J Korean Med Sci.
2024 Jun;39(23):e187. 10.3346/jkms.2024.39.e187.
Impact of the Early COVID-19 Pandemic on Emergency Department Visits of Adult Cancer Patients With Fever or Respiratory Symptoms: A Korean Nationwide Population-Based Study, 2016–2020
- Affiliations
-
- 1Public Health Research Institute, National Medical Center, Seoul, Korea
- 2National Emergency Medical Center, National Medical Center, Seoul, Korea
- 3Department of Pediatrics, National Medical Center, Seoul, Korea
- 4Department of Preventive Medicine, Chungnam National University College of Medicine, Daejeon, Korea
- KMID: 2556681
- DOI: http://doi.org/10.3346/jkms.2024.39.e187
Abstract
- Background
We performed a nationwide analysis to evaluate the impact of the early coronavirus disease 2019 (COVID-19) pandemic on emergency department (ED) visits by adult cancer patients having COVID-like symptoms.
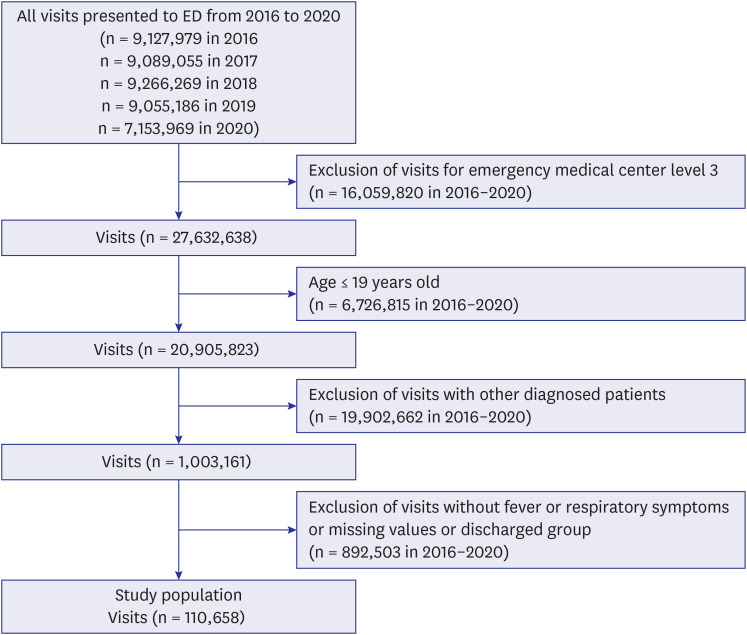
Methods
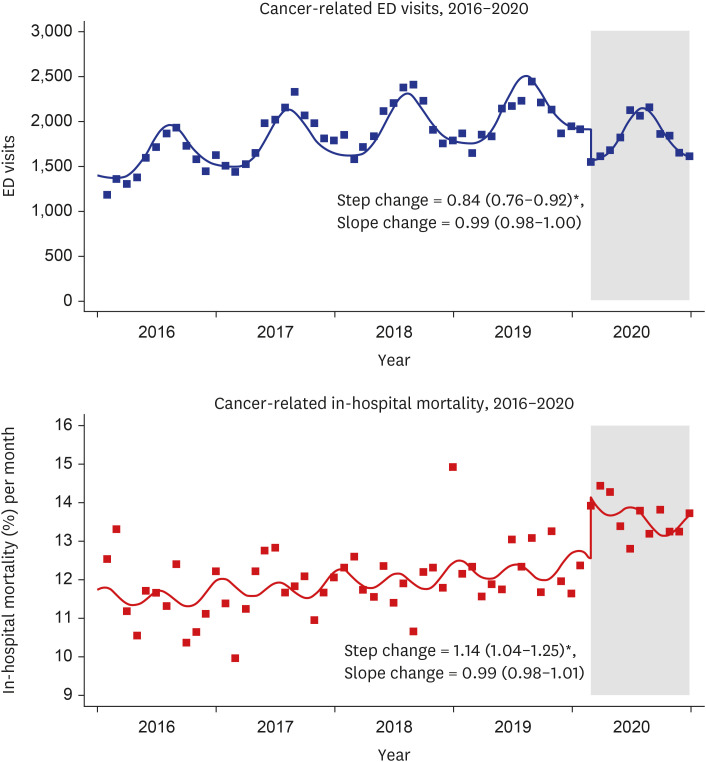
We analyzed the National Emergency Department Information System (NEDIS) data on ED visits by adult cancer patients who presented with chief complaints of fever or respiratory symptoms (FRS) indicative of COVID-19, from 2016 to 2020. An interrupted time series analysis with a quasi-Poisson regression model was performed, adjusting for seasonality and time, to evaluate whether underlying trends for monthly ED visits and the in-hospital mortality rate (%) per month changed with the pandemic among these patients. We also estimated the adjusted odds ratio (aOR) of in-hospital deaths among cancer patients using multivariable logistic regression analysis.
Results
ED visits by cancer patients with FRS decreased during the COVID-19 pandemic (relative risk [RR] with 95% confidence interval [CI]: slope change, 0.99 [0.98–1.00] and step change, 0.84 [0.76–0.92]). However, the in-hospital mortality rate (%) for these patients was increased (slope change, 1.14 [1.04–1.25] and step change, 0.99 [0.98–1.01]). Factors such as urgent triage status, ambulance use, and treatment in hospitals with fewer than 300 staffed beds significantly contributed to increased aOR of in-hospital deaths during the COVID-19 pandemic compared to the pre-pandemic period.
Conclusion
Further studies are needed to highlight the importance of ED service preparation in planning and managing resources for cancer patients during future pandemics.
Keyword
Figure
Reference
-
1. Şan İ, Usul E, Bekgöz B, Korkut S. Effects of COVID‐19 pandemic on emergency medical services. Int J Clin Pract. 2021; 75(5):e13885. PMID: 33280198.2. Nuñez JH, Sallent A, Lakhani K, Guerra-Farfan E, Vidal N, Ekhtiari S, et al. Impact of the COVID-19 pandemic on an emergency traumatology service: experience at a tertiary trauma centre in Spain. Injury. 2020; 51(7):1414–1418. PMID: 32405089.3. Lee DE, Ro YS, Ryoo HW, Moon S. Impact of temporary closures of emergency departments during the COVID-19 outbreak on clinical outcomes for emergency patients in a metropolitan area. Am J Emerg Med. 2021; 47:35–41. PMID: 33756131.4. Kim D, Jung W, Yu JY, Chang H, Lee SU, Kim T, et al. Effect of fever or respiratory symptoms on leaving without being seen during the COVID-19 pandemic in South Korea. Clin Exp Emerg Med. 2022; 9(1):1–9. PMID: 35354228.5. Lim D, Park SY, Choi B, Kim SH, Ryu JH, Kim YH, et al. The comparison of emergency medical service responses to and outcomes of out-of-hospital cardiac arrest before and during the COVID-19 pandemic in an area of Korea. J Korean Med Sci. 2021; 36(36):e255. PMID: 34519188.6. Yoon D, Kim KE, Lee JE, Kim M, Kim JH. Impact of the coronavirus disease 2019 (COVID-19) pandemic on medical use of military hospitals in Korea. J Korean Med Sci. 2021; 36(28):e204. PMID: 34282607.7. Rivera DR, Gallicchio L, Brown J, Liu B, Kyriacou DN, Shelburne N. Trends in adult cancer–related emergency department utilization: an analysis of data from the nationwide emergency department sample. JAMA Oncol. 2017; 3(10):e172450. PMID: 28859189.8. Lee SY, Ro YS, Shin SD, Moon S. Epidemiologic trends in cancer-related emergency department utilization in Korea from 2015 to 2019. Sci Rep. 2021; 11(1):21981. PMID: 34754058.9. Min HS, Chang HJ, Sung HK. Emergency department utilization of adult cancer patient in Korea: a nationwide population-based study, 2017-2019. Cancer Res Treat. 2022; 54(3):680–689. PMID: 34583460.10. Hsu J, Donnelly JP, Moore JX, Meneses K, Williams G, Wang HE. National characteristics of Emergency Department visits by patients with cancer in the United States. Am J Emerg Med. 2018; 36(11):2038–2043. PMID: 29573899.11. Patt D, Gordan L, Diaz M, Okon T, Grady L, Harmison M, et al. Impact of COVID-19 on cancer care: how the pandemic is delaying cancer diagnosis and treatment for American seniors. JCO Clin Cancer Inform. 2020; 4(4):1059–1071. PMID: 33253013.12. Lee S, Lim AR, Kim MJ, Choi YJ, Kim JW, Park KH, et al. Innovative countermeasures can maintain cancer care continuity during the coronavirus disease-2019 pandemic in Korea. Eur J Cancer. 2020; 136:69–75. PMID: 32652443.13. Lee KS, Min HS, Moon JY, Lim D, Kim Y, Ko E, et al. Patient and hospital characteristics predict prolonged emergency department length of stay and in-hospital mortality: a nationwide analysis in Korea. BMC Emerg Med. 2022; 22(1):183. PMID: 36411433.14. Fitzner J, Qasmieh S, Mounts AW, Alexander B, Besselaar T, Briand S, et al. Revision of clinical case definitions: influenza-like illness and severe acute respiratory infection. Bull World Health Organ. 2018; 96(2):122–128. PMID: 29403115.15. Yoo SH, Sim JA, Shin J, Keam B, Park JB, Shin A. The impact of COVID-19 on cancer care in a tertiary hospital in Korea: possible collateral damage to emergency care. Epidemiol Health. 2022; 44:e2022044. PMID: 35538696.16. Bernal JL, Cummins S, Gasparrini A. Interrupted time series regression for the evaluation of public health interventions: a tutorial. Int J Epidemiol. 2017; 46(1):348–355. PMID: 27283160.17. Han C. Changes in mortality rate of the general population during the COVID-19 pandemic: an interrupted time series study in Korea. Int J Epidemiol. 2022; 51(5):1396–1407. PMID: 35462402.18. Kong M, Cambon A, Smith MJ. Extended logistic regression model for studies with interrupted events, seasonal trend, and serial correlation. Commun Stat Theory Methods. 2012; 41(19):3528–3543.19. Cohen BA, Wessling EG, Serina PT, Cruz DS, Kim HS, McCarthy DM, et al. Emergency department operations in a large health system during COVID-19. Am J Emerg Med. 2021; 41:241–243. PMID: 32505468.20. Kim YS, Kim IB, Kim SR, Cho BJ. Changes in emergency department case severity and length of stay before and after COVID-19 outbreak in Korea. Healthcare (Basel). 2022; 10(8):1540. PMID: 36011197.21. Kalolo A, Gautier L, Radermacher R, Srivastava S, Meshack M, De Allegri M. Factors influencing variation in implementation outcomes of the redesigned community health fund in the Dodoma region of Tanzania: a mixed-methods study. BMC Public Health. 2021; 21(1):1. PMID: 33388037.22. Çıkrıkçı Işık G, Çevik Y. Impact of COVID-19 pandemic on visits of an urban emergency department. Am J Emerg Med. 2021; 42:78–82. PMID: 33493832.23. Gutovitz S, Pangia J, Finer A, Rymer K, Johnson D. Emergency department utilization and patient outcomes during the COVID-19 pandemic in America. J Emerg Med. 2021; 60(6):798–806. PMID: 33581990.24. Wai AK, Wong CK, Wong JY, Xiong X, Chu OC, Wong MS, et al. Changes in emergency department visits, diagnostic groups, and 28-day mortality associated with the COVID-19 pandemic: a territory-wide, retrospective, cohort study. Ann Emerg Med. 2022; 79(2):148–157. PMID: 34742591.25. Alharthi S, Al-Moteri M, Plummer V, Al Thobiaty A. The impact of COVID-19 on the service of emergency department. Healthcare (Basel). 2021; 9(10):1295. PMID: 34682975.26. Kang S, Ahn TK, Seo YH, Suh YJ, Paik JH. Comparison of emergency department utilization trends between the COVID-19 pandemic and control period. Medicine (Baltimore). 2021; 100(32):e26847. PMID: 34397892.27. Ha JY, Sung WY. Impact of COVID-19 pandemic on emergency department length of stay and clinical outcomes of patients with severe pneumonia: a single-center observational study. Medicine (Baltimore). 2022; 101(38):e30633. PMID: 36197269.28. Lee SJ, Choi A, Ryoo HW, Pak YS, Kim HC, Kim JH. Changes in clinical characteristics among febrile patients visiting the emergency department before and after the COVID-19 outbreak. Yonsei Med J. 2021; 62(12):1136–1144. PMID: 34816644.29. Alquézar-Arbé A, Piñera P, Jacob J, Martín A, Jiménez S, Llorens P, et al. Impact of the COVID-19 pandemic on hospital emergency departments: results of a survey of departments in 2020 - the Spanish ENCOVUR study. Emergencias (Madr). 2020; 32(5):320–331.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Impact of the COVID-19 Pandemic on Esophagogastroduodenoscopy and Gastric Cancer Claims in South Korea: A Nationwide, Population-Based Study
- The elderly population are more vulnerable for the management of colorectal cancer during the COVID-19 pandemic: a nationwide, population-based study
- The impact of the COVID-19 pandemic on clinical practices related to colorectal cancer and colonoscopy in South Korea: a nationwide population-based study
- Impact of the COVID-19 Outbreak on Emergency Care Utilization in Patients with Acute Myocardial Infarction: a Nationwide Population-based Study
- Effect of fever or respiratory symptoms on leaving without being seen during the COVID-19 pandemic in South Korea