J Neurocrit Care.
2021 Dec;14(2):78-87. 10.18700/jnc.210018.
Basic considerations on magnesium in the management of neurocritical patients
- Affiliations
-
- 1Medical and Surgical Research Center, Cartagena, Colombia
- 2Colombian Clinical Research Group in Neurocritical Care, School of Medicine, University of Cartagena, Cartagena, Colombia
- 3Latin American Council of Neurocritical Care, Cartagena, Colombia
- 4School of Medicine, Universidad del Magdalena, Santa Marta, Colombia
- 5School of Medicine, Universidad de la Sabana, Chía, Colombia
- 6School of Medicine, Fundación Universitaria Juan N Corpas, Bogotá, Colombia
- 7Colombian Clinical Research Group in Neurocritical Care, School of Medicine, Fundación Universitaria Autonoma de las Americas, Pereira, Colombia
- 8School of Medicine, Universidad de Manizales, Manizales, Colombia
- 9Department of Intensive Care, Regions Hospital, St Paul, MN, USA
- KMID: 2523717
- DOI: http://doi.org/10.18700/jnc.210018
Abstract
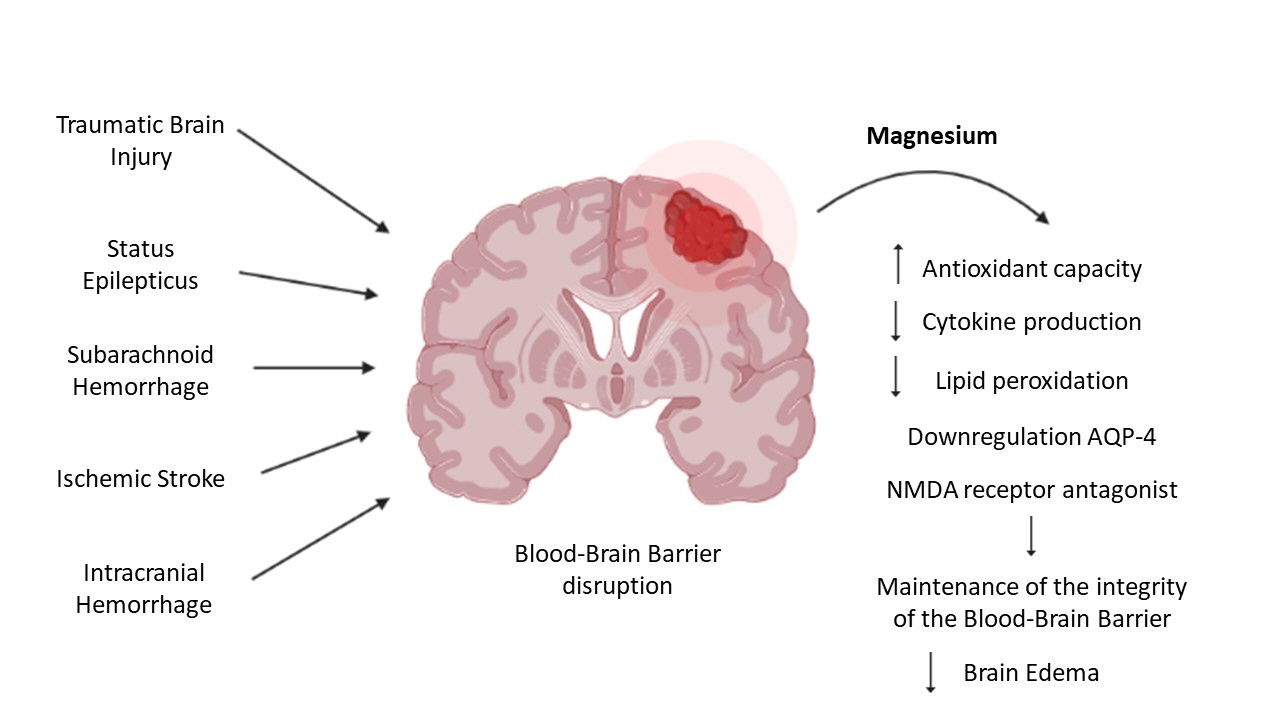
- Magnesium is an essential chemical element in human life. In the brain, it is physiologically responsible for a large number of processes involved in intracellular homeostasis, blood-brain barrier integrity, protein synthesis, neuronal proliferation, aging, and apoptosis. Considering that neurocritical care is a relatively new discipline in certain regions of the world and is an independent protective factor of neurological diseases in critical care, it is essential to disseminate basic concepts and utilities of tools that can positively impact the neurological disease burden. Magnesium and its use in neurocritical care are poorly understood. Therefore, this study aimed to review basic concepts regarding the physiology of magnesium in neurological dynamics, its role in the pathophysiology of neurological disorders, and the outcome of its use in the management of neurocritical illnesses.
Figure
Reference
-
1. Vink R, Nechifor M. Magnesium in the central nervous system. Adelaide: University of Adelaide Press;2011.2. Wolahan SM, Hirt D, Glenn TC. Translational metabolomics of head injury: exploring dysfunctional cerebral metabolism with ex vivo NMR spectroscopy-based metabolite quantification. In : Kobeissy FH, editor. Brain neurotrauma: molecular, neuropsychological, and rehabilitation aspects. Boca Raton, FL: CRC Press/Taylor & Francis;2015.3. Botturi A, Ciappolino V, Delvecchio G, Boscutti A, Viscardi B, Brambilla P. The role and the effect of magnesium in mental disorders: a systematic review. Nutrients. 2020; 12:1661.
Article4. Xue W, You J, Su Y, Wang Q. The effect of magnesium deficiency on neurological disorders: a narrative review article. Iran J Public Health. 2019; 48:379–87.5. Chang JJ, Armonda R, Goyal N, Arthur AS. Magnesium: pathophysiological mechanisms and potential therapeutic roles in intracerebral hemorrhage. Neural Regen Res. 2019; 14:1116–21.
Article6. Maas AI, Murray GD. Magnesium for neuroprotection after traumatic brain injury. Lancet Neurol. 2007; 6:20–1.
Article7. Kramer AH, Couillard P. Neurocritical care: a growing international collaborative. Neurocrit Care. 2020; 32:80–3.
Article8. Porcayo-Liborio S, Rivera-Durón E, Orta-San-Juan D. The evolution of neuro-critical care in Mexico. Rev Mex Anest. 2010; 33:50–5.9. Suarez JI, Zaidat OO, Suri MF, Feen ES, Lynch G, Hickman J, et al. Length of stay and mortality in neurocritically ill patients: impact of a specialized neurocritical care team. Crit Care Med. 2004; 32:2311–7.
Article10. Varelas PN, Conti MM, Spanaki MV, Potts E, Bradford D, Sunstrom C, et al. The impact of a neurointensivist-led team on a semiclosed neurosciences intensive care unit. Crit Care Med. 2004; 32:2191–8.
Article11. World Health Organization. Global burden of neurological disorders: estimates and projections [Internet]. Geneva: World Health Organization;2007. [cited 2021 Jun 14]. Available from: https://www.who.int/mental_health/neurology/chapter_2_neuro_disorders_public_h_challenges.pdf.12. Amory CF, Varelas PN. Magnesium and hydrogen in subarachnoid hemorrhage: is neuroprotection finally a reality? Stroke. 2021; 52:28–30.13. Dorhout Mees SM, Algra A, Vandertop WP, van Kooten F, Kuijsten HA, Boiten J, et al. Magnesium for aneurysmal subarachnoid haemorrhage (MASH-2): a randomised placebo-controlled trial. Lancet. 2012; 380:44–9.14. van den Bergh WM, Dijkhuizen RM, Rinkel GJ. Potentials of magnesium treatment in subarachnoid haemorrhage. Magnes Res. 2004; 17:301–13.15. van den Bergh WM, Algra A, van Kooten F, Dirven CM, van Gijn J, Vermeulen M, et al. Magnesium sulfate in aneurysmal subarachnoid hemorrhage: a randomized controlled trial. Stroke. 2005; 36:1011–5.16. Venkatasubba Rao CP, Suarez JI. Magnesium and neuroprotection in subarachnoid haemorrhage. Lancet. 2012; 380:9–11.
Article17. Wong GK, Poon WS. Magnesium sulphate for aneurysmal subarachnoid hemorrhage: why, how, and current controversy. Acta Neurochir Suppl. 2013; 115:45–8.
Article18. Altman D, Carroli G, Duley L, Farrell B, Moodley J, Neilson J, et al. Do women with pre-eclampsia, and their babies, benefit from magnesium sulphate? The Magpie trial: a randomised placebo-controlled trial. Lancet. 2002; 359:1877–90.19. Belfort MA, Anthony J, Saade GR, Allen JC Jr; Nimodipine Study Group. A comparison of magnesium sulfate and nimodipine for the prevention of eclampsia. N Engl J Med. 2003; 348:304–11.
Article20. McLean RM; Nimodipine Study Group. Magnesium and its therapeutic uses: a review. Am J Med. 1994; 96:63–76.
Article21. McKee JA, Brewer RP, Macy GE, Borel CO, Reynolds JD, Warner DS. Magnesium neuroprotection is limited in humans with acute brain injury. Neurocrit Care. 2005; 2:342–51.
Article22. Li W, Bai YA, Li YJ, Liu KG, Wang MD, Xu GZ, et al. Magnesium sulfate for acute traumatic brain injury. J Craniofac Surg. 2015; 26:393–8.
Article23. Sitzia C, Sterlicchio M, Crapanzano C, Dozio E, Vianello E, Corsi Romanelli MM. Intra-erythrocytes magnesium deficiency could reflect cognitive impairment status due to vascular disease: a pilot study. J Transl Med. 2020; 18:458.
Article24. Jahnen-Dechent W, Ketteler M. Magnesium basics. Clin Kidney J. 2012; 5(Suppl 1):i3–14.
Article25. Barbosa FT, Barbosa LT, Jucá MJ, Cunha RM. Applications of magnesium sulfate in obstetrics and anesthesia. Rev Bras Anestesiol. 2010; 60:104–10.
Article26. Volpe SL. Magnesium in disease prevention and overall health. Adv Nutr. 2013; 4:378S–383S.
Article27. Gröber U, Schmidt J, Kisters K. Magnesium in prevention and therapy. Nutrients. 2015; 7:8199–226.
Article28. Stangherlin A, O'Neill JS. Signal transduction: magnesium manifests as a second messenger. Curr Biol. 2018; 28:R1403–5.29. Seyama T, Kamei Y, Iriyama T, Imada S, Ichinose M, Toshimitsu M, et al. Pretreatment with magnesium sulfate attenuates white matter damage by preventing cell death of developing oligodendrocytes. J Obstet Gynaecol Res. 2018; 44:601–7.
Article30. Sun Q, Weinger JG, Mao F, Liu G. Regulation of structural and functional synapse density by L-threonate through modulation of intraneuronal magnesium concentration. Neuropharmacology. 2016; 108:426–39.
Article31. Spasov AA, Iezhitsa IN, Kravchenko MS, Kharitonova MV. Features of central neurotransmission in animals in conditions of dietary magnesium deficiency and after its correction. Neurosci Behav Physiol. 2009; 39:645–53.
Article32. Yamanaka R, Shindo Y, Oka K. Magnesium is a key player in neuronal maturation and neuropathology. Int J Mol Sci. 2019; 20:3439.
Article33. Matsui Y, Funato Y, Imamura H, Miki H, Mizukami S, Kikuchi K. Visualization of long-term Mg2+ dynamics in apoptotic cells using a novel targetable fluorescent probe. Chem Sci. 2017; 8:8255–64.
Article34. Ortega-Sierra MG, Durán-Daza RM, Carrera-Patiño SA, Rojas-Nuñez AX, Charry-Caicedo JI, Lozada-Martínez ID. Neuroeducation and neurorehabilitation in the neurosurgical patient: programs to be developed in Latin America and the Caribbean. J Neurosurg Sci. 2021; Jun. 10. [Epub]. https://doi.org/10.23736/S0390-5616.21.05439-4.
Article35. Abbott NJ. Evidence for bulk flow of brain interstitial fluid: significance for physiology and pathology. Neurochem Int. 2004; 45:545–52.
Article36. Abbott NJ, Patabendige AA, Dolman DE, Yusof SR, Begley DJ. Structure and function of the blood-brain barrier. Neurobiol Dis. 2010; 37:13–25.
Article37. Abbott NJ, Romero IA. Transporting therapeutics across the blood-brain barrier. Mol Med Today. 1996; 2:106–13.
Article38. Allsop TF. Transfer of magnesium across the perfused choroid plexus of sheep. Aust J Biol Sci. 1986; 39:161–9.
Article39. Allsop TF, Pauli JV. Magnesium concentrations in the ventricular and lumbar cerebrospinal fluid of hypomagnesaemic cows. Res Vet Sci. 1985; 38:61–4.
Article40. Agre P, Preston GM, Smith BL, Jung JS, Raina S, Moon C, et al. Aquaporin CHIP: the archetypal molecular water channel. Am J Physiol. 1993; 265(4 Pt 2):F463–76.
Article41. Amiry-Moghaddam M, Ottersen OP. The molecular basis of water transport in the brain. Nat Rev Neurosci. 2003; 4:991–1001.
Article42. Butt AM, Jones HC, Abbott NJ. Electrical resistance across the blood-brain barrier in anaesthetized rats: a developmental study. J Physiol. 1990; 429:47–62.
Article43. Bara M, Guiet-Bara A. Potassium, magnesium and membranes: review of present status and new findings. Magnesium. 1984; 3:215–25.44. Martin KJ, González EA, Slatopolsky E. Clinical consequences and management of hypomagnesemia. J Am Soc Nephrol. 2009; 20:2291–5.
Article45. Panahi Y, Mojtahedzadeh M, Najafi A, Ghaini MR, Abdollahi M, Sharifzadeh M, et al. The role of magnesium sulfate in the intensive care unit. EXCLI J. 2017; 16:464–82.46. Gragossian A, Bashir K, Friede R. Hypomagnesemia. Treasure Island, FL: StatPearls Publishing;2021.47. Pham PC, Pham PA, Pham SV, Pham PT, Pham PM, Pham PT. Hypomagnesemia: a clinical perspective. Int J Nephrol Renovasc Dis. 2014; 7:219–30.
Article48. Van Laecke S. Hypomagnesemia and hypermagnesemia. Acta Clin Belg. 2019; 74:41–7.
Article49. Broman M, Hansson F, Klarin B. Analysis of hypo- and hypermagnesemia in an intensive care unit cohort. Acta Anaesthesiol Scand. 2018; 62:648–57.
Article50. Cascella M, Vaqar S. Hypermagnesemia. Treasure Island, FL: StatPearls Publishing;2021.51. Topf JM, Murray PT. Hypomagnesemia and hypermagnesemia. Rev Endocr Metab Disord. 2003; 4:195–206.52. Schelling JR. Fatal hypermagnesemia. Clin Nephrol. 2000; 53:61–5.53. Bokhari SR, Siriki R, Teran FJ, Batuman V. Fatal hypermagnesemia due to laxative use. Am J Med Sci. 2018; 355:390–5.
Article54. Gomes D, Pimentel J, Bentes C, Aguiar de Sousa D, Antunes AP, Alvarez A, et al. Consensus protocol for the treatment of super-refractory status epilepticus. Acta Med Port. 2018; 31:598–605.
Article55. Zeiler FA, Matuszczak M, Teitelbaum J, Gillman LM, Kazina CJ. Magnesium sulfate for non-eclamptic status epilepticus. Seizure. 2015; 32:100–8.
Article56. Kirkland AE, Sarlo GL, Holton KF. The role of magnesium in neurological disorders. Nutrients. 2018; 10:730.
Article57. Macías-Ruíz VS, Cordero-Pérez MB, Vásquez-Cedeño DA, Saltos-Mata F. Factors associated with mortality of spontaneous intraparenchymal cerebral hemorrhage in patients over 50 years of age who attended the teodoro maldonado carbo hospital during the year 2017. Rev Ecuat Neurol. 2019; 28:10–5.58. Jafari M, Di Napoli M, Lattanzi S, Mayer SA, Bachour S, Bershad EM, et al. Serum magnesium level and hematoma expansion in patients with intracerebral hemorrhage. J Neurol Sci. 2019; 398:39–44.
Article59. Liotta EM, Prabhakaran S, Sangha RS, Bush RA, Long AE, Trevick SA, et al. Magnesium, hemostasis, and outcomes in patients with intracerebral hemorrhage. Neurology. 2017; 89:813–9.
Article60. Mejía C JA, Niño de Mejía MC, Ferrer Z LE, Cohen MD. Cerebral vasospasm secondary to subarachnoid hemorrhage due to ruptured intracerebral aneurysm. Rev Colomb Anesthesiol. 2007; 35:143–62.61. Soliman R, Zohry G. Effect of magnesium sulphate and milrinone on cerebral vasospasm after aneurysmal subarachnoid hemorrhage: a randomized study. Braz J Anesthesiol. 2019; 69:64–71.
Article62. Findlay JM, Nisar J, Darsaut T. Cerebral vasospasm: a review. Can J Neurol Sci. 2016; 43:15–32.
Article63. Larsson SC, Traylor M, Burgess S, Boncoraglio GB, Jern C, Michaëlsson K, et al. Serum magnesium and calcium levels in relation to ischemic stroke: Mendelian randomization study. Neurology. 2019; 92:e944–50.64. Lai TW, Zhang S, Wang YT. Excitotoxicity and stroke: identifying novel targets for neuroprotection. Prog Neurobiol. 2014; 115:157–88.
Article65. Saver JL, Kidwell C, Eckstein M, Starkman S; FAST-MAG Pilot Trial Investigators. Prehospital neuroprotective therapy for acute stroke: results of the Field Administration of Stroke Therapy-Magnesium (FAST-MAG) pilot trial. Stroke. 2004; 35:e106–8.
Article66. Saver JL, Starkman S, Eckstein M, Stratton SJ, Pratt FD, Hamilton S, et al. Prehospital use of magnesium sulfate as neuroprotection in acute stroke. N Engl J Med. 2015; 372:528–36.
Article67. Shkirkova K, Starkman S, Sanossian N, Eckstein M, Stratton S, Pratt F, et al. Paramedic initiation of neuroprotective agent infusions: successful achievement of target blood levels and attained level effect on clinical outcomes in the FAST-MAG pivotal trial (field administration of stroke therapy-magnesium). Stroke. 2017; 48:1901–7.68. Pan WH, Lai YH, Yeh WT, Chen JR, Jeng JS, Bai CH, et al. Intake of potassium- and magnesium-enriched salt improves functional outcome after stroke: a randomized, multicenter, double-blind controlled trial. Am J Clin Nutr. 2017; 106:1267–73.
Article69. Bechler K, Shkirkova K, Saver JL, Starkman S, Hamilton S, Liebeskind DS, et al. The effect of early treatment with intravenous magnesium sulfate on the incidence of cardiac comorbidities in hospitalized stroke patients. Cardiovasc Ther. 2020; 2020:1494506.
Article70. Wong GK, Poon WS, Chan MT, Boet R, Gin T, Ng SC, et al. Intravenous magnesium sulphate for aneurysmal subarachnoid hemorrhage (IMASH): a randomized, double-blinded, placebo-controlled, multicenter phase III trial. Stroke. 2010; 41:921–6.71. Takeuchi S, Kumagai K, Toyooka T, Otani N, Wada K, Mori K. Intravenous hydrogen therapy with intracisternal magnesium sulfate infusion in severe aneurysmal subarachnoid hemorrhage. Stroke. 2021; 52:20–7.
Article72. Fang X, Wang K, Han D, He X, Wei J, Zhao L, et al. Dietary magnesium intake and the risk of cardiovascular disease, type 2 diabetes, and all-cause mortality: a dose-response meta-analysis of prospective cohort studies. BMC Med. 2016; 14:210.
Article73. Xu R, Wang L, Sun L, Dong J. Neuroprotective effect of magnesium supplementation on cerebral ischemic diseases. Life Sci. 2021; 272:119257.
Article74. Lee JS, Han YM, Yoo DS, Choi SJ, Choi BH, Kim JH, et al. A molecular basis for the efficacy of magnesium treatment following traumatic brain injury in rats. J Neurotrauma. 2004; 21:549–61.
Article75. Stippler M, Fischer MR, Puccio AM, Wisniewski SR, Carson-Walter EB, Dixon CE, et al. Serum and cerebrospinal fluid magnesium in severe traumatic brain injury outcome. J Neurotrauma. 2007; 24:1347–54.
Article76. Godoy DA, Pahnke P, Piñero GR, Videtta W, Aguilera S. Intensive care in severe cranioencephalic trauma. Neurociencias Colomb. 2016; 23:193–220.77. Lyons MW, Blackshaw WJ. Does magnesium sulfate have a role in the management of severe traumatic brain injury in civilian and military populations? A systematic review and meta-analysis. J R Army Med Corps. 2018; 164:442–9.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Optimal and Safe Bowel Preparation for Colonoscopy
- A comparison of ritodrine and magnesium sulfate for the suppression of preterm labor
- Magnesium Sulfate in the Treatment of Torsade De Pointes
- Magnesium: a versatile drug for anesthesiologists
- A Comparison of Efficacy and Safety of Ritodrine hydrochloride alone and Combined Treatment with Magnesium sulfate in the Management of Preterm Labor