Intest Res.
2023 Oct;21(4):500-509. 10.5217/ir.2023.00004.
The elderly population are more vulnerable for the management of colorectal cancer during the COVID-19 pandemic: a nationwide, population-based study
- Affiliations
-
- 1Department of Internal Medicine, Kyung Hee University Hospital at Gangdong, College of Medicine, Kyung Hee University, Seoul, Korea
- KMID: 2547200
- DOI: http://doi.org/10.5217/ir.2023.00004
Abstract
- Background/Aims
The impact of coronavirus disease 2019 (COVID-19) on the management of colorectal cancer (CRC) may worse in elderly population, as almost all COVID-19 deaths occurred in the elderly patients. This study aimed to evaluate the impact of COVID-19 on CRC management in the elderly population.
Methods
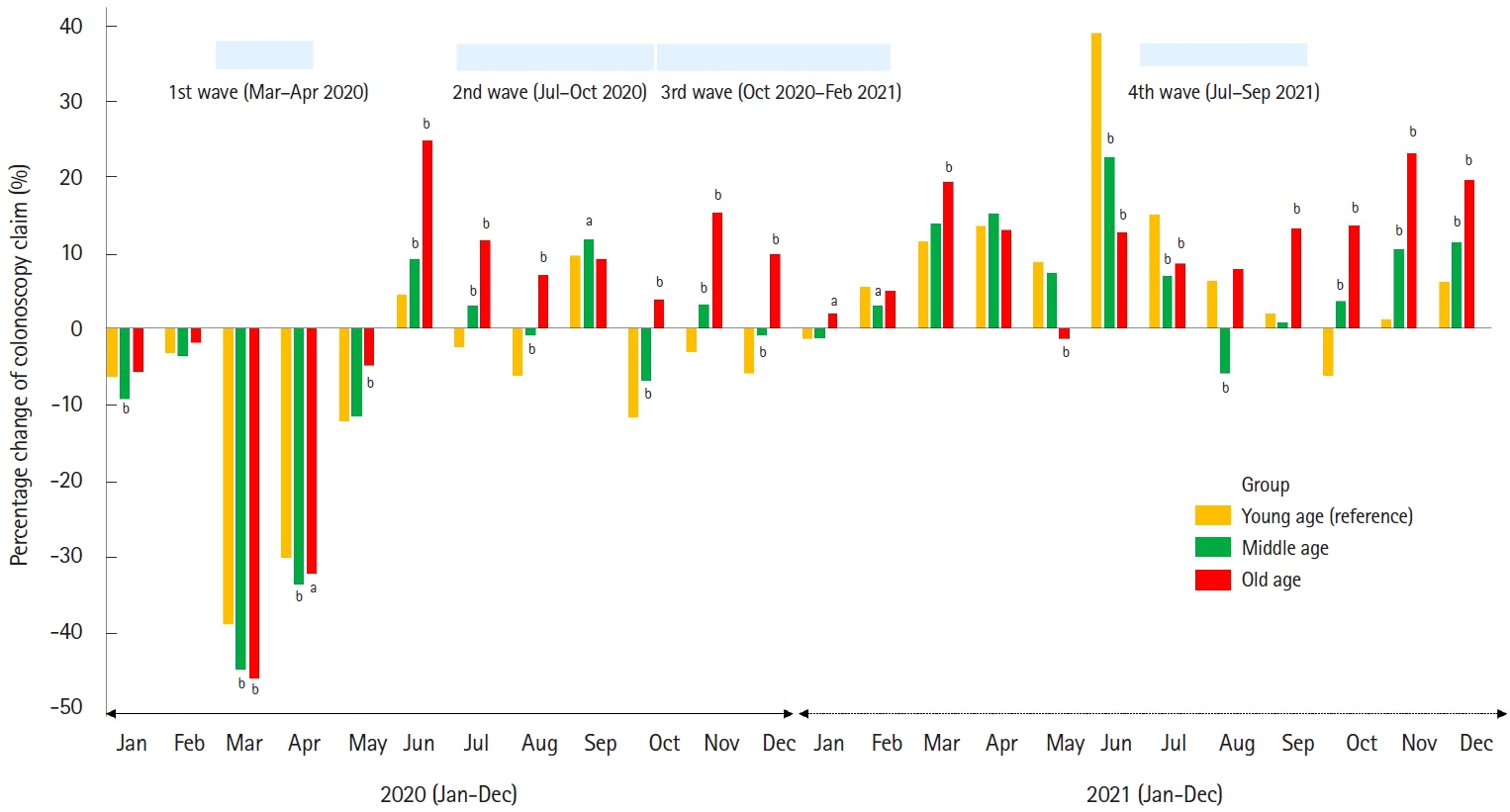
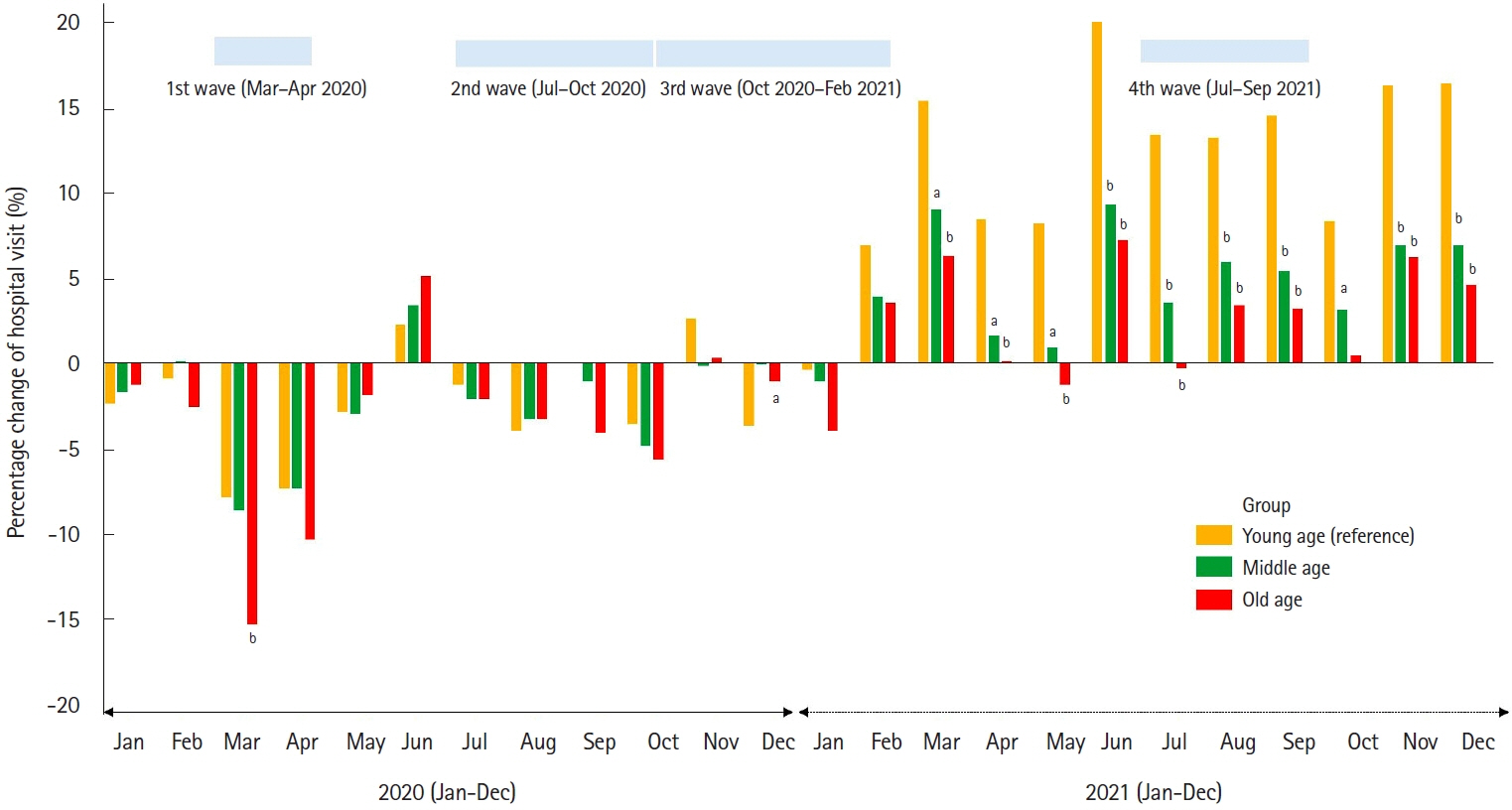
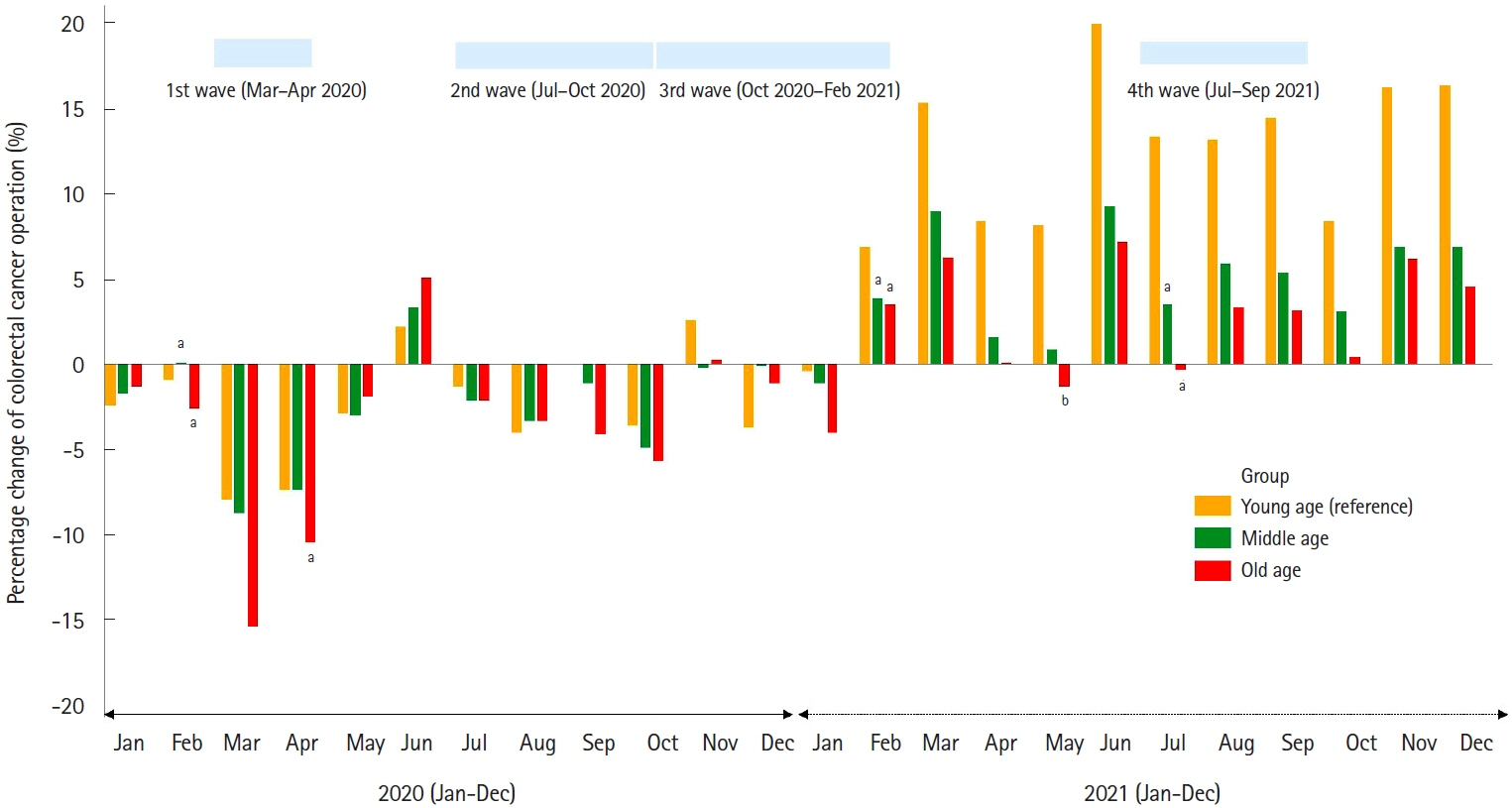
The numbers of patients who underwent colonoscopy, who visited hospitals or operated for CRC in 2020 and 2021 (COVID-19 era) were compared with those in 2019, according to 3 age groups (≥70 years, 50–69 years, and ≤49 years), based on the nationwide, population-based database (2019–2021) in South Korea.
Results
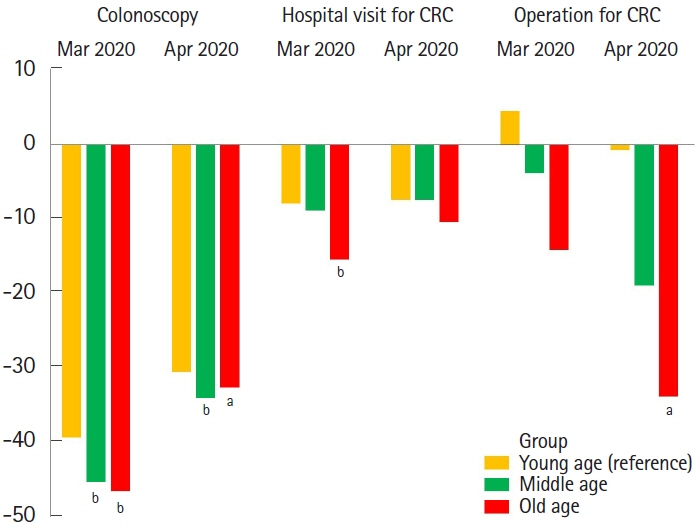
The annual volumes of colonoscopy and hospital visits for CRC in 2020 were more significantly declined in the old age group than in the young age group (both P<0.001). In addition, the annual volume of patients operated for CRC numerically more declined in old age group than in young age group. During the first surge of COVID-19 (March and April 2020), old age patients showed statistically significant declines for the monthly number of colonoscopies (–46.5% vs. –39.3%, P<0.001), hospital visits (–15.4% vs. –7.9%, P<0.001), CRC operations (–33.8% vs. –0.7%, P<0.05), and colonoscopic polypectomies (–41.8% vs. –38.0%, P<0.001) than young age patients, compared with those of same months in 2019.
Conclusions
Elderly population are more vulnerable for the management of CRC during the COVID-19 pandemic. Therefore, the elderly population are more carefully cared for in the management of CRC during the next pandemic.
Keyword
Figure
Cited by 1 articles
-
To overcome medical gap in screening and surveillance of colorectal cancer during the COVID-19 pandemic
Yoo Min Han
Intest Res. 2023;21(4):418-419. doi: 10.5217/ir.2023.00144.
Reference
-
1. Jee Y, Kim YJ, Oh J, Kim YJ, Ha EH, Jo I. A COVID-19 mortality prediction model for Korean patients using nationwide Korean disease control and prevention agency database. Sci Rep. 2022; 12:3311.
Article2. Sultan S, Lim JK, Altayar O, et al. AGA rapid recommendations for gastrointestinal procedures during the COVID-19 pandemic. Gastroenterology. 2020; 159:739–758.
Article3. Lee JB, Jung M, Kim JH, et al. Guidelines for cancer care during the COVID-19 pandemic in South Korea. Cancer Res Treat. 2021; 53:323–329.
Article4. Morris EJ, Goldacre R, Spata E, et al. Impact of the COVID-19 pandemic on the detection and management of colorectal cancer in England: a population-based study. Lancet Gastroenterol Hepatol. 2021; 6:199–208.
Article5. Lui TK, Leung K, Guo CG, Tsui VW, Wu JT, Leung WK. Impacts of the coronavirus 2019 pandemic on gastrointestinal endoscopy volume and diagnosis of gastric and colorectal cancers: a population-based study. Gastroenterology. 2020; 159:1164–1166.
Article6. Dessie ZG, Zewotir T. Mortality-related risk factors of COVID-19: a systematic review and meta-analysis of 42 studies and 423,117 patients. BMC Infect Dis. 2021; 21:855.
Article7. Pijls BG, Jolani S, Atherley A, et al. Demographic risk factors for COVID-19 infection, severity, ICU admission and death: a meta-analysis of 59 studies. BMJ Open. 2021; 11:e044640.
Article8. Kim L, Kim JA, Kim S. A guide for the utilization of Health Insurance Review and Assessment Service National Patient Samples. Epidemiol Health. 2014; 36:e2014008.
Article9. Kim JA, Yoon S, Kim LY, Kim DS. Towards actualizing the value potential of Korea Health Insurance Review and Assessment (HIRA) data as a resource for health research: strengths, limitations, applications, and strategies for optimal use of HIRA data. J Korean Med Sci. 2017; 32:718–728.
Article10. Sung JJ, Ng SC, Chan FK, et al. An updated Asia Pacific Consensus Recommendations on colorectal cancer screening. Gut. 2015; 64:121–132.
Article11. Health Insurance Review and Assessmen. Standard guide to calculating disease behavior statistics [Internet]. c2021 [cited 2023 Jan 9]. http://opendata.hira.or.kr/co.apndFile.dir/download.do?fileNm=illnessBehavior.pdf.12. Khan A, Bilal M, Morrow V, Cooper G, Thakkar S, Singh S. Impact of the coronavirus disease 2019 pandemic on gastrointestinal procedures and cancers in the United States: a multicenter research network study. Gastroenterology. 2021; 160:2602–2604.
Article13. Lantinga MA, Theunissen F, Ter Borg PC, et al. Impact of the COVID-19 pandemic on gastrointestinal endoscopy in the Netherlands: analysis of a prospective endoscopy database. Endoscopy. 2021; 53:166–170.
Article14. Jeon J, Han C, Kim T, Lee S. Evolution of responses to COVID-19 and epidemiological characteristics in South Korea. Int J Environ Res Public Health. 2022; 19:4056.
Article15. Ho FK, Petermann-Rocha F, Gray SR, et al. Is older age associated with COVID-19 mortality in the absence of other risk factors? General population cohort study of 470,034 participants. PLoS One. 2020; 15:e0241824.
Article16. Damayanthi HD, Prabani KI, Weerasekara I. Factors associated for mortality of older people with COVID 19: a systematic review and meta-analysis. Gerontol Geriatr Med. 2021; 7:23337214211057392.17. Yanez ND, Weiss NS, Romand JA, Treggiari MM. COVID-19 mortality risk for older men and women. BMC Public Health. 2020; 20:1742.
Article18. Whaley CM, Pera MF, Cantor J, et al. Changes in health services use among commercially insured US populations during the COVID-19 pandemic. JAMA Netw Open. 2020; 3:e2024984.
Article19. Shaukat A, Church T. Colorectal cancer screening in the USA in the wake of COVID-19. Lancet Gastroenterol Hepatol. 2020; 5:726–727.
Article20. Gupta S, Lieberman D. Screening and surveillance colonoscopy and COVID-19: avoiding more casualties. Gastroenterology. 2020; 159:1205–1208.
Article21. Han YD, Oh TJ, Chung TH, et al. Early detection of colorectal cancer based on presence of methylated syndecan-2 (SDC2) in stool DNA. Clin Epigenetics. 2019; 11:51.
Article22. Yong JH, Mainprize JG, Yaffe MJ, et al. The impact of episodic screening interruption: COVID-19 and population-based cancer screening in Canada. J Med Screen. 2021; 28:100–107.
Article23. Maringe C, Spicer J, Morris M, et al. The impact of the COVID-19 pandemic on cancer deaths due to delays in diagnosis in England, UK: a national, population-based, modelling study. Lancet Oncol. 2020; 21:1023–1034.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- The impact of the COVID-19 pandemic on clinical practices related to colorectal cancer and colonoscopy in South Korea: a nationwide population-based study
- Impact of the COVID-19 Pandemic on Esophagogastroduodenoscopy and Gastric Cancer Claims in South Korea: A Nationwide, Population-Based Study
- Influence of the COVID-19 Pandemic on the Treatment Patterns and Outcomes of Colorectal Cancer
- The impact of COVID-19 on screening for colorectal, gastric, breast, and cervical cancer in Korea
- Residual Neuropsychiatric Sequelae of the Elderly and Neurocognitive Disorder Patients Who Recovered from Coronavirus Infection (COVID-19) : A review