Cancer Res Treat.
2024 Jul;56(3):885-892. 10.4143/crt.2023.1264.
Bilateral Seminal Vesicle Invasion as a Strong Prognostic Indicator in T3b Prostate Cancer Patients Following Radical Prostatectomy: A Comprehensive, Multicenter, Long-term Follow-up Study
- Affiliations
-
- 1Department of Urology, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Korea
- 2Department of Urology, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea
- 3Department of Urology, Seoul National University Hospital, Seoul, Korea
- 4Department of Urology, Seoul National University Bundang Hospital, Seongnam, Korea
- KMID: 2557675
- DOI: http://doi.org/10.4143/crt.2023.1264
Abstract
- Purpose
Pathologic T3b (pT3b) prostate cancer, characterized by seminal vesicle invasion (SVI), exhibits variable oncological outcomes post–radical prostatectomy (RP). Identifying prognostic factors is crucial for patient-specific management. This study investigates the impact of bilateral SVI on prognosis in pT3b prostate cancer.
Materials and Methods
We evaluated the medical records of a multi-institutional cohort of men who underwent RP for prostate cancer with SVI between 2000 and 2012. Univariate and multivariable analyses were performed using Kaplan-Meier analysis and covariate-adjusted Cox proportional hazard regression for biochemical recurrence (BCR), clinical progression (CP), and cancer-specific survival (CSS).
Results
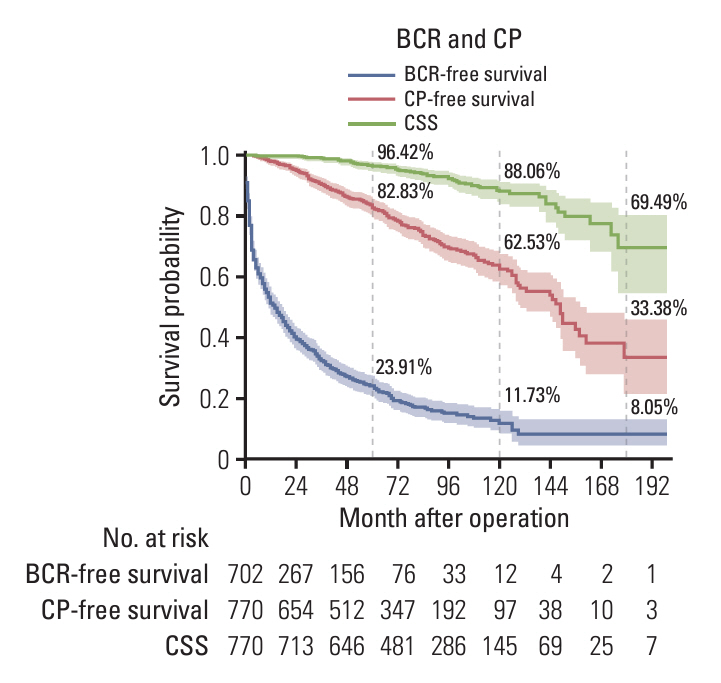
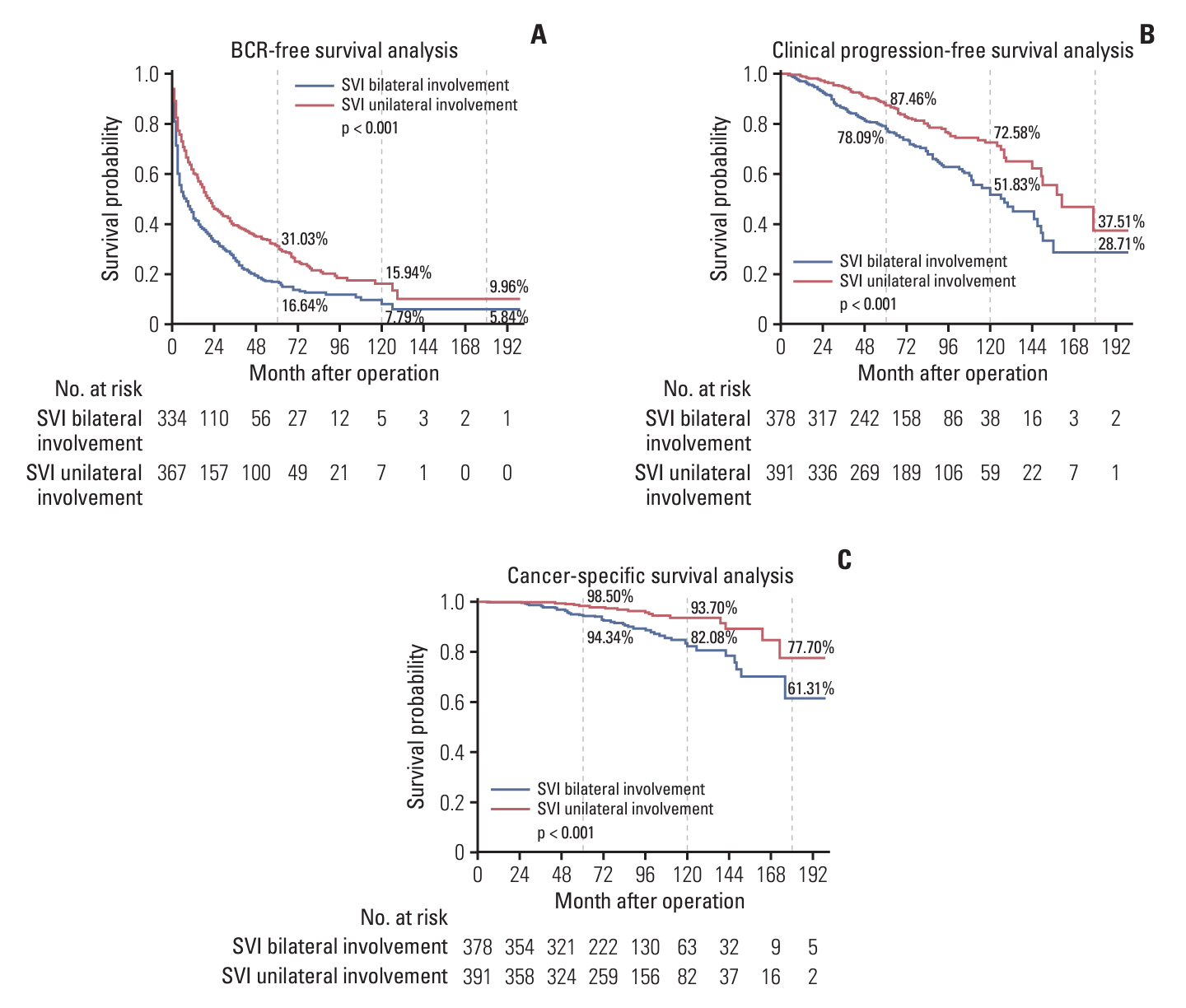
Among 770 men who underwent RP without neo-adjuvant treatment, median follow-up was 85.7 months. Patients with bilateral SVI had higher preoperative prostate-specific antigen levels and clinical T category (all p < 0.001). Extracapsular extension, tumor volume, lymph node metastasis (p < 0.001), pathologic Gleason grade group (p < 0.001), and resection margin positivity (p < 0.001) were also higher in patients with bilateral SVI. The 5-, 10-, and 15-year BCR-free survival rates were 23.9%, 11.7%, and 8.5%; CP-free survival rates were 82.8%, 62.5%, and 33.4%; and CSS rates were 96.4%, 88.1%, and 69.5%, respectively. The bilateral SVI group demonstrated significantly lower BCR-free survival rates, CP-free survival rates, and CSS rates (all p < 0.001). Bilateral SVI was independently associated with BCR (hazard ratio, 1.197; 95% confidence interval, p=0.049), CP (p=0.022), and CSS (p=0.038) in covariate-adjusted Cox regression.
Conclusion
Bilateral SVI is a robust, independent prognostic factor for poor oncological outcomes in pT3b prostate cancer.
Figure
Reference
-
References
1. Culp MB, Soerjomataram I, Efstathiou JA, Bray F, Jemal A. Recent global patterns in prostate cancer incidence and mortality rates. Eur Urol. 2020; 77:38–52.
Article2. Buhmeida A, Pyrhonen S, Laato M, Collan Y. Prognostic factors in prostate cancer. Diagn Pathol. 2006; 1:4.
Article3. Mukamel E, deKernion JB, Hannah J, Smith RB, Skinner DG, Goodwin WE. The incidence and significance of seminal vesicle invasion in patients with adenocarcinoma of the prostate. Cancer. 1987; 59:1535–8.
Article4. Goupy F, Supiot S, Pasquier D, Latorzeff I, Schick U, Monpetit E, et al. Intensity-modulated radiotherapy for prostate cancer with seminal vesicle involvement (T3b): a multicentric retrospective analysis. PLoS One. 2019; 14:e0210514.
Article5. Pierorazio PM, Ross AE, Schaeffer EM, Epstein JI, Han M, Walsh PC, et al. A contemporary analysis of outcomes of adenocarcinoma of the prostate with seminal vesicle invasion (pT3b) after radical prostatectomy. J Urol. 2011; 185:1691–7.6. Mikel Hubanks J, Boorjian SA, Frank I, Gettman MT, Houston Thompson R, Rangel LJ, et al. The presence of extracapsular extension is associated with an increased risk of death from prostate cancer after radical prostatectomy for patients with seminal vesicle invasion and negative lymph nodes. Urol Oncol. 2014; 32:26.
Article7. Secin FP, Bianco FJ Jr, Vickers AJ, Reuter V, Wheeler T, Fearn PA, et al. Cancer-specific survival and predictors of prostate-specific antigen recurrence and survival in patients with seminal vesicle invasion after radical prostatectomy. Cancer. 2006; 106:2369–75.
Article8. Epstein JI, Partin AW, Potter SR, Walsh PC. Adenocarcinoma of the prostate invading the seminal vesicle: prognostic stratification based on pathologic parameters. Urology. 2000; 56:283–8.
Article9. Mottet N, van den Bergh RC, Briers E, Van den Broeck T, Cumberbatch MG, De Santis M, et al. EAU-EANM-ESTRO-ESUR-SIOG guidelines on prostate cancer-2020 update. Part 1: screening, diagnosis, and local treatment with curative intent. Eur Urol. 2021; 79:243–62.10. Tilki D, Chen MH, Wu J, Huland H, Graefen M, Wiegel T, et al. Adjuvant versus early salvage radiation therapy for men at high risk for recurrence following radical prostatectomy for prostate cancer and the risk of death. J Clin Oncol. 2021; 39:2284–93.
Article11. Parker C, Castro E, Fizazi K, Heidenreich A, Ost P, Procopio G, et al. Prostate cancer: ESMO clinical practice guidelines for diagnosis, treatment and follow-up. Ann Oncol. 2020; 31:1119–34.
Article12. Lee HJ, Han JH, Lee DH, Nam JK, Kim TN, Chung MK, et al. Does bilateral seminal vesicle invasion at radical prostatectomy predict worse prognosis than unilateral invasion among patients with pT3b prostate cancers? Int J Urol. 2016; 23:758–63.
Article13. Kristiansen A, Wiklund F, Wiklund P, Egevad L. Prognostic significance of patterns of seminal vesicle invasion in prostate cancer. Histopathology. 2013; 62:1049–56.
Article14. Vidal Crespo N, Enguita Arnal L, Gomez-Ferrer A, Collado Serra A, Mascaros JM, Calatrava Fons A, et al. Bilateral seminal vesicle invasion is not associated with worse outcomes in locally advanced prostate carcinoma. Medicina (Kaunas). 2022; 58:1057.
Article15. Numbere N, Teramoto Y, Gurung PM, Wang Y, Yang Z, Miyamoto H. The clinical impact of unilateral versus bilateral invasion into the seminal vesicle in patients with prostate cancer undergoing radical prostatectomy. Arch Pathol Lab Med. 2022; 146:855–61.
Article16. Epstein JI, Zelefsky MJ, Sjoberg DD, Nelson JB, Egevad L, Magi-Galluzzi C, et al. A contemporary prostate cancer grading system: a validated alternative to the Gleason score. Eur Urol. 2016; 69:428–35.
Article17. Buyyounouski MK, Choyke PL, McKenney JK, Sartor O, Sandler HM, Amin MB, et al. Prostate cancer: major changes in the American Joint Committee on Cancer eighth edition cancer staging manual. CA Cancer J Clin. 2017; 67:245–53.18. Cookson MS, Aus G, Burnett AL, Canby-Hagino ED, D’Amico AV, Dmochowski RR, et al. Variation in the definition of biochemical recurrence in patients treated for localized prostate cancer: the American Urological Association Prostate Guidelines for Localized Prostate Cancer Update Panel report and recommendations for a standard in the reporting of surgical outcomes. J Urol. 2007; 177:540–5.
Article19. Boorjian SA, Thompson RH, Tollefson MK, Rangel LJ, Bergstralh EJ, Blute ML, et al. Long-term risk of clinical progression after biochemical recurrence following radical prostatectomy: the impact of time from surgery to recurrence. Eur Urol. 2011; 59:893–9.
Article20. Jain B, Ng K, Santos PM, Taparra K, Muralidhar V, Mahal BA, et al. Prostate cancer disparities in risk group at presentation and access to treatment for Asian Americans, native Hawaiians, and Pacific islanders: a study with disaggregated ethnic groups. JCO Oncol Pract. 2022; 18:e204–18.21. Zhu Y, Mo M, Wei Y, Wu J, Pan J, Freedland SJ, et al. Epidemiology and genomics of prostate cancer in Asian men. Nat Rev Urol. 2021; 18:282–301.
Article22. Sachdeva A, Veeratterapillay R, Voysey A, Kelly K, Johnson MI, Aning J, et al. Positive surgical margins and biochemical recurrence following minimally-invasive radical prostatectomy: an analysis of outcomes from a UK tertiary referral centre. BMC Urol. 2017; 17:91.23. Pagano MJ, Whalen MJ, Paulucci DJ, Reddy BN, Matulay JT, Rothberg M, et al. Predictors of biochemical recurrence in pT3b prostate cancer after radical prostatectomy without adjuvant radiotherapy. Prostate. 2016; 76:226–34.
Article24. Maxeiner A, Magheli A, Johrens K, Kilic E, Braun TL, Kempkensteffen C, et al. Significant reduction in positive surgical margin rate after laparoscopic radical prostatectomy by application of the modified surgical margin recommendations of the 2009 International Society of Urological Pathology consensus. BJU Int. 2016; 118:750–7.
Article25. Fleshner NE, Evans A, Chadwick K, Lawrentschuk N, Zlotta A. Clinical significance of the positive surgical margin based upon location, grade, and stage. Urol Oncol. 2010; 28:197–204.
Article26. Zhang L, Wu B, Zha Z, Zhao H, Yuan J, Jiang Y, et al. Surgical margin status and its impact on prostate cancer prognosis after radical prostatectomy: a meta-analysis. World J Urol. 2018; 36:1803–15.
Article27. Retel VP, Bouchardy C, Usel M, Neyroud-Caspar I, Schmidlin F, Wirth G, et al. Determinants and effects of positive surgical margins after prostatectomy on prostate cancer mortality: a population-based study. BMC Urol. 2014; 14:86.
Article28. Jemal A, Fedewa SA, Ma J, Siegel R, Lin CC, Brawley O, et al. Prostate cancer incidence and PSA testing patterns in relation to USPSTF screening recommendations. JAMA. 2015; 314:2054–61.
Article29. Egevad L, Srigley JR, Delahunt B. International Society of Urological Pathology (ISUP) consensus conference on handling and staging of radical prostatectomy specimens: rationale and organization. Mod Pathol. 2011; 24:1–5.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Predictors of Biochemical Failure after Radical Perineal Prostatectomy for Localized Prostate Cancer
- The Pathological Characteristics of Localized Prostate Cancer, Managed with Radical Prostatectomy
- Prostate Volume has Prognostic Value Only in Pathologic T2 Radical Prostatectomy Specimens
- Clinicopathological Significance of the Lymphovascular Invasion Detected in Specimens from Radical Retropubic Prostatectomies
- The Role of Endorectal Magnetic Resonance Imaging in Predicting Extraprostatic Extension and Seminal Vesicle Invasion in Clinically Localized Prostate Cancer