J Korean Med Sci.
2024 Jun;39(23):e179. 10.3346/jkms.2024.39.e179.
Comparative Effectiveness of Personal Sound Amplification Products Versus Hearing Aids for Unilateral Hearing Loss: A Prospective Randomized Crossover Trial
- Affiliations
-
- 1Department of Otolaryngology-Head and Neck Surgery, Chungnam National University College of Medicine, Daejeon, Korea
- 2Department of Otolaryngology-Head and Neck Surgery, Chungnam National University Sejong Hospital, Chungnam National University College of Medicine, Sejong, Korea
- 3Brain Research Institute, College of Medicine, Chungnam National University, Daejeon, Korea
- KMID: 2556680
- DOI: http://doi.org/10.3346/jkms.2024.39.e179
Abstract
- Background
This study compared hearing outcomes with use of personal sound amplification products (PSAPs) and hearing aids (HAs) in patients with moderate to moderately severe unilateral hearing loss.
Methods
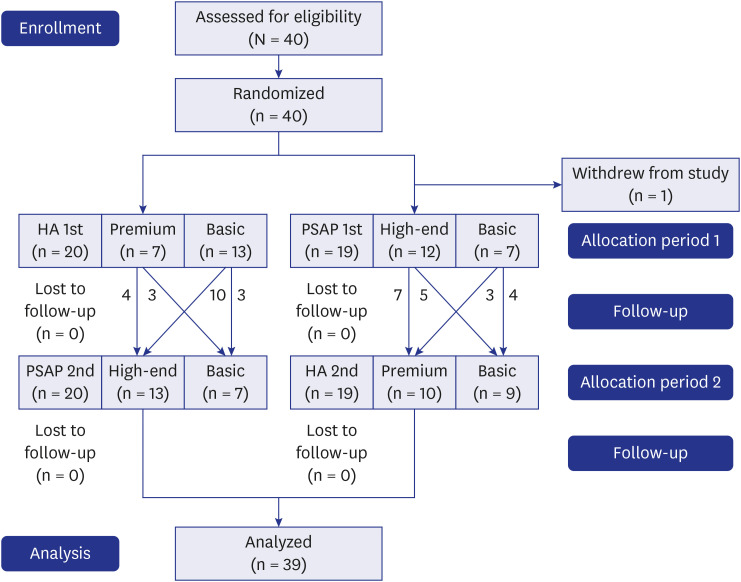
Thirty-nine participants were prospectively enrolled, and randomly assigned to use either one HA (basic or premium type) or one PSAP (basic or high-end type) for the first 8 weeks and then the other device for the following 8 weeks. Participants underwent a battery of examinations at three visits, including sound-field audiometry, word recognition score (WRS), speech perception in quiet and in noise, real-ear measurement, and self-report questionnaires.
Results
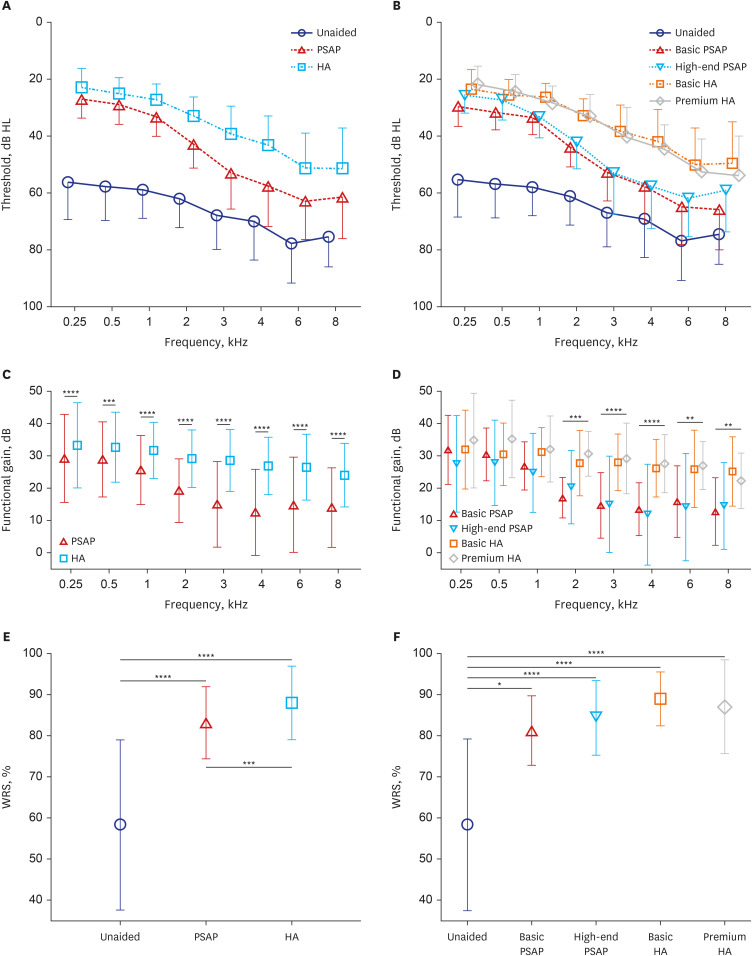
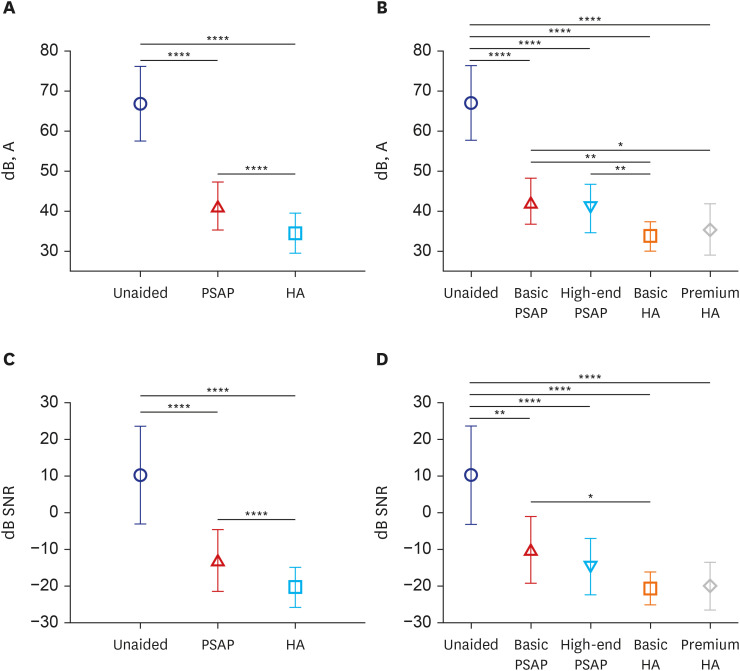
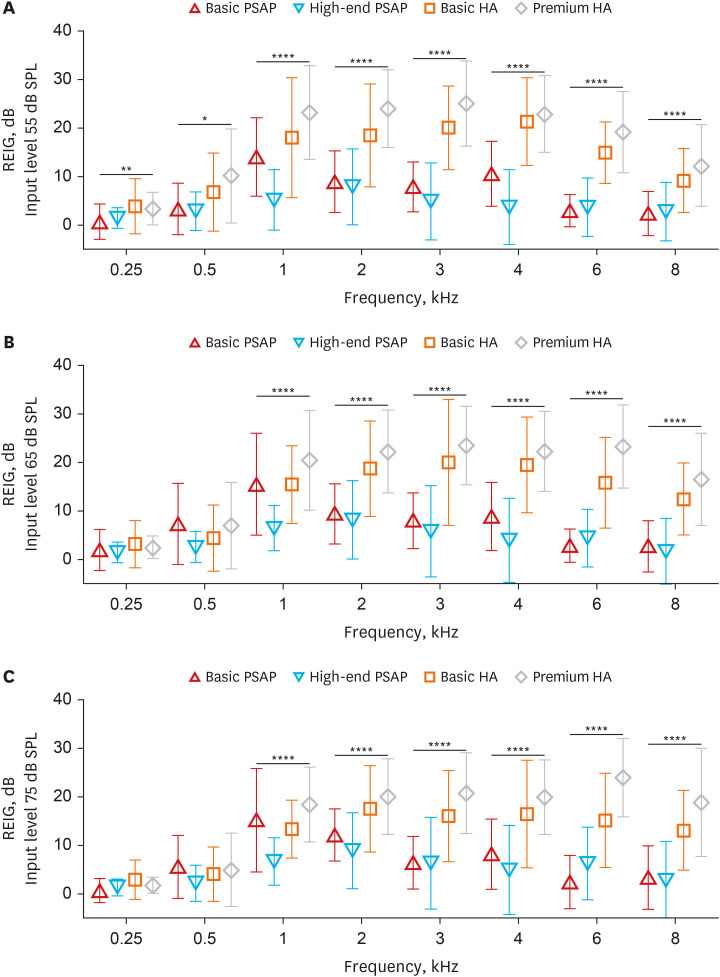
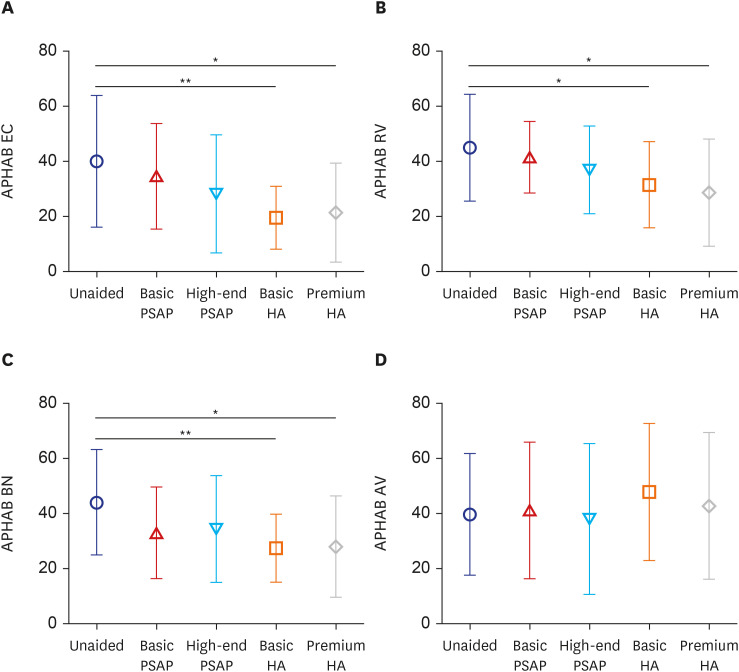
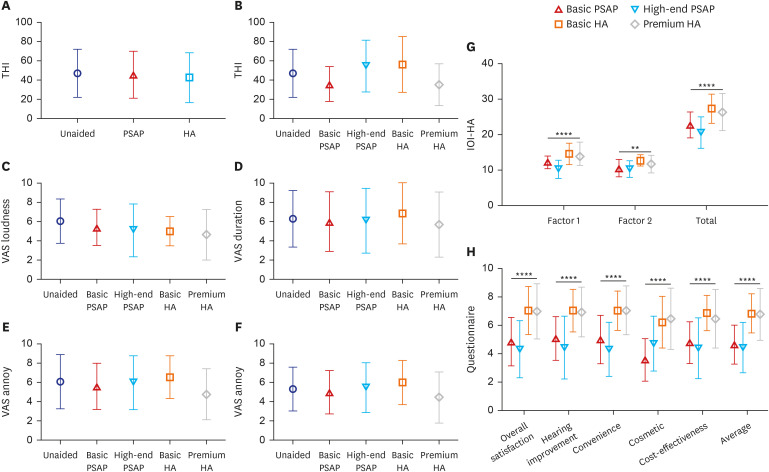
Functional gain was significantly higher with HAs across all frequencies (P < 0.001). While both PSAPs and HAs improved WRS from the unaided condition, HAs were superior to PSAPs. The speech recognition threshold in quiet conditions and signal-to-noise ratio in noisy conditions were significantly lower in the HA-aided condition than in the PSAP-aided condition, and in the PSAP-aided condition than in the unaided condition. Subjective satisfaction also favored HAs than PSAPs in questionnaires, Abbreviated Profile of Hearing Aid Benefit, International Outcome Inventory for Hearing Aids, and Host Institutional Questionnaire.
Conclusion
While PSAPs provide some benefit for moderate to moderately severe unilateral hearing loss, HAs are more effective. This underscores the potential role of PSAPs as an accessible, affordable first-line intervention in hearing rehabilitation, particularly for individuals facing challenges in accessing conventional HAs.
Figure
Reference
-
1. World Health Organization. Addressing the Rising Prevalence of Hearing Loss. Geneva, Switzerland: World Health Organization;2018.2. Mathers C, Smith A, Concha M. Global Burden of Hearing Loss in the Year 2000. Geneva, Switzerland: World Health Organization;2000. p. 1–30.3. Gates GA, Mills JH. Presbycusis. Lancet. 2005; 366(9491):1111–1120. PMID: 16182900.4. Choi J, Chung WH. Age-related hearing loss and the effects of hearing aids. J Korean Med Assoc. 2011; 54(9):918.5. Atef RZ, Michalowsky B, Raedke A, Platen M, Mohr W, Mühlichen F, et al. Impact of hearing aids on progression of cognitive decline, depression, and quality of life among people with cognitive impairment and dementia. J Alzheimers Dis. 2023; 92(2):629–638. PMID: 36776058.6. Dillard LK, Pinto A, Mueller KD, Schubert CR, Paulsen AJ, Merten N, et al. Associations of hearing loss and hearing aid use with cognition, health-related quality of life, and depressive symptoms. J Aging Health. 2023; 35(7-8):455–465. PMID: 36412130.7. Marques T, Marques FD, Miguéis A. Age-related hearing loss, depression and auditory amplification: a randomized clinical trial. Eur Arch Otorhinolaryngol. 2022; 279(3):1317–1321. PMID: 33860839.8. Naylor G, Dillard L, Orrell M, Stephan BC, Zobay O, Saunders GH. Dementia and hearing-aid use: a two-way street. Age Ageing. 2022; 51(12):afac266. PMID: 36571777.9. Weinstein BE, Sirow LW, Moser S. Relating hearing aid use to social and emotional loneliness in older adults. Am J Audiol. 2016; 25(1):54–61. PMID: 26999406.10. Zahl SM. Effects of receiving hearing aids on health-related quality of life in adults with mild hearing loss. J Audiol Otol. 2023; 27(1):24–29. PMID: 36710416.11. Bisgaard N, Zimmer S, Laureyns M, Groth J. A model for estimating hearing aid coverage world-wide using historical data on hearing aid sales. Int J Audiol. 2022; 61(10):841–849. PMID: 34428121.12. Grundfast KM, Liu SW. What otolaryngologists need to know about hearing aids. JAMA Otolaryngol Head Neck Surg. 2017; 143(2):109–110. PMID: 27893006.13. Powell W, Jacobs JA, Noble W, Bush ML, Snell-Rood C. Rural adult perspectives on impact of hearing loss and barriers to care. J Community Health. 2019; 44(4):668–674. PMID: 30949965.14. Valente M, Amlani AM. Cost as a barrier for hearing aid adoption. JAMA Otolaryngol Head Neck Surg. 2017; 143(7):647–648. PMID: 28520884.15. Brody L, Wu YH, Stangl E. A comparison of personal sound amplification products and hearing aids in ecologically relevant test environments. Am J Audiol. 2018; 27(4):581–593. PMID: 30458521.16. Cho YS, Park SY, Seol HY, Lim JH, Cho YS, Hong SH, et al. Clinical performance evaluation of a personal sound amplification product vs a basic hearing aid and a premium hearing aid. JAMA Otolaryngol Head Neck Surg. 2019; 145(6):516–522. PMID: 31095263.17. Choi JE, Kim J, Yoon SH, Hong SH, Moon IJ. A personal sound amplification product compared to a basic hearing aid for speech intelligibility in adults with mild-to-moderate sensorineural hearing loss. J Audiol Otol. 2020; 24(2):91–98. PMID: 31842534.18. Chen CH, Huang CY, Cheng HL, Lin HH, Chu YC, Chang CY, et al. Comparison of personal sound amplification products and conventional hearing aids for patients with hearing loss: a systematic review with meta-analysis. EClinicalMedicine. 2022; 46:101378. PMID: 35434580.19. Kim GY, Kim S, Jo M, Seol HY, Cho YS, Lim J, et al. Hearing and speech perception for people with hearing loss using personal sound amplification products. J Korean Med Sci. 2022; 37(12):e94. PMID: 35347902.20. Perron M, Lau B, Alain C. Interindividual variability in the benefits of personal sound amplification products on speech perception in noise: a randomized cross-over clinical trial. PLoS One. 2023; 18(7):e0288434. PMID: 37467243.21. Sheffield SW, Jacobs M, Ellis C Jr, Gerasimchik A. Comparing direct-to-consumer devices to hearing aids: amplification accuracy for three types of hearing loss. Am J Audiol. 2023.22. Reed NS, Betz J, Kendig N, Korczak M, Lin FR. Personal sound amplification products vs a conventional hearing aid for speech understanding in noise. JAMA. 2017; 318(1):89–90. PMID: 28672306.23. Bess FH, Tharpe AM, Gibler AM. Auditory performance of children with unilateral sensorineural hearing loss. Ear Hear. 1986; 7(1):20–26. PMID: 3949097.24. Douglas SA, Yeung P, Daudia A, Gatehouse S, O’Donoghue GM. Spatial hearing disability after acoustic neuroma removal. Laryngoscope. 2007; 117(9):1648–1651. PMID: 18062043.25. Dwyer NY, Firszt JB, Reeder RM. Effects of unilateral input and mode of hearing in the better ear: self-reported performance using the speech, spatial and qualities of hearing scale. Ear Hear. 2014; 35(1):126–136. PMID: 24084062.26. Firszt JB, Reeder RM, Holden LK. Unilateral hearing loss: understanding speech recognition and localization variability-implications for cochlear implant candidacy. Ear Hear. 2017; 38(2):159–173. PMID: 28067750.27. Golub JS, Lin FR, Lustig LR, Lalwani AK. Prevalence of adult unilateral hearing loss and hearing aid use in the United States. Laryngoscope. 2018; 128(7):1681–1686. PMID: 29193112.28. Suh MJ, Lee J, Cho WH, Jin IK, Kong TH, Oh SH, et al. Improving accuracy and reliability of hearing tests: an exploration of international standards. J Audiol Otol. 2023; 27(4):169–180. PMID: 37872752.29. Kim JS, Lim D, Hong HN, Shin HW, Lee KD, Hong BN, et al. Development of Korean standard monosyllabic word lists for adults (KS-MWL-A). Audiology. 2008; 4(2):126–140.30. Moon SK, Mun HA, Jung HK, Soli SD, Lee JH, Park K. Development of Sentences for Korean Hearing in Noise Test (KHINT). Korean J Otorhinolaryngol-Head Neck Surg. 2005; 48(6):724–728.31. Lim HJ, Park MK, Cho YS, Han GC, Choi JW, An YH, et al. Validation of the Korean version of the abbreviated profile of hearing aid benefit. Korean J Otorhinolaryngol-Head Neck Surg. 2017; 60(4):164–173.32. Kim JH, Lee SY, Kim CH, Lim SL, Shin JN, Chung WH, et al. Reliability and validity of a Korean adaptation of the Tinnitus Handicap Inventory. Korean J Otorhinolaryngol-Head Neck Surg. 2002; 45(4):328–334.33. Chu H, Cho YS, Park SN, Byun JY, Shin JE, Han GC, et al. Standardization for a Korean adaptation of the international outcome inventory for hearing aids: study of validity and reliability. Korean J Otorhinolaryngol-Head Neck Surg. 2012; 55(1):20–25.34. Kim GY, Kim JS, Jo M, Seol HY, Cho YS, Moon IJ. Feasibility of personal sound amplification products in patients with moderate hearing loss: a pilot study. Clin Exp Otorhinolaryngol. 2022; 15(1):60–68. PMID: 33541032.35. Venkitakrishnan S, Urbanski D, Wu YH. Efficacy and effectiveness of evidence-based non-self-fitting presets compared to prescription hearing aid fittings and a personal sound amplification product. Am J Audiol. 2023; 33(1):1–24.36. Han JS, Kim Y, Park MK, Song JJ, Moon IJ, Lee W, et al. Perception and expectations of personal sound amplification products in Korea: a hospital-based, multi-center, cross-sectional survey. PLoS One. 2022; 17(5):e0269123. PMID: 35617328.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Hearing Rehabilitation Experiences With Osia®2 Bone Conduction Hearing Implant in Patients With Iatrogenic Unilateral Hearing Loss
- Hearing and Speech Perception for People With Hearing Loss Using Personal Sound Amplification Products
- Rehabilitation of Sensorineural Hearing Loss: Hearing Aid
- Management of Hearing Aids Clinic
- The Effectiveness of the Hearing Aid in Hearing Loss with Tinnitus