National Health Insurance Service database spanning from January 2005 to December 2019. All live-born offspring of nulligravida (n=3,685,817) were included. The maternal age was subdivided into the following subgroups: <25 years (n=153,818), 25-29 years (n=845,355), 30-34 years (n=1,738,299), 35-39 years (n=787,530), 40-44 years (n=151,519), and >44 years (n=9,296). Outcomes were assessed based on International Classification of Diseases-10 codes. Adjusted odds ratios (aOR) were calculated with the group of 25-29 years as a reference. Result Most congenital malformations showed an age dependent increase, but cleft lip and abdominal wall defect exhibited a U-shape curve, indicating an increase even in those <25 years old. Similarly, various disorders included in the neonatal composite outcomes from short-term outcomes showed aged dependent escalation. However, the preterm birth from the short-term outcome and most of the long-term developmental outcomes, except for motor developmental delay and Tics, showed a U-shaped pattern. The aOR of autism and cerebral palsy, showing the most obvious U-shaped curved in the long-term outcomes, was 1.50 (95% confidence interval [CI], 1.24-1.82) and 1.54 (95% CI, 1.17-2.03), respectively in the group >44 years old and 1.18 (95% CI, 1.11-1.25) and 1.19 (95% CI, 1.09-1.30) in <25 years old group.
Conclusion
Overall, an advanced maternal age has an age-dependent correlation with most congenital malformations and shortand long-term outcomes of neonates.
Figure
Reference
-
References
1. Gantt A, Metz TD, Kuller JA, Louis JM, Cahill AG, Turrentine MA. Obstetric care consensus #11, pregnancy at age 35 years or older. Am J Obstet Gynecol. 2023; 228:B25–40.
Article2. Statistics Korea. Birth statistics in 2021 [Internet]. Daejeon: Statistics Korea;c2022. [cited 2023 Dec 15]. Available from: https://kostat.go.kr/board.es?mid=a20108100000&bid=11773&act=view&list_no=420358.3. Lee KS, Han DH, Bae CW. Changes in statistical birth data related to maternity and newborn over the past 15 years in Korea. Korean J Perinatol. 2011; 3:229–36.4. Kahveci B, Melekoglu R, Evruke IC, Cetin C. The effect of advanced maternal age on perinatal outcomes in nulliparous singleton pregnancies. BMC Pregnancy Childbirth. 2018; 18:343.
Article5. Kim J, Nam JY, Park EC. Advanced maternal age and severe maternal morbidity in South Korea: a population-based cohort study. Sci Rep. 2022; 12:21358.
Article6. Statistics Korea. 2022 movements of population [Internet]. Daejeon: Statistics Korea;c2023. [cited 2023 Dec 15]. Available from: https://kosis.kr/upsHtml/online.do?isOnline=Y&PART=G&pubcode=CC&isNew=Y&dev=Y#gongDiv_CC.7. Koo YJ, Ryu HM, Yang JH, Lim JH, Lee JE, Kim MY, et al. Pregnancy outcomes according to increasing maternal age. Taiwan J Obstet Gynecol. 2012; 51:60–5.
Article8. Machado-Gédéon A, Badeghiesh A, Baghlaf H, Dahan MH. Adverse pregnancy, delivery and neonatal outcomes across different advanced maternal ages: a population-based retrospective cohort study. Eur J Obstet Gynecol Reprod Biol X. 2023; 17:100180.
Article9. Kim D, Yang PS, You SC, Sung JH, Jang E, Yu HT, et al. Treatment timing and the effects of rhythm control strategy in patients with atrial fibrillation: nationwide cohort study. BMJ. 2021; 373:n991.10. Chun CB, Kim SY, Lee JY, Lee SY. Republic of Korea: health system review. Health Systems in Transition. 2009; 11:7.11. EUROCAT. EUROCAT guide 1.4: instruction for the registration of congenital anomalies [Internet]. Coleraine: University of Ulster; c2013 [cited 2024 Apr 30]. Available from: https://eu-rd-platform.jrc.ec.europa.eu/sites/default/files/Full_Guide_1_4_version_28_DEC2018.pdf.12. Noh Y, Lee H, Choi A, Kwon JS, Choe SA, Chae J, et al. First-trimester exposure to benzodiazepines and risk of congenital malformations in offspring: a population-based cohort study in South Korea. PLoS Med. 2022; 19:e1003945.
Article13. Lee J, Lee JS, Park SH, Shin SA, Kim K. Cohort profile: The National Health Insurance Service-National Sample Cohort (NHIS-NSC), South Korea. Int J Epidemiol. 2017; 46:e15.
Article14. Shin DW, Cho B, Guallar E. Korean National Health Insurance database. JAMA Intern Med. 2016; 176:138.
Article15. Kimm H, Yun JE, Lee SH, Jang Y, Jee SH. Validity of the diagnosis of acute myocardial infarction in korean national medical health insurance claims data: the korean heart study (1). Korean Circ J. 2012; 42:10–5.16. Charlson ME, Pompei P, Ales KL, MacKenzie CR. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis. 1987; 40:373–83.
Article17. Kim KH. Comparative study on three algorithms of the ICD-10 Charlson comorbidity index with myocardial infarction patients. J Prev Med Public Health. 2010; 43:42–9.
Article18. Lee SY. The 2018 national survey on fertility and family health and welfare [Internet]. Sejong: Korea Institute for Health and Social Affairs;c2019. [cited 2023 Dec 15]. Available from: https://www.kihasa.re.kr/en/publish/paper/research/view?seq=30703.19. Svensson E, Ehrenstein V, Nørgaard M, Bakketeig LS, Rothman KJ, Sørensen HT, et al. Estimating the proportion of all observed birth defects occurring in pregnancies terminated by a second-trimester abortion. Epidemiology. 2014; 25:866–71.
Article20. Khalife D, Nassar A, Khalil A, Awwad J, Abu Musa A, Hannoun A, et al. Cumulative live-birth rates by maternal age after one or multiple in vitro fertilization cycles: an institutional experience. Int J Fertil Steril. 2020; 14:34–40.21. Belcher RH, Patel SA, Kynes M, Carlucci JG, Hodson E, Zhao S, et al. Demographics and trends of cleft lip and palate patients born in Tennessee from 2000 to 2017. Int J Pediatr Otorhinolaryngol. 2022; 163:111312.
Article22. Martelli DR, Cruz KW, Barros LM, Silveira MF, Swerts MS, Martelli Júnior H. Maternal and paternal age, birth order and interpregnancy interval evaluation for cleft lip-palate. Braz J Otorhinolaryngol. 2010; 76:107–12.23. Wu Y, Li M, Zhang J, Wang S. Unveiling uterine aging: much more to learn. Ageing Res Rev. 2023; 86:101879.
Article24. Wooldridge AL, Pasha M, Chitrakar P, Kirschenman R, Quon A, Spaans F, et al. Advanced maternal age impairs uterine artery adaptations to pregnancy in rats. Int J Mol Sci. 2022; 23:9191.
Article25. Office for National Statistics. Birth characteristics in England and Wales: 2021 [Internet]. London: Office for National Statistics;c2023. [cited 2024 Apr 31]. Available from: https://www.ons.gov.uk/peoplepopulationandcommunity/birthsdeathsandmarriages/livebirths/bulletins/birthcharacteristicsinenglandandwales/2021.26. Bai J, Wong FW, Bauman A, Mohsin M. Parity and pregnancy outcomes. Am J Obstet Gynecol. 2002; 186:274–8.
Article27. Yimer NB, Gedefaw A, Tenaw Z, Liben ML, Meikena HK, Amano A, et al. Adverse obstetric outcomes in public hospitals of southern Ethiopia: the role of parity. J Matern Fetal Neonatal Med. 2022; 35:1915–22.
Article28. McCarthy FP, Moss-Morris R, Khashan AS, North RA, Baker PN, Dekker G, et al. Previous pregnancy loss has an adverse impact on distress and behaviour in subsequent pregnancy. BJOG. 2015; 122:1757–64.
Article29. van Oppenraaij RH, Jauniaux E, Christiansen OB, Horcajadas JA, Farquharson RG, Exalto N. Predicting adverse obstetric outcome after early pregnancy events and complications: a review. Hum Reprod Update. 2009; 15:409–21.
Article30. Couto ER, Couto E, Vian B, Gregório Z, Nomura ML, Zaccaria R, et al. Quality of life, depression and anxiety among pregnant women with previous adverse pregnancy outcomes. Sao Paulo Med J. 2009; 127:185–9.31. Chang Z, Lichtenstein P, D’Onofrio BM, Almqvist C, Kuja-Halkola R, Sjölander A, et al. Maternal age at childbirth and risk for ADHD in offspring: a population-based cohort study. Int J Epidemiol. 2014; 43:1815–24.
Article32. Croen LA, Najjar DV, Fireman B, Grether JK. Maternal and paternal age and risk of autism spectrum disorders. Arch Pediatr Adolesc Med. 2007; 161:334–40.
Article33. Sandin S, Hultman CM, Kolevzon A, Gross R, Mac-Cabe JH, Reichenberg A. Advancing maternal age is associated with increasing risk for autism: a review and meta-analysis. J Am Acad Child Adolesc Psychiatry. 2012; 51:477–86.e1.
Article34. Choi YJ, Jung JY, Kim JH, Kwon H, Park JW, Kwak YH, et al. Febrile seizures: are they truly benign? Longitudinal analysis of risk factors and future risk of afebrile epileptic seizure based on the national sample cohort in South Korea, 2002-2013. Seizure. 2019; 64:77–83.
Article35. Green RF, Devine O, Crider KS, Olney RS, Archer N, Olshan AF, et al. Association of paternal age and risk for major congenital anomalies from the National Birth Defects Prevention Study, 1997 to 2004. Ann Epidemiol. 2010; 20:241–9.36. Mac Bird T, Robbins JM, Druschel C, Cleves MA, Yang S, Hobbs CA. Demographic and environmental risk factors for gastroschisis and omphalocele in the National Birth Defects Prevention Study. J Pediatr Surg. 2009; 44:1546–51.
Article37. Roeckner JT, Bennett S, Mitta M, Sanchez-Ramos L, Kaunitz AM. Pregnancy outcomes associated with an abnormal 50-g glucose screen during pregnancy: a systematic review and Meta-analysis. J Matern Fetal Neonatal Med. 2021; 34:4132–40.
Article38. Kim YJ, Lee JE, Kim SH, Shim SS, Cha DH. Maternal age-specific rates of fetal chromosomal abnormalities in Korean pregnant women of advanced maternal age. Obstet Gynecol Sci. 2013; 56:160–6.
Article39. Ko HS, Kwak DW, Oh SY, Choi SK, Hong JS, Hwang HS, et al. Clinical significance of soft markers in second trimester ultrasonography for pregnant Korean women: a multicenter study and literature review. Obstet Gynecol Sci. 2022; 65:145–55.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- The Maternal Obesity: Adverse Outcomes of Pregnancy and the Offspring
- Gestational Diabetes Mellitus: Diagnostic Approaches and Maternal-Offspring Complications
- Association between Maternal Adverse Childhood Experiences and Risk of Post-traumatic Stress Disorder in the Offspring
- Prenatal Factors Influencing Long-Term Neurodevelopmental Outcomes
- Trends in Birth Weight and the Incidence of Low Birth Weight and Advanced Maternal Age in Korea between 1993 and 2016