J Korean Neurosurg Soc.
2024 Jul;67(4):451-457. 10.3340/jkns.2023.0176.
Protein Requirement Changes According to the Treatment Application in Neurocritical Patients
- Affiliations
-
- 1Department of Traumatology, Gachon University Gil Medical Center, Incheon, Korea
- 2Department of Critical Care Medicine, Kangbuk Samsung Hospital, Sungkyunkwan University School of Medicine, Seoul, Korea
- 3Department of Neurosurgery, Seoul St. Mary’s Hospital, College of Medicine, The Catholic University of Korea, Seoul, Korea
- 4Department of Neurosurgery, Incheon St. Mary’s Hospital, College of Medicine, The Catholic University of Korea, Incheon, Korea
- 5SMG-SNU Boramae Medical Center, Seoul, Korea
- 6Department of Critical Care Medicine, Seoul National University Hospital, Seoul, Korea
- 7Department of Neurosurgery, Seoul National University Hospital, Seoul, Korea
- KMID: 2556742
- DOI: http://doi.org/10.3340/jkns.2023.0176
Abstract
Objective
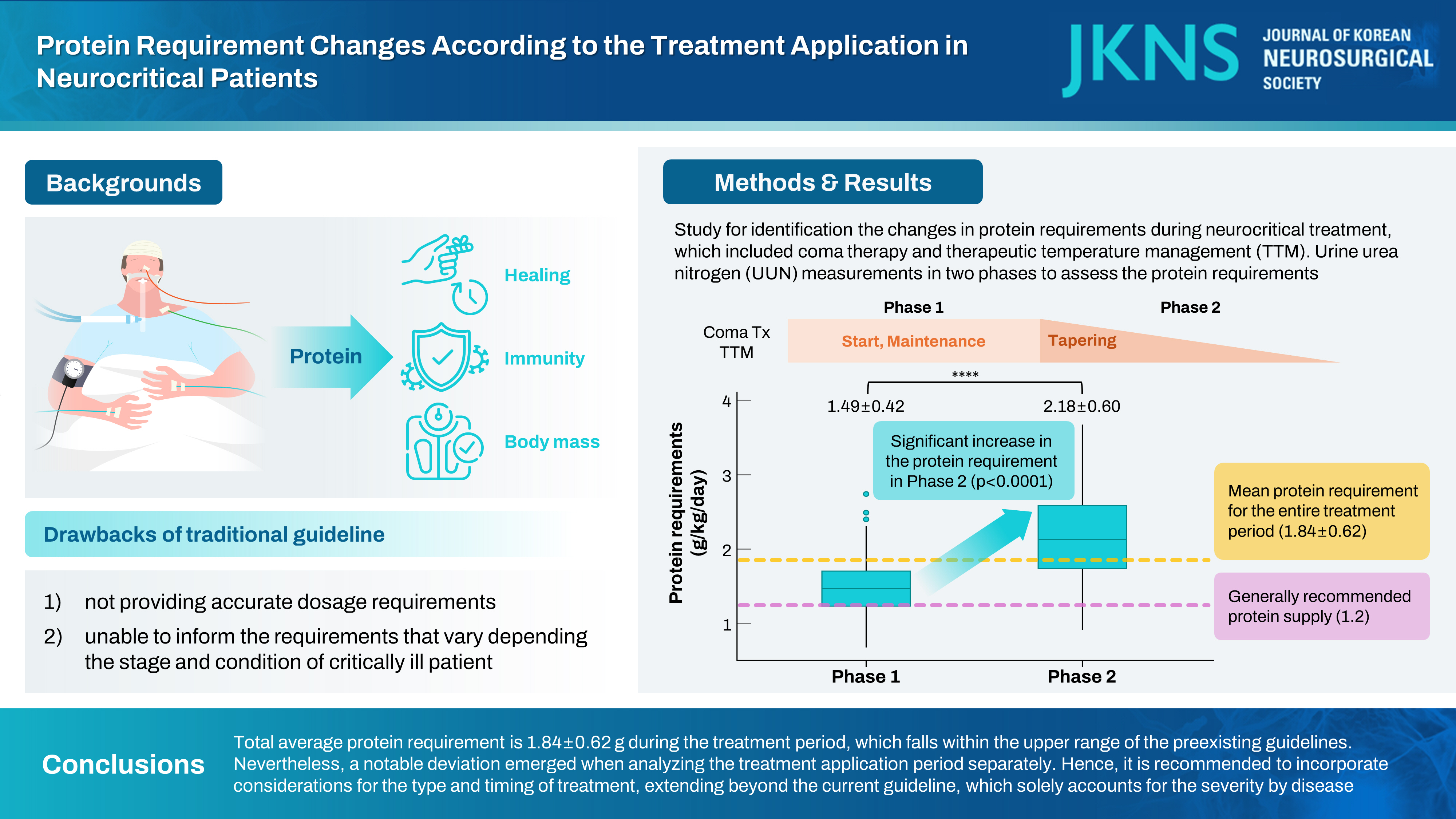
: Exploring protein requirements for critically ill patients has become prominent. On the other hand, considering the significant impact of coma therapy and targeted temperature management (TTM) on the brain as well as systemic metabolisms, protein requirements may plausibly be changed by treatment application. However, there is currently no research on protein requirements following the application of these treatments. Therefore, the aim of this study is to elucidate changes in patients’ protein requirements during the application of TTM and coma therapy.
Methods
: This study is a retrospective analysis of prospectively collected data from March 2019 to May 2022. Among the patients admitted to the intensive care unit, those receiving coma therapy and TTM were included. The patient’s treatment period was divided into two phases (phase 1, application and maintenance of coma therapy and TTM; phase 2, tapering and cessation of treatment). In assessing protein requirements, the urine urea nitrogen (UUN) method was employed to estimate the nitrogen balance, offering insight into protein utilization within the body. The patient’s protein requirement for each phase was defined as the amount of protein required to achieve a nitrogen balance within ±5, based on the 24-hour collection of UUN. Changes in protein requirements between phases were analyzed.
Results
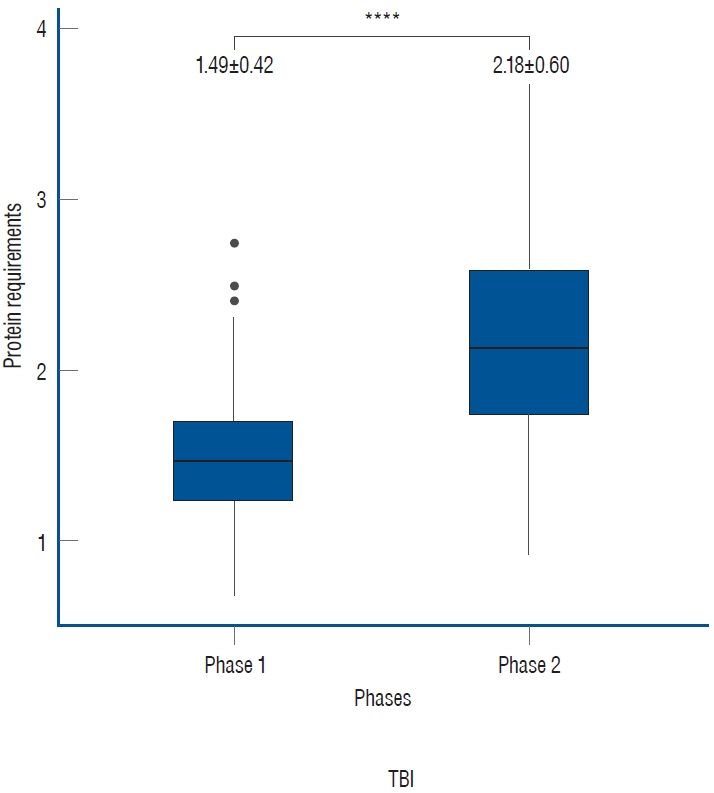
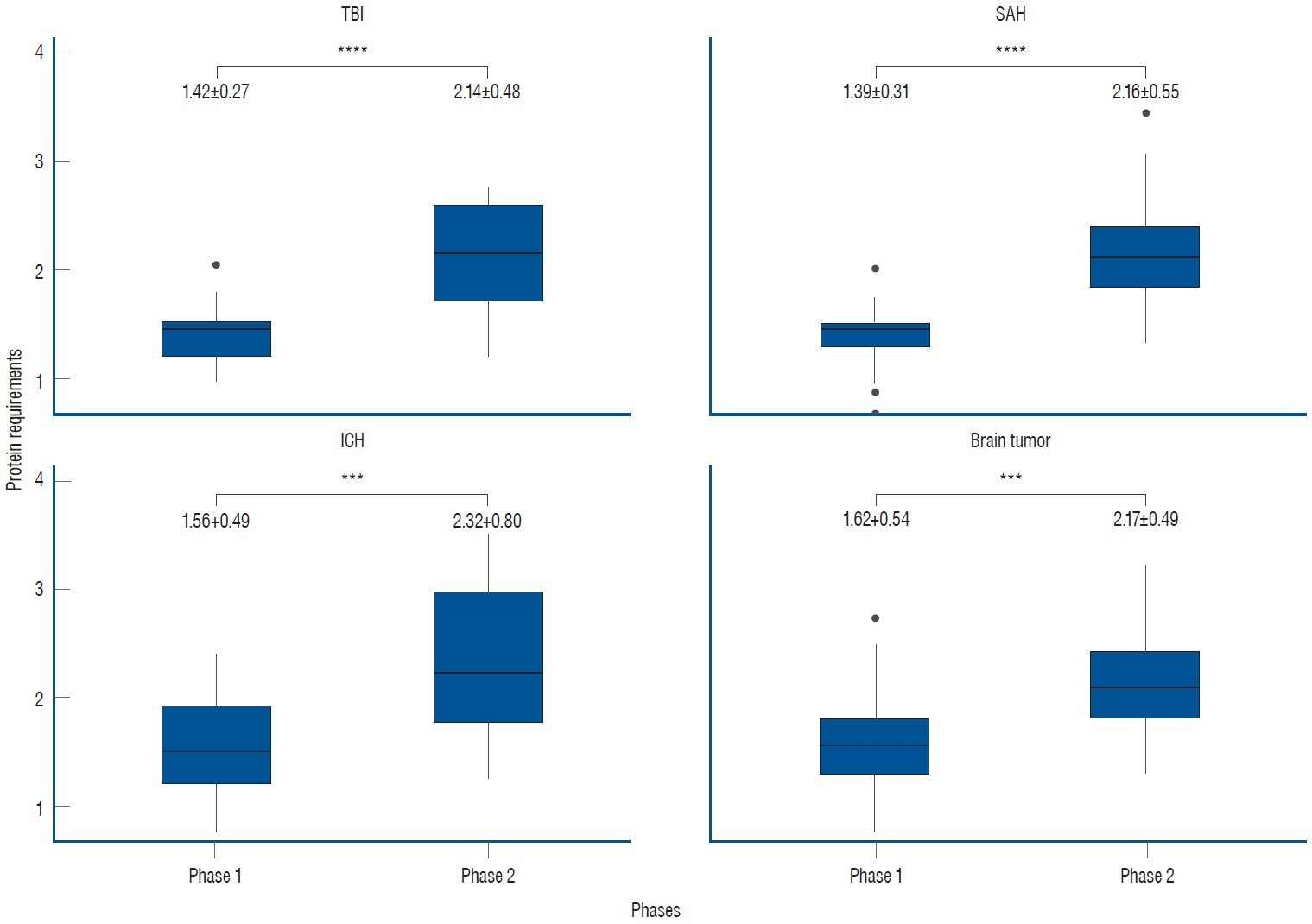
: Out of 195 patients, 107 patients with a total of 214 UUN values were included. The mean protein requirement for the entire treatment period was 1.84±0.62 g/kg/day, which is higher than the generally recommended protein supply of 1.2 g/kg/day. As the treatment was tapered, there was a statistically significant increase in the protein requirement from 1.49±0.42 to 2.18±0.60 in phase 2 (p<0.001).
Conclusion
: Our study revealed a total average protein requirement of 1.84±0.62 g during the treatment period, which falls within the upper range of the preexisting guidelines. Nevertheless, a notable deviation emerged when analyzing the treatment application period separately. Hence, it is recommended to incorporate considerations for the type and timing of treatment, extending beyond the current guideline, which solely accounts for the severity by disease.
Keyword
Figure
Cited by 1 articles
-
Editors’ Pick in July 2024
Hee-Jin Yang
J Korean Neurosurg Soc. 2024;67(4):383-384. doi: 10.3340/jkns.2024.0119.
Reference
-
References
1. Ashcraft CM, Frankenfield DC. Energy expenditure during barbiturate coma. Nutr Clin Pract. 28:603–608. 2013.
Article2. Badjatia N, Monahan A, Carpenter A, Zimmerman J, Schmidt JM, Claassen J, et al. Inflammation, negative nitrogen balance, and outcome after aneurysmal subarachnoid hemorrhage. Neurology. 84:680–687. 2015.
Article3. Bidkar PU. Nutrition in neuro-intensive care and outcomes. J Neuroanaesth Crit Care. 3:S70–S76. 2016.
Article4. Bingham SA. Urine nitrogen as a biomarker for the validation of dietary protein intake. J Nutr 133 Suppl. 3:921S–924S. 2003.
Article5. Bourke CD, Berkley JA, Prendergast AJ. Immune dysfunction as a cause and consequence of malnutrition. Trends Immunol. 37:386–398. 2016.
Article6. Buckley CT, Dickerson RN. Propofol: a risk factor for caloric overfeeding and inadequate protein delivery. Hosp Pharm. 55:151–152. 2020.
Article7. Chapple LA, Chapman MJ, Lange K, Deane AM, Heyland DK. Nutrition support practices in critically ill head-injured patients: a global perspective. Crit Care. 20:6. 2016.
Article8. Compher C, Bingham AL, McCall M, Patel J, Rice TW, Braunschweig C, et al. Guidelines for the provision of nutrition support therapy in the adult critically ill patient: the American Society for Parenteral and Enteral Nutrition. JPEN J Parenter Enteral Nutr. 46:12–41. 2022.
Article9. Dickerson RN, Roth-Yousey L. Medication effects on metabolic rate: a systematic review (part 1). J Am Diet Assoc. 105:835–843. 2005.
Article10. Erecinska M, Thoresen M, Silver IA. Effects of hypothermia on energy metabolism in Mammalian central nervous system. J Cereb Blood Flow Metab. 23:513–530. 2003.
Article11. Fan E, Ciesla ND, Truong AD, Bhoopathi V, Zeger SL, Needham DM. Inter-rater reliability of manual muscle strength testing in ICU survivors and simulated patients. Intensive Care Med. 36:1038–1043. 2010.
Article12. Fisher N, Uhler ME : Basic Neurochemistry: Molecular, Cellular, and Medical Aspects. Philadelphia : Lippincott Williams & Wilkins, 1999.13. Fuhrman FA. The effect of body temperature on the duration of barbiturate anesthesia in mice. Science. 105:387–388. 1947.
Article14. Heyland DK, Mourtzakis M : Malnutrition in Critical Illness: Implications, Causes, and Therapeutic Approaches in Stevens RD, Hart N, Herridge MS (eds) : Textbook of Post-ICU Medicine: The Legacy of Critical Care. Oxford : Oxford University Press, 2014, pp.401-416.15. Heyland DK, Weijs PJ, Coss‐Bu JA, Taylor B, Kristof AS, O’Keefe GE, et al. Protein delivery in the intensive care unit: optimal or suboptimal? Nutr Clin Pract. 32:58S–71S. 2017.
Article16. Ingadottir AR, Beck AM, Baldwin C, Weekes CE, Geirsdottir OG, Ramel A, et al. Association of energy and protein intakes with length of stay, readmission and mortality in hospitalised patients with chronic obstructive pulmonary disease. Br J Nutr. 119:543–551. 2018.
Article17. Lee HY, Oh BM. Nutrition management in patients with traumatic brain injury: a narrative review. Brain Neurorehabil. 15:e4. 2022.
Article18. McCall M, Jeejeebhoy K, Pencharz P, Moulton R. Effect of neuromuscular blockade on energy expenditure in patients with severe head injury. JPEN J Parenter Enteral Nutr. 27:27–35. 2003.
Article19. McClave SA, Taylor BE, Martindale RG, Warren MM, Johnson DR, Braunschweig C, et al. Guidelines for the provision and assessment of nutrition support therapy in the adult critically ill patient: Society of Critical Care Medicine (SCCM) and American Society for Parenteral and Enteral Nutrition (A.S.P.E.N.). JPEN J Parenter Enteral Nutr. 40:159–211. 2016.
Article20. Mogensen KM, Robinson MK, Casey JD, Gunasekera NS, Moromizato T, Rawn JD, et al. Nutritional status and mortality in the critically ill. Crit Care Med. 43:2605–2615. 2015.
Article21. Moritz F, Petit J, Kaeffer N, Oksenhendler G, Papion H, Hecketsweiler B, et al. Metabolic effects of propofol and flunitrazepam given for sedation after aortic surgery. Br J Anaesth. 70:451–453. 1993.
Article22. Polderman KH. Mechanisms of action, physiological effects, and complications of hypothermia. Crit Care Med. 37(7 Suppl):S186–S202. 2009.
Article23. Sato J, Inaba H, Hirasawa H, Mizuguchi T. Metabolic changes associated with malnutrition in the patients with multiple organ failure. J Anesth. 7:276–286. 1993.
Article24. Sieber CC. Malnutrition and sarcopenia. Aging Clin Exp Res. 31:793–798. 2019.
Article25. Singer P, Blaser AR, Berger MM, Alhazzani W, Calder PC, Casaer MP, et al. ESPEN guideline on clinical nutrition in the intensive care unit. Clin Nutr. 38:48–79. 2019.
Article26. Stechmiller JK. Understanding the role of nutrition and wound healing. Nutr Clin Pract. 25:61–68. 2010.
Article27. Tripathy S. Nutrition in the neurocritical care unit. J Neuroanaesth Crit Care. 2:88–96. 2015.
Article28. Villet S, Chiolero RL, Bollmann MD, Revelly JP, Cayeux R N MC, Delarue J, et al. Negative impact of hypocaloric feeding and energy balance on clinical outcome in ICU patients. Clin Nutr. 24:502–509. 2005.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Hiccups in neurocritical care
- Basic considerations on magnesium in the management of neurocritical patients
- Surgical Treatment in Neurocritical Care for Acute Spinal Cord Injuries
- Neurotrauma Code: Proposal for the Implementation of Strategies in Areas of Difficult Care for a Time-dependent Condition.
- Therapeutic Momentum: Scenarios in Patients with Neurotrauma