J Korean Med Sci.
2024 Jul;39(26):e199. 10.3346/jkms.2024.39.e199.
Relationship Between Aspirin Use and Site-Specific Colorectal Cancer Risk Among Individuals With Metabolic Comorbidity
- Affiliations
-
- 1Department of Cancer Biomedical Science, Graduate School of Cancer Science and Policy, National Cancer Center, Goyang, Korea
- 2Center for Colorectal Cancer, National Cancer Center Hospital, National Cancer Center, Goyang, Korea
- 3Department of Preventive Medicine, Seoul National University College of Medicine, Seoul, Korea
- KMID: 2557774
- DOI: http://doi.org/10.3346/jkms.2024.39.e199
Abstract
- Background
The relationship between aspirin usage and the risk of colorectal cancer (CRC) among individuals with both hypertension (HTN) and diabetes mellitus (DM) remains unclear. This study aims to explore the impact of aspirin use on the site-specific CRC risk in patients with metabolic comorbidity.
Methods
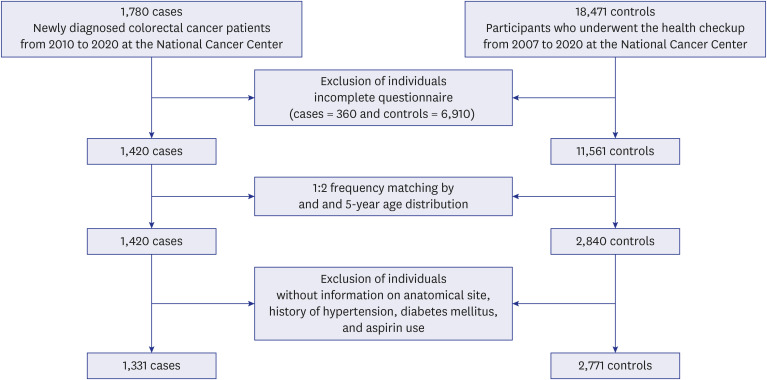
A case-control study was conducted among 1,331 CRC patients and 2,771 controls recruited from the Nation Cancer Center in Korea. Multinomial logistic regression analyses were used to calculate the odds ratios (ORs) and 95% confidence intervals (CIs) for the association between aspirin use, metabolic disease status, and site-specific CRC risk.
Results
Among the 4,102 participants, 1,191 individuals had neither HTN nor DM, 2,044 were diagnosed with HTN, 203 with DM, and 664 presented with HTN and DM comorbidity. An increasing number of HTN and DM was associated with an increased risk of overall CRC (HTN or DM: OR, 1.70; 95% CI, 1.39–2.07; HTN and DM: OR, 8.43; 95% CI, 6.37–11.16), while aspirin use was associated with a decreased risk of overall CRC (OR, 0.31; 95% CI, 0.21–0.46). These results remained consistent across anatomical sites. Among individuals with HTN and DM comorbidity, aspirin use notably associated with lower risk of overall CRC (OR, 0.39; 95% CI, 0.21–0.72), proximal colon (OR, 0.32; 95% CI, 0.13–0.71) and rectal cancer (OR, 0.27; 95% CI, 0.08–0.97), but not distal colon cancer (OR, 0.58; 95% CI, 0.27–1.24).
Conclusion
This study showed that aspirin use is negatively associated with overall and sitespecific CRC, even among individuals with HTN and DM comorbidity.
Keyword
Figure
Reference
-
1. Rawla P, Sunkara T, Barsouk A. Epidemiology of colorectal cancer: incidence, mortality, survival, and risk factors. Prz Gastroenterol. 2019; 14(2):89–103. PMID: 31616522.2. Onyoh EF, Hsu WF, Chang LC, Lee YC, Wu MS, Chiu HM. The rise of colorectal cancer in Asia: epidemiology, screening, and management. Curr Gastroenterol Rep. 2019; 21(8):36. PMID: 31289917.3. Byun JY, Yoon SJ, Oh IH, Kim YA, Seo HY, Lee YH. Economic burden of colorectal cancer in Korea. J Prev Med Public Health. 2014; 47(2):84–93. PMID: 24744825.4. Demb J, Earles A, Martínez ME, Bustamante R, Bryant AK, Murphy JD, et al. Risk factors for colorectal cancer significantly vary by anatomic site. BMJ Open Gastroenterol. 2019; 6(1):e000313.5. Brenner H, Chen C. The colorectal cancer epidemic: challenges and opportunities for primary, secondary and tertiary prevention. Br J Cancer. 2018; 119(7):785–792. PMID: 30287914.6. Cho YA, Lee J, Oh JH, Chang HJ, Sohn DK, Shin A, et al. Genetic Risk Score, Combined Lifestyle Factors and Risk of Colorectal Cancer. Cancer Res Treat. 2019; 51(3):1033–1040. PMID: 30336659.7. Toma M, Beluşică L, Stavarachi M, Apostol P, Spandole S, Radu I, et al. Rating the environmental and genetic risk factors for colorectal cancer. J Med Life. 2012; 5(Spec Issue):152–159. PMID: 31803304.8. Cho S, Shin A. Population attributable fraction of established modifiable risk factors on colorectal cancer in Korea. Cancer Res Treat. 2021; 53(2):480–486. PMID: 33070559.9. Johnson CM, Wei C, Ensor JE, Smolenski DJ, Amos CI, Levin B, et al. Meta-analyses of colorectal cancer risk factors. Cancer Causes Control. 2013; 24(6):1207–1222. PMID: 23563998.10. O’Sullivan DE, Sutherland RL, Town S, Chow K, Fan J, Forbes N, et al. Risk factors for early-onset colorectal cancer: a systematic review and meta-analysis. Clin Gastroenterol Hepatol. 2022; 20(6):1229–1240.e5. PMID: 33524598.11. Aune D, Lau R, Chan DS, Vieira R, Greenwood DC, Kampman E, et al. Dairy products and colorectal cancer risk: a systematic review and meta-analysis of cohort studies. Ann Oncol. 2012; 23(1):37–45. PMID: 21617020.12. Chan AT, Giovannucci EL, Meyerhardt JA, Schernhammer ES, Curhan GC, Fuchs CS. Long-term use of aspirin and nonsteroidal anti-inflammatory drugs and risk of colorectal cancer. JAMA. 2005; 294(8):914–923. PMID: 16118381.13. Maniewska J, Jeżewska D. Non-steroidal anti-inflammatory drugs in colorectal cancer chemoprevention. Cancers (Basel). 2021; 13(4):594. PMID: 33546238.14. Bosetti C, Santucci C, Gallus S, Martinetti M, La Vecchia C. Aspirin and the risk of colorectal and other digestive tract cancers: an updated meta-analysis through 2019. Ann Oncol. 2020; 31(5):558–568. PMID: 32272209.15. Drew DA, Chan AT. Aspirin in the prevention of colorectal neoplasia. Annu Rev Med. 2021; 72(1):415–430. PMID: 33035431.16. Ma S, Han T, Sun C, Cheng C, Zhang H, Qu G, et al. Does aspirin reduce the incidence, recurrence, and mortality of colorectal cancer? A meta-analysis of randomized clinical trials. Int J Colorectal Dis. 2021; 36(8):1653–1666. PMID: 33594505.17. Nounu A, Richmond RC, Stewart ID, Surendran P, Wareham NJ, Butterworth A, et al. Salicylic acid and risk of colorectal cancer: a two-sample Mendelian randomization study. Nutrients. 2021; 13(11):4164. PMID: 34836419.18. Cao Y, Nishihara R, Wu K, Wang M, Ogino S, Willett WC, et al. Population-wide impact of long-term use of aspirin and the risk for cancer. JAMA Oncol. 2016; 2(6):762–769. PMID: 26940135.19. Guo CG, Ma W, Drew DA, Cao Y, Nguyen LH, Joshi AD, et al. Aspirin use and risk of colorectal cancer among older adults. JAMA Oncol. 2021; 7(3):428–435. PMID: 33475710.20. Lin HD, Vora P, Soriano-Gabarró M, Chan KA. Association between low-dose aspirin use and colorectal cancer incidence in Taiwan. JAMA Netw Open. 2020; 3(11):e2026494. PMID: 33211109.21. Wang SY, Zhang WS, Jiang CQ, Jin YL, Zhu T, Zhu F, et al. Association of measures of glucose metabolism with colorectal cancer risk in older Chinese: a 13-year follow-up of the Guangzhou Biobank Cohort Study-Cardiovascular Disease Substudy and meta-analysis. Diabetes Metab J. 2024; 48(1):134–145. PMID: 38173369.22. Jung KJ, Kim MT, Jee SH. Impaired fasting glucose, single-nucleotide polymorphisms, and risk for colorectal cancer in Koreans. Epidemiol Health. 2016; 38:e2016002. PMID: 26797220.23. An S, Ahn C, Jang J, Lee J, Kang D, Lee JK, et al. Comparison of the prevalence of cardiometabolic disorders and comorbidities in Korea and the United States: analysis of the national health and nutrition examination survey. J Korean Med Sci. 2022; 37(18):e149. PMID: 35535376.24. Fowler H, Belot A, Ellis L, Maringe C, Luque-Fernandez MA, Njagi EN, et al. Comorbidity prevalence among cancer patients: a population-based cohort study of four cancers. BMC Cancer. 2020; 20(1):2. PMID: 31987032.25. Chen H, Zheng X, Zong X, Li Z, Li N, Hur J, et al. Metabolic syndrome, metabolic comorbid conditions and risk of early-onset colorectal cancer. Gut. 2021; 70(6):1147–1154. PMID: 33037055.26. Han F, Wu G, Zhang S, Zhang J, Zhao Y, Xu J. The association of metabolic syndrome and its components with the incidence and survival of colorectal cancer: a systematic review and meta-analysis. Int J Biol Sci. 2021; 17(2):487–497. PMID: 33613107.27. Jin EH, Han K, Lee DH, Shin CM, Lim JH, Choi YJ, et al. Association between metabolic syndrome and the risk of colorectal cancer diagnosed before age 50 years according to tumor location. Gastroenterology. 2022; 163(3):637–648.e2. PMID: 35643169.28. Lin CC, Lai MS, Shau WY. Can aspirin reduce the risk of colorectal cancer in people with diabetes? A population-based cohort study. Diabet Med. 2015; 32(3):324–331. PMID: 25252097.29. Shami JJ, Yan VK, Wei Y, Alwafi H, Blais JE, Wan E, et al. Low-dose aspirin does not lower the risk of colorectal cancer in patients with type 2 diabetes taking metformin. J Intern Med. 2023; 293(3):371–383. PMID: 36382924.30. Whelton PK, Carey RM, Aronow WS, Casey DE Jr, Collins KJ, Dennison Himmelfarb C, et al. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA guideline for the prevention, detection, evaluation, and management of high blood pressure in adults: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. J Am Coll Cardiol. 2018; 71(19):e127–e248. PMID: 29146535.31. An S, Moon S, Park SK. Association of metabolic comorbidity with myocardial infarction in individuals with a family history of cardiovascular disease: a prospective cohort study. BMC Public Health. 2022; 22(1):1992. PMID: 36316766.32. Woo H, Lee J, Lee J, Park JW, Park S, Kim J, et al. Diabetes mellitus and site-specific colorectal cancer risk in Korea: a case-control study. J Prev Med Public Health. 2016; 49(1):45–52. PMID: 26841884.33. Xuan K, Zhao T, Sun C, Patel AS, Liu H, Chen X, et al. The association between hypertension and colorectal cancer: a meta-analysis of observational studies. Eur J Cancer Prev. 2021; 30(1):84–96. PMID: 32039929.34. Yu GH, Li SF, Wei R, Jiang Z. Diabetes and colorectal cancer risk: clinical and therapeutic implications. J Diabetes Res. 2022; 2022:1747326. PMID: 35296101.35. Reuter S, Gupta SC, Chaturvedi MM, Aggarwal BB. Oxidative stress, inflammation, and cancer: how are they linked? Free Radic Biol Med. 2010; 49(11):1603–1616. PMID: 20840865.36. Zhu B, Qu S. The relationship between diabetes mellitus and cancers and its underlying mechanisms. Front Endocrinol (Lausanne). 2022; 13:800995. PMID: 35222270.37. Bardelčíková A, Šoltys J, Mojžiš J. Oxidative stress, inflammation and colorectal cancer: an overview. Antioxidants. 2023; 12(4):901. PMID: 37107276.38. Sankaranarayanan R, Kumar DR, Altinoz MA, Bhat GJ. Mechanisms of colorectal cancer prevention by aspirin-a literature review and perspective on the role of COX-dependent and -independent pathways. Int J Mol Sci. 2020; 21(23):9018. PMID: 33260951.39. McQuillan A, Eikelboom JW. Cyclooxygenase inhibitors and the antiplatelet effects of aspirin. N Engl J Med. 2002; 346(20):1589–1590.40. Greenhough A, Smartt HJ, Moore AE, Roberts HR, Williams AC, Paraskeva C, et al. The COX-2/PGE2 pathway: key roles in the hallmarks of cancer and adaptation to the tumour microenvironment. Carcinogenesis. 2009; 30(3):377–386. PMID: 19136477.41. El-Kenawi AE, El-Remessy AB. Angiogenesis inhibitors in cancer therapy: mechanistic perspective on classification and treatment rationales. Br J Pharmacol. 2013; 170(4):712–729. PMID: 23962094.42. Rothwell PM, Wilson M, Elwin CE, Norrving B, Algra A, Warlow CP, et al. Long-term effect of aspirin on colorectal cancer incidence and mortality: 20-year follow-up of five randomised trials. Lancet. 2010; 376(9754):1741–1750. PMID: 20970847.43. Kuan YC, Huang KW, Lin CL, Luo JC, Kao CH. Effects of aspirin or clopidogrel on colorectal cancer chemoprevention in patients with type 2 diabetes mellitus. Cancers (Basel). 2019; 11(10):1468. PMID: 31569587.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Is height a risk factor for colorectal adenoma?
- Can an Aspirin a Day Keep the Colorectal Cancer Away?
- Risk of malignancies and chemopreventive effect of statin, metformin, and aspirin in Korean patients with ulcerative colitis: a nationwide population-based study
- Regression of colon polyposis after aspirin medication
- Relationship between Metabolic Syndrome and MTHFR Polymorphism in Colorectal Cancer