Ann Pediatr Endocrinol Metab.
2024 Jun;29(3):191-200. 10.6065/apem.2346060.030.
Factors affecting bone mineral density in children and adolescents with systemic lupus erythematosus
- Affiliations
-
- 1Department of Pediatrics, College of Medicine, The Catholic University of Korea, Seoul, Korea
- KMID: 2556676
- DOI: http://doi.org/10.6065/apem.2346060.030
Abstract
- Purpose
Patients with juvenile-onset systemic lupus erythematosus (JSLE) are at a high risk of entering adulthood with disease-related morbidities like reduced bone mass and osteoporosis. This study aimed to evaluate the clinical characteristics of JSLE and to analyze the factors associated with low bone mineral density (BMD) in these patients.
Methods
Children and adolescents diagnosed with JSLE at a single institution in Korea were included. Demographic, clinical, and laboratory data as well as details about the use of glucocorticoids (GCs) and disease-modifying antirheumatic drugs were collected. The lumbar spine (LS) BMD z-score was measured using dual energy x-ray absorptiometry, and lateral thoracolumbar spine radiographs were collected.
Results
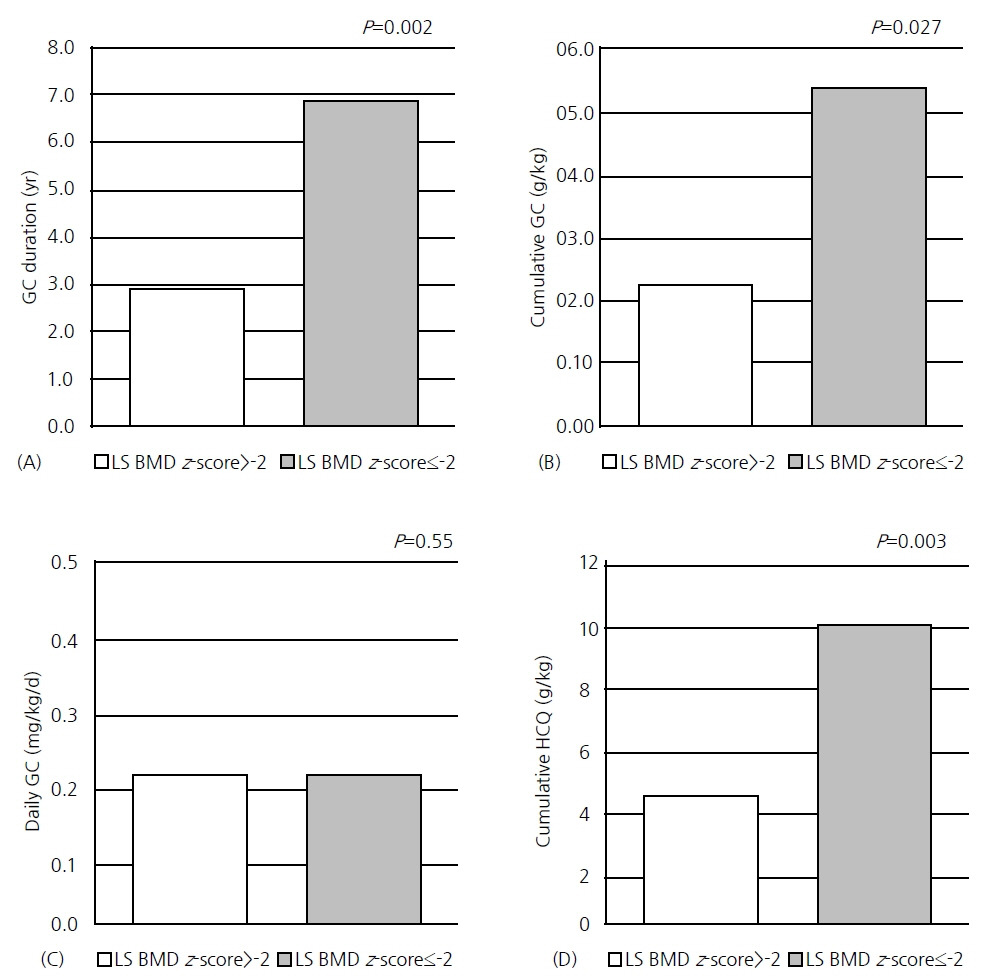
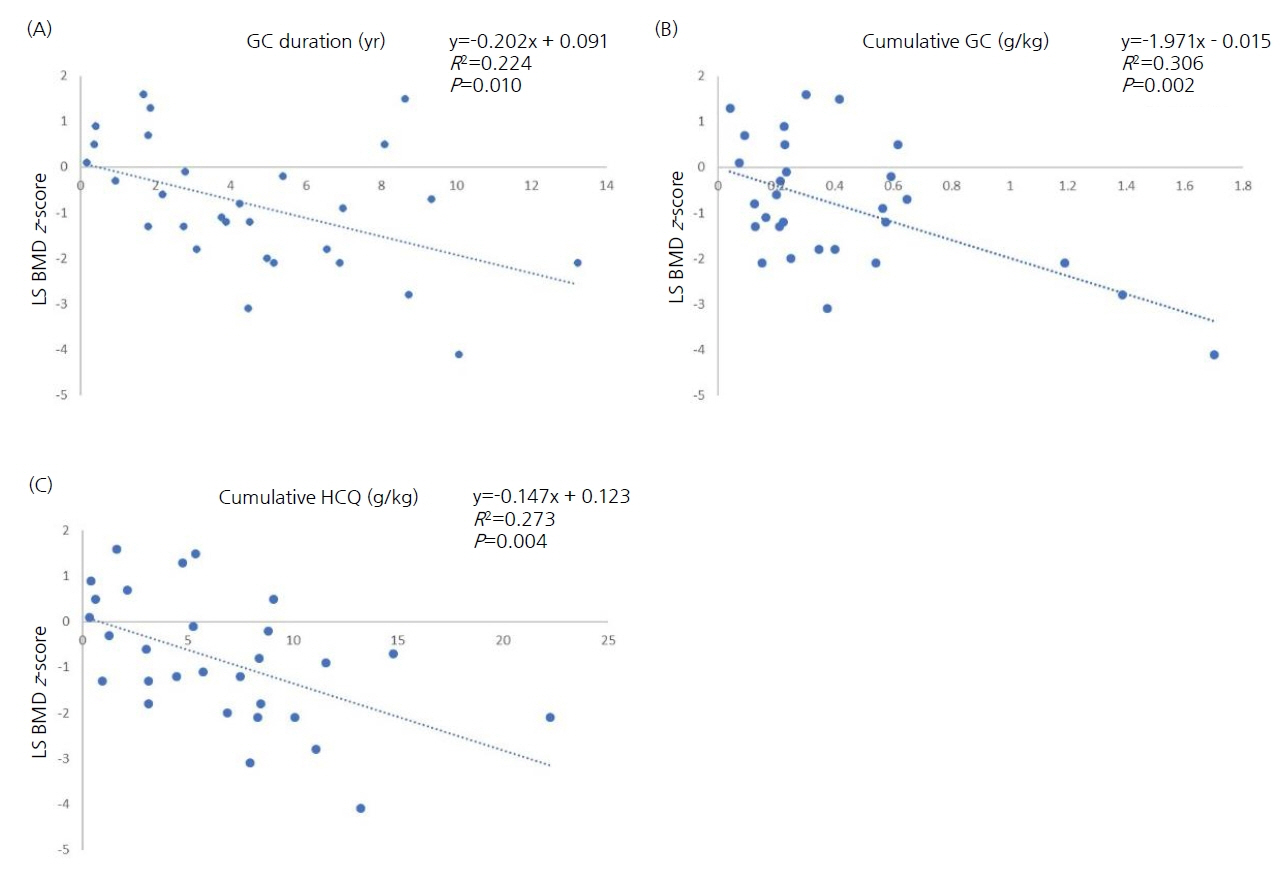
A total of 29 patients with JSLE were included in this study. Of these patients, 7 had a BMD z-score of -2.0 or lower and were designated as the low BMD group. The differences in the clinical parameters and treatment variables between the low BMD and non-low BMD groups were compared. Higher cumulative GC dose, longer GC exposure, and higher cumulative hydroxychloroquine (HCQ) dose were all associated with low BMD; among them, the main factor was the duration of GC exposure. There was no significant correlation between BMD and clinical profile, disease activity, or bone-metabolism markers.
Conclusion
The duration of GC exposure, cumulative GC dose, and cumulative HCQ dose were risk factors for low BMD in patients with JSLE, with the main factor being the duration of GC exposure. Thus, patients with JSLE should be routinely monitored for low BMD and potential fracture risks, and GC-sparing treatment regimens should be considered.
Keyword
Figure
Reference
-
References
1. Compeyrot-Lacassagne S, Tyrrell PN, Atenafu E, Doria AS, Stephens D, Gilday D, et al. Prevalence and etiology of low bone mineral density in juvenile systemic lupus erythematosus. Arthritis Rheum. 2007; 56:1966–73.
Article2. Stagi S, Rigante D. Vitamin D and juvenile systemic lupus erythematosus: lights, shadows and still unresolved issues. Autoimmun Rev. 2018; 17:290–300.
Article3. Phang KF, Cho J, Lee W, Mak A. Glucocorticoid-induced osteoporosis in systemic lupus erythematosus. Rheumatol Pract Res. 2018; 3:2059902118802510.
Article4. Lilleby V, Lien G, Frey Frøslie K, Haugen M, Flatø B, Førre Ø. Frequency of osteopenia in children and young adults with childhood-onset systemic lupus erythematosus. Arthritis Rheum. 2005; 52:2051–9.
Article5. Maggioli C, Stagi S. Bone modeling, remodeling, and skeletal health in children and adolescents: mineral accrual, assessment and treatment. Ann Pediatr Endocrinol Metab. 2017; 22:1–5.
Article6. Lee YA, Kwon A, Kim JH, Nam HK, Yoo JH, Lim JS, et al. Clinical practice guidelines for optimizing bone health in Korean children and adolescents. Ann Pediatr Endocrinol Metab. 2022; 27:5–14.
Article7. Bultink IEM. Bone disease in connective tissue disease/systemic lupus erythematosus. Calcif Tissue Int. 2018; 102:575–91.
Article8. Rizzoli R, Biver E. Glucocorticoid-induced osteoporosis: who to treat with what agent? Nat Rev Rheumatol. 2015; 11:98–109.
Article9. Mendoza-Pinto C, Rojas-Villarraga A, Molano-González N, Jiménez-Herrera EA, León-Vázquez ML, Montiel-Jarquín Á, et al. Bone mineral density and vertebral fractures in patients with systemic lupus erythematosus: a systematic review and meta-regression. PLoS One. 2018; 13:e0196113.
Article10. Jacobs J, Korswagen LA, Schilder AM, van Tuyl LH, Dijkmans BA, Lems WF, et al. Six-year follow-up study of bone mineral density in patients with systemic lupus erythematosus. Osteoporos Int. 2013; 24:1827–33.
Article11. Davidson JE, Fu Q, Rao S, Magder LS, Petri M. Quantifying the burden of steroid-related damage in SLE in the Hopkins Lupus Cohort. Lupus Sci Med. 2018; 5:e000237.12. Chen HL, Shen LJ, Hsu PN, Shen CY, Hall SA, Hsiao FY. Cumulative burden of glucocorticoid-related adverse events in patients with systemic lupus erythematosus: findings from a 12-year longitudinal study. J Rheumatol. 2018; 45:83–9.
Article13. Gu C, Zhao R, Zhang X, Gu Z, Zhou W, Wang Y, et al. A meta-analysis of secondary osteoporosis in systemic lupus erythematosus: prevalence and risk factors. Arch Osteoporos. 2019; 15:1.
Article14. Trapani S, Civinini R, Ermini M, Paci E, Falcini F. Osteoporosis in juvenile systemic lupus erythematosus: a longitudinal study on the effect of steroids on bone mineral density. Rheumatol Int. 1998; 18:45–9.
Article15. Nakhla M, Scuccimarri R, Duffy KN, Chédeville G, Campillo S, Duffy CM, et al. Prevalence of vertebral fractures in children with chronic rheumatic diseases at risk for osteopenia. J Pediatr. 2009; 154:438–43.
Article16. Burnham JM, Shults J, Weinstein R, Lewis JD, Leonard MB. Childhood onset arthritis is associated with an increased risk of fracture: a population based study using the General Practice Research Database. Ann Rheum Dis. 2006; 65:1074–9.
Article17. Valta H, Lahdenne P, Jalanko H, Aalto K, Mäkitie O. Bone health and growth in glucocorticoid-treated patients with juvenile idiopathic arthritis. J Rheumatol. 2007; 34:831–6.18. Ward LM, Ma J, Robinson ME, Scharke M, Ho J, Houghton K, et al. Osteoporotic fractures and vertebral body reshaping in children with glucocorticoid-treated rheumatic disorders. J Clin Endocrinol Metab. 2021; 106:e5195. –207.
Article19. Hochberg MC. Updating the American College of Rheumatology revised criteria for the classification of systemic lupus erythematosus. Arthritis Rheum. 1997; 40:1725.
Article20. Aringer M, Costenbader K, Daikh D, Brinks R, Mosca M, Ramsey-Goldman R, et al. 2019 European League Against Rheumatism/American College of Rheumatology classification criteria for systemic lupus erythematosus. Ann Rheum Dis. 2019; 78:1151–9.21. Petri M, Orbai AM, Alarcón GS, Gordon C, Merrill JT, Fortin PR, et al. Derivation and validation of the Systemic Lupus International Collaborating Clinics classification criteria for systemic lupus erythematosus. Arthritis Rheum. 2012; 64:2677–86.22. Silva CA, Avcin T, Brunner HI. Taxonomy for systemic lupus erythematosus with onset before adulthood. Arthritis Care Res (Hoboken). 2012; 64:1787–93.
Article23. The American College of Rheumatology nomenclature and case definitions for neuropsychiatric lupus syndromes. Arthritis Rheum. 1999; 42:599–608.24. Gladman DD, Ibañez D, Urowitz MB. Systemic lupus erythematosus disease activity index 2000. J Rheumatol. 2002; 29:288–91.25. Thanou A, Jupe E, Purushothaman M, Niewold TB, Munroe ME. Clinical disease activity and flare in SLE: Current concepts and novel biomarkers. J Autoimmun. 2021; 119:102615.
Article26. Yi KH, Hwang JS, Kim EY, Lee JA, Kim DH, Lim JS. Reference values for bone mineral density according to age with body size adjustment in Korean children and adolescents. J Bone Miner Metab. 2014; 32:281–9.
Article27. Genant HK, Wu CY, van Kuijk C, Nevitt MC. Vertebral fracture assessment using a semiquantitative technique. J Bone Miner Res. 1993; 8:1137–48.
Article28. Fanouriakis A, Kostopoulou M, Alunno A, Aringer M, Bajema I, Boletis JN, et al. 2019 update of the EULAR recommendations for the management of systemic lupus erythematosus. Ann Rheum Dis. 2019; 78:736–45.
Article29. LeBlanc CM, Ma J, Taljaard M, Roth J, Scuccimarri R, Miettunen P, et al. Incident vertebral fractures and risk factors in the first three years following glucocorticoid initiation among pediatric patients with rheumatic disorders. J Bone Miner Res. 2015; 30:1667–75.
Article30. Costedoat-Chalumeau N, Amoura Z, Hulot JS, Hammoud HA, Aymard G, Cacoub P, et al. Low blood concentration of hydroxychloroquine is a marker for and predictor of disease exacerbations in patients with systemic lupus erythematosus. Arthritis Rheum. 2006; 54:3284–90.
Article31. Mok CC, Mak A, Ma KM. Bone mineral density in postmenopausal Chinese patients with systemic lupus erythematosus. Lupus. 2005; 14:106–12.
Article32. Lakshminarayanan S, Walsh S, Mohanraj M, Rothfield N. Factors associated with low bone mineral density in female patients with systemic lupus erythematosus. J Rheumatol. 2001; 28:102–8.33. Cramarossa G, Urowitz MB, Su J, Gladman D, Touma Z. Prevalence and associated factors of low bone mass in adults with systemic lupus erythematosus. Lupus. 2017; 26:365–72.
Article34. Hauser B, Raterman H, Ralston SH, Lems WF. The Effect of anti-rheumatic drugs on the skeleton. Calcif Tissue Int. 2022; 111:445–56.
Article35. Ahn MB, Suh BK. Bone morbidity in pediatric acute lymphoblastic leukemia. Ann Pediatr Endocrinol Metab. 2020; 25:1–9.
Article36. Cranney AB, McKendry RJ, Wells GA, Ooi DS, Kanigsberg ND, Kraag GR, et al. The effect of low dose methotrexate on bone density. J Rheumatol. 2001; 28:2395–9.37. Florén CH, Ahrén B, Bengtsson M, Bartosik J, Obrant K. Bone mineral density in patients with Crohn's disease during long-term treatment with azathioprine. J Intern Med. 1998; 243:123–6.
Article38. Zhu TY, Griffith JF, Au SK, Tang XL, Kwok AW, Leung PC, et al. Bone mineral density change in systemic lupus erythematosus: a 5-year followup study. J Rheumatol. 2014; 41:1990–7.
Article39. Naka H, Iki M, Morita A, Ikeda Y. Effects of pubertal development, height, weight, and grip strength on the bone mineral density of the lumbar spine and hip in peripubertal Japanese children: Kyoto kids increase density in the skeleton study (Kyoto KIDS study). J Bone Miner Metab. 2005; 23:463–9.
Article40. Masip E, Donat E, Polo Miquel B, Ribes-Koninckx C. Bone mineral density in Spanish children at the diagnosis of inflammatory bowel disease. Arch Osteoporos. 2021; 16:96.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Case of Transverse Myelitis as a First Manifestation of Systemic Lupus Erythematosus
- A Case Of Systemic Lupus Erythematosus Associated With Hyperthyroidism And Severe Retinopathy
- A Case of Lupus Enteritis That Developed during the Treatment of Systemic Lupus Erythematosus
- Multiple Dermatofibromas in a woman with Systemic Lupus Erythematosus
- A Ruptured Aneurysm in a Patient with Systemic Lupus Erythematosus: Case Report