Cancer Res Treat.
2024 Jul;56(3):809-824. 10.4143/crt.2023.920.
The Clinical Efficacy of Colorectal Cancer Patients with Pulmonary Oligometastases by Sterotactic Body Ablative Radiotherapy: A Meta-Analysis
- Affiliations
-
- 1Department of Radiation Oncology, Chonnam National University Hwasun Hospital, Chonnam National University College of Medicine, Hwasun, Korea
- 2Department of Radiation Oncology, Korea University Ansan Hospital, Korea University College of Medicine, Ansan, Korea
- 3Department of Radiation Oncology, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea
- 4Department of Radiation Oncology, Seoul National University College of Medicine, Seoul, Korea
- 5Department of Radiation Oncology, St. Vincent’s Hospital, College of Medicine, The Catholic University of Korea, Suwon, Korea
- KMID: 2557668
- DOI: http://doi.org/10.4143/crt.2023.920
Abstract
- Purpose
There is increasing interest in the efficacy of stereotactic ablative radiotherapy (SABR) for treating colorectal cancer (CRC) patients with oligometastases (OM), recently. The purpose of this meta-analysis was to evaluate local control (LC), progression-free survival (PFS), and overall survival (OS) of CRC patients with pulmonary OM treated with SABR and toxicities.
Materials and Methods
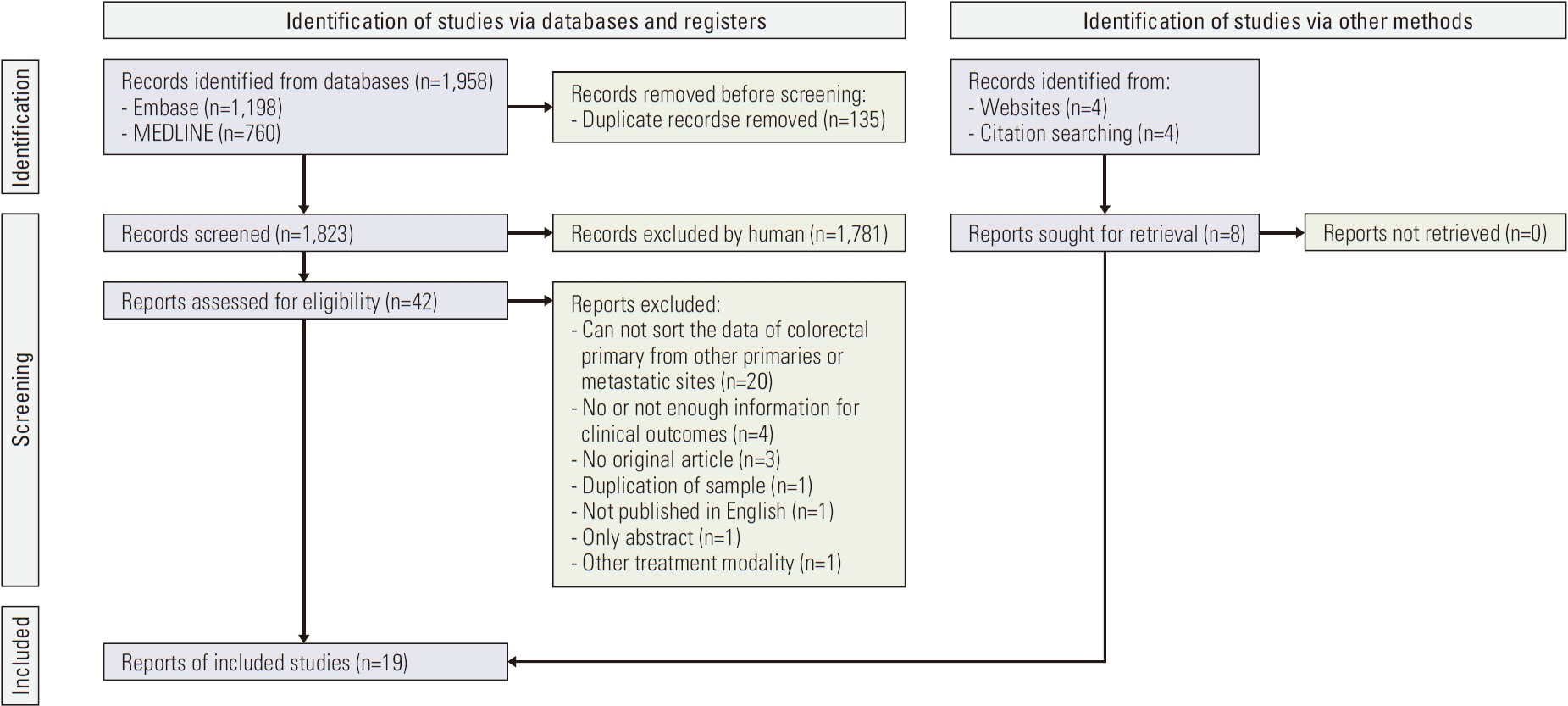
Studies that reported SABR for CRC patients with pulmonary OM were searched from MEDLINE and Embase. Treatment outcomes including LC, PFS, OS, and toxicities of grade 3 or higher were assessed.
Results
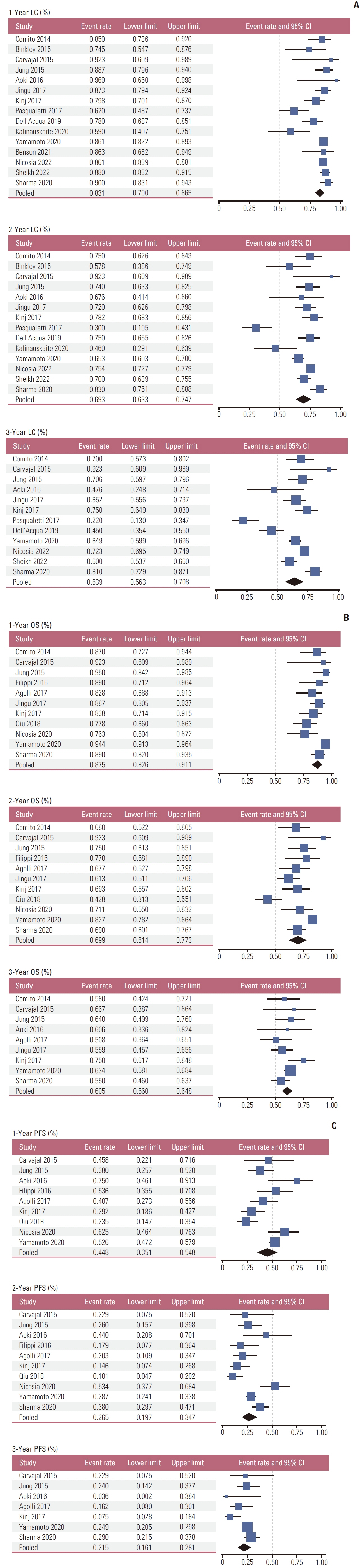
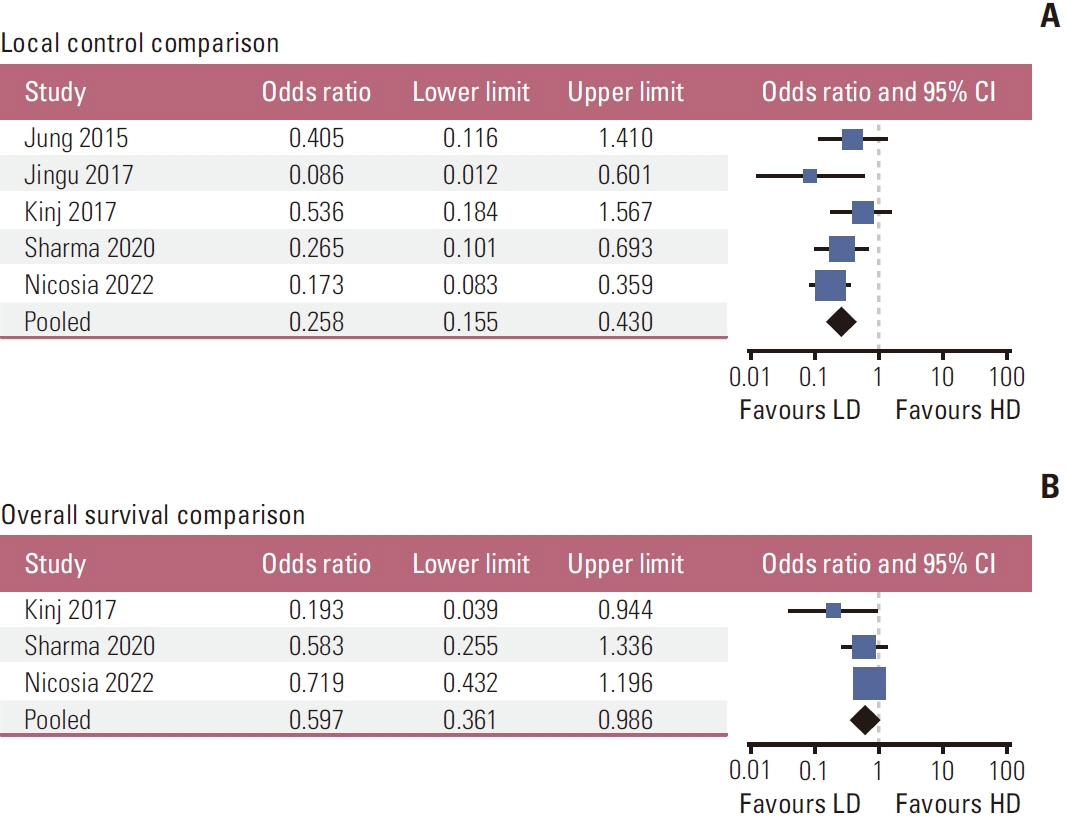
A total of 19 studies with 1,668 patients were chosen for this meta-analysis. Pooled 1-, 2-, and 3-year LC rates were 83.1%, 69.3%, and 63.9%, respectively. PFS rates were 44.8%, 26.5%, and 21.5% at 1, 2, and 3 years, respectively. OS rates at 1-, 2-, and 3-year were 87.5%, 69.9%, and 60.5%, respectively. The toxicity rate of grade 3 or higher was 3.6%. The effect of dose escalation was meta-analyzed using available studies.
Conclusion
Application of SABR to CRC patients with pulmonary OM achieved modest local control with acceptable toxicity according to the present meta-analysis. Further studies establishing the clinical efficacy of SABR are guaranteed.
Keyword
Figure
Cited by 1 articles
-
Identifying Trends in Oncology Research through a Bibliographic Analysis of
Cancer Research and Treatment
Choong-kun Lee, Jeong Min Choo, Yong Chan Ahn, Jin Kim, Sun Young Rha, Chai Hong Rim
Cancer Res Treat. 2025;57(1):11-18. doi: 10.4143/crt.2024.688.
Reference
-
References
1. Hellman S, Weichselbaum RR. Oligometastases. J Clin Oncol. 1995; 13:8–10.
Article2. Hughes KS, Rosenstein RB, Songhorabodi S, Adson MA, Ilstrup DM, Fortner JG, et al. Resection of the liver for colorectal carcinoma metastases: a multi-institutional study of longterm survivors. Dis Colon Rectum. 1988; 31:1–4.3. Nordlinger B, Guiguet M, Vaillant JC, Balladur P, Boudjema K, Bachellier P, et al. Surgical resection of colorectal carcinoma metastases to the liver: a prognostic scoring system to improve case selection, based on 1568 patients. Association Francaise de Chirurgie. Cancer. 1996; 77:1254–62.
Article4. Weichselbaum RR, Hellman S. Oligometastases revisited. Nat Rev Clin Oncol. 2011; 8:378–82.
Article5. Gomez DR, Tang C, Zhang J, Blumenschein GR Jr, Hernandez M, Lee JJ, et al. Local consolidative therapy vs. maintenance therapy or observation for patients with oligometastatic non-small-cell lung cancer: long-term results of a multi-institutional, phase II, randomized study. J Clin Oncol. 2019; 37:1558–65.
Article6. Iyengar P, Wardak Z, Gerber DE, Tumati V, Ahn C, Hughes RS, et al. Consolidative radiotherapy for limited metastatic non-small-cell lung cancer: a phase 2 randomized clinical trial. JAMA Oncol. 2018; 4:e173501.7. Parker CC, James ND, Brawley CD, Clarke NW, Hoyle AP, Ali A, et al. Radiotherapy to the primary tumour for newly diagnosed, metastatic prostate cancer (STAMPEDE): a randomised controlled phase 3 trial. Lancet. 2018; 392:2353–66.8. Biasco G, Derenzini E, Grazi G, Ercolani G, Ravaioli M, Pantaleo MA, et al. Treatment of hepatic metastases from colorectal cancer: many doubts, some certainties. Cancer Treat Rev. 2006; 32:214–28.
Article9. Van Cutsem E, Nordlinger B, Adam R, Kohne CH, Pozzo C, Poston G, et al. Towards a pan-European consensus on the treatment of patients with colorectal liver metastases. Eur J Cancer. 2006; 42:2212–21.
Article10. Grossmann I, Avenarius JK, Mastboom WJ, Klaase JM. Preoperative staging with chest CT in patients with colorectal carcinoma: not as a routine procedure. Ann Surg Oncol. 2010; 17:2045–50.
Article11. Qiu M, Hu J, Yang D, Cosgrove DP, Xu R. Pattern of distant metastases in colorectal cancer: a SEER based study. Oncotarget. 2015; 6:38658–66.
Article12. Vatandoust S, Price TJ, Karapetis CS. Colorectal cancer: metastases to a single organ. World J Gastroenterol. 2015; 21:11767–76.
Article13. Ruers T, Punt C, Van Coevorden F, Pierie J, Borel-Rinkes I, Ledermann JA, et al. Radiofrequency ablation combined with systemic treatment versus systemic treatment alone in patients with non-resectable colorectal liver metastases: a randomized EORTC Intergroup phase II study (EORTC 40004). Ann Oncol. 2012; 23:2619–26.14. Treasure T, Farewell V, Macbeth F, Monson K, Williams NR, Brew-Graves C, et al. Pulmonary Metastasectomy versus Continued Active Monitoring in Colorectal Cancer (PulMiCC): a multicentre randomised clinical trial. Trials. 2019; 20:718.
Article15. Lee BM, Chang JS, Koom WS, Byun HK, Kim HS, Beom SH, et al. Importance of local ablative therapies for lung metastases in patients with colorectal cancer. Ann Surg. 2023; 278:e173.
Article16. Willmann J, Adilovic S, Vlaskou Badra E, Christ SM, Ahmadsei M, Tanadini-Lang S, et al. Repeat stereotactic body radiotherapy for oligometastatic disease. Radiother Oncol. 2023; 184:109671.
Article17. Onaitis MW, Petersen RP, Haney JC, Saltz L, Park B, Flores R, et al. Prognostic factors for recurrence after pulmonary resection of colorectal cancer metastases. Ann Thorac Surg. 2009; 87:1684–8.
Article18. Lee WS, Yun SH, Chun HK, Lee WY, Yun HR, Kim J, et al. Pulmonary resection for metastases from colorectal cancer: prognostic factors and survival. Int J Colorectal Dis. 2007; 22:699–704.
Article19. Okunieff P, Petersen AL, Philip A, Milano MT, Katz AW, Boros L, et al. Stereotactic body radiation therapy (SBRT) for lung metastases. Acta Oncol. 2006; 45:808–17.
Article20. Rusthoven KE, Kavanagh BD, Cardenes H, Stieber VW, Burri SH, Feigenberg SJ, et al. Multi-institutional phase I/II trial of stereotactic body radiation therapy for liver metastases. J Clin Oncol. 2009; 27:1572–8.
Article21. NCCN Clinical Practice Guidelines in Oncology. Colon cancer version 4.2023 [Internet]. Plymouth Meeing, PA: National Comprehensive Cancer Network; c2023 [cited 2023 Nov 15]. Available from: https://www.nccn.org/guidelines/guidelines-detail?category=1&id=1428.22. Moher D, Liberati A, Tetzlaff J, Altman DG, Group P. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Ann Intern Med. 2009; 151:264–9.
Article23. Stang A. Critical evaluation of the Newcastle-Ottawa scale for the assessment of the quality of nonrandomized studies in meta-analyses. Eur J Epidemiol. 2010; 25:603–5.
Article24. Cochran WG. The combination of estimates from different experiments. Biometrics. 1954; 10:101–29.
Article25. Higgins JP, Thompson SG. Quantifying heterogeneity in a meta-analysis. Stat Med. 2002; 21:1539–58.
Article26. Egger M, Davey Smith G, Schneider M, Minder C. Bias in meta-analysis detected by a simple, graphical test. BMJ. 1997; 315:629–34.
Article27. Duval S, Tweedie R. Trim and fill: a simple funnel-plot-based method of testing and adjusting for publication bias in metaanalysis. Biometrics. 2000; 56:455–63.
Article28. Comito T, Cozzi L, Clerici E, Campisi MC, Liardo RL, Navarria P, et al. Stereotactic ablative radiotherapy (SABR) in inoperable oligometastatic disease from colorectal cancer: a safe and effective approach. BMC Cancer. 2014; 14:619.
Article29. Binkley MS, Trakul N, Jacobs LR, von Eyben R, Le QT, Maxim PG, et al. Colorectal histology is associated with an increased risk of local failure in lung metastases treated with stereotactic ablative radiation therapy. Int J Radiat Oncol Biol Phys. 2015; 92:1044–52.30. Carvajal C, Navarro-Martin A, Cacicedo J, Ramos R, Guedea F. Stereotactic body radiotherapy for colorectal lung oligometastases: preliminary single-institution results. J BUON. 2015; 20:158–65.31. Jung J, Song SY, Kim JH, Yu CS, Kim JC, Kim TW, et al. Clinical efficacy of stereotactic ablative radiotherapy for lung metastases arising from colorectal cancer. Radiat Oncol. 2015; 10:238.
Article32. Aoki M, Hatayama Y, Kawaguchi H, Hirose K, Sato M, Akimoto H, et al. Stereotactic body radiotherapy for lung metastases as oligo-recurrence: a single institutional study. J Radiat Res. 2016; 57:55–61.
Article33. Filippi AR, Guerrera F, Badellino S, Ceccarelli M, Castiglione A, Guarneri A, et al. Exploratory analysis on overall survival after either surgery or stereotactic radiotherapy for lung oligometastases from colorectal cancer. Clin Oncol (R Coll Radiol). 2016; 28:505–12.
Article34. Agolli L, Bracci S, Nicosia L, Valeriani M, De Sanctis V, Osti MF. Lung metastases treated with stereotactic ablative radiation therapy in oligometastatic colorectal cancer patients: outcomes and prognostic factors after long-term follow-up. Clin Colorectal Cancer. 2017; 16:58–64.
Article35. Jingu K, Matsuo Y, Onishi H, Yamamoto T, Aoki M, Murakami Y, et al. Dose escalation improves outcome in stereotactic body radiotherapy for pulmonary oligometastases from colorectal cancer. Anticancer Res. 2017; 37:2709–13.
Article36. Kinj R, Bondiau PY, Francois E, Gerard JP, Naghavi AO, Leysalle A, et al. Radiosensitivity of colon and rectal lung oligometastasis treated with stereotactic ablative radiotherapy. Clin Colorectal Cancer. 2017; 16:e211.
Article37. Pasqualetti F, Montrone S, Vivaldi C, Zani M, Fedele D, Fornaro L, et al. Stereotactic body radiotherapy in patients with lung oligometastases from colorectal cancer. Anticancer Res. 2017; 37:315–9.
Article38. Qiu H, Katz AW, Chowdhry AK, Usuki KY, Singh DP, Metcalfe S, et al. Stereotactic body radiotherapy for lung metastases from colorectal cancer: prognostic factors for disease control and survival. Am J Clin Oncol. 2018; 41:53–8.39. Dell’Acqua V, Surgo A, Kraja F, Kobiela J, Zerella MA, Spychalski P, et al. Stereotactic radiation therapy in oligometastatic colorectal cancer: outcome of 102 patients and 150 lesions. Clin Exp Metastasis. 2019; 36:331–42.
Article40. Kalinauskaite GG, Tinhofer II, Kufeld MM, Kluge AA, Grun AA, Budach VV, et al. Radiosurgery and fractionated stereotactic body radiotherapy for patients with lung oligometastases. BMC Cancer. 2020; 20:404.
Article41. Nicosia L, Cuccia F, Mazzola R, Ricchetti F, Figlia V, Giaj-Levra N, et al. Disease course of lung oligometastatic colorectal cancer treated with stereotactic body radiotherapy. Strahlenther Onkol. 2020; 196:813–20.
Article42. Sharma A, Baker S, Duijm M, Oomen-de Hoop E, Cornelissen R, Verhoef C, et al. Prognostic factors for local control and survival for inoperable pulmonary colorectal oligometastases treated with stereotactic body radiotherapy. Radiother Oncol. 2020; 144:23–9.
Article43. Yamamoto T, Niibe Y, Matsumoto Y, Onishi H, Aoki M, Nishikawa A, et al. Analyses of local control and survival after stereotactic body radiotherapy for pulmonary oligometastases from colorectal adenocarcinoma. J Radiat Res. 2020; 61:935–44.
Article44. Benson KRK, Sandhu N, Zhang C, Ko R, Toesca DA, Lee PE, et al. Local recurrence outcomes of colorectal cancer oligometastases treated with stereotactic ablative radiotherapy. Am J Clin Oncol. 2021; 44:559–64.45. Nicosia L, Franceschini D, Perrone-Congedi F, Casamassima F, Gerardi MA, Rigo M, et al. A multicenter LArge retrospectIve daTabase on the personalization of stereotactic ABlative radiotherapy use in lung metastases from colon-rectal cancer: The LaIT-SABR study. Radiother Oncol. 2022; 166:92–9.
Article46. Sheikh S, Chen H, Sahgal A, Poon I, Erler D, Badellino S, et al. An analysis of a large multi-institutional database reveals important associations between treatment parameters and clinical outcomes for stereotactic body radiotherapy (SBRT) of oligometastatic colorectal cancer. Radiother Oncol. 2022; 167:187–94.
Article47. Siebenhuner AR, Guller U, Warschkow R. Population-based SEER analysis of survival in colorectal cancer patients with or without resection of lung and liver metastases. BMC Cancer. 2020; 20:246.
Article48. Yu WS, Bae MK, Choi JK, Hong YK, Park IK. Pulmonary metastasectomy in colorectal cancer: a population-based retrospective cohort study using the Korean National Health Insurance Database. Cancer Res Treat. 2021; 53:1104–12.
Article49. Kuo HT, Que J, Lin LC, Yang CC, Koay LB, Lin CH. Impact of tumor size on outcome after stereotactic body radiation therapy for inoperable hepatocellular carcinoma. Medicine (Baltimore). 2017; 96:e9249.
Article50. Owen D, Siva S, Salama JK, Daly M, Kruser TJ, Giuliani M. Some like it hot: the value of dose and hot spots in lung stereotactic body radiation therapy. Int J Radiat Oncol Biol Phys. 2023; 117:1–5.
Article51. Klement RJ. Radiobiological parameters of liver and lung metastases derived from tumor control data of 3719 metastases. Radiother Oncol. 2017; 123:218–26.
Article52. Van den Begin R, Engels B, Collen C, de Vin T, Defauw A, Dubaere E, et al. The METABANK score: a clinical tool to predict survival after stereotactic radiotherapy for oligometastatic disease. Radiother Oncol. 2019; 133:113–9.
Article53. Willmann J, Vlaskou Badra E, Adilovic S, Ahmadsei M, Christ SM, van Timmeren JE, et al. Evaluation of the prognostic value of the ESTRO EORTC classification of oligometastatic disease in patients treated with stereotactic body radiotherapy: a retrospective single center study. Radiother Oncol. 2022; 168:256–64.
Article54. Franzese C, Comito T, Franceschini D, Loi M, Clerici E, Navarria P, et al. Recursive partitioning model-based analysis for survival of colorectal cancer patients with lung and liver oligometastases treated with stereotactic body radiation therapy. J Cancer Res Clin Oncol. 2020; 146:1227–34.
Article55. Klement RJ, Guckenberger M, Alheid H, Allgauer M, Becker G, Blanck O, et al. Stereotactic body radiotherapy for oligometastatic liver disease: influence of pre-treatment chemotherapy and histology on local tumor control. Radiother Oncol. 2017; 123:227–33.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Tumor Control and Overall Survival after Stereotactic Body Radiotherapy for Pulmonary Oligometastases from Colorectal Cancer: A Meta-Analysis
- Bone-only oligometastatic prostate cancer: can SABR improve outcomes? A single-center experience
- Long-term survival after multimodal treatment involving radiotherapy for huge hepatocellular carcinoma with oligometastasis: a case report
- Local ablative radiotherapy for oligometastatic non-small cell lung cancer
- Stereotactic Body Radiotherapy for Early Stage Lung Cancer