J Korean Acad Oral Health.
2024 Jun;48(2):33-39. 10.11149/jkaoh.2024.48.2.33.
Usefulness of the odontogenic ameloblast-associated protein and quantitative analysis of periodontal disease-associated bacteria as biomarkers for evaluation of improvement in periodontal status following scaling intervention
- Affiliations
-
- 1Department of Dental Hygiene, Namseoul University, Cheonan, Korea
- 2Regenerative Dental Medicine R&D Center, HysensBio Co., Ltd., Gwacheon, Korea
- KMID: 2556592
- DOI: http://doi.org/10.11149/jkaoh.2024.48.2.33
Abstract
Objectives
In this study, we investigated the validity and effectiveness of biomarkers and oral microbiome analysis for evaluation of periodontal status following scaling intervention.
Methods
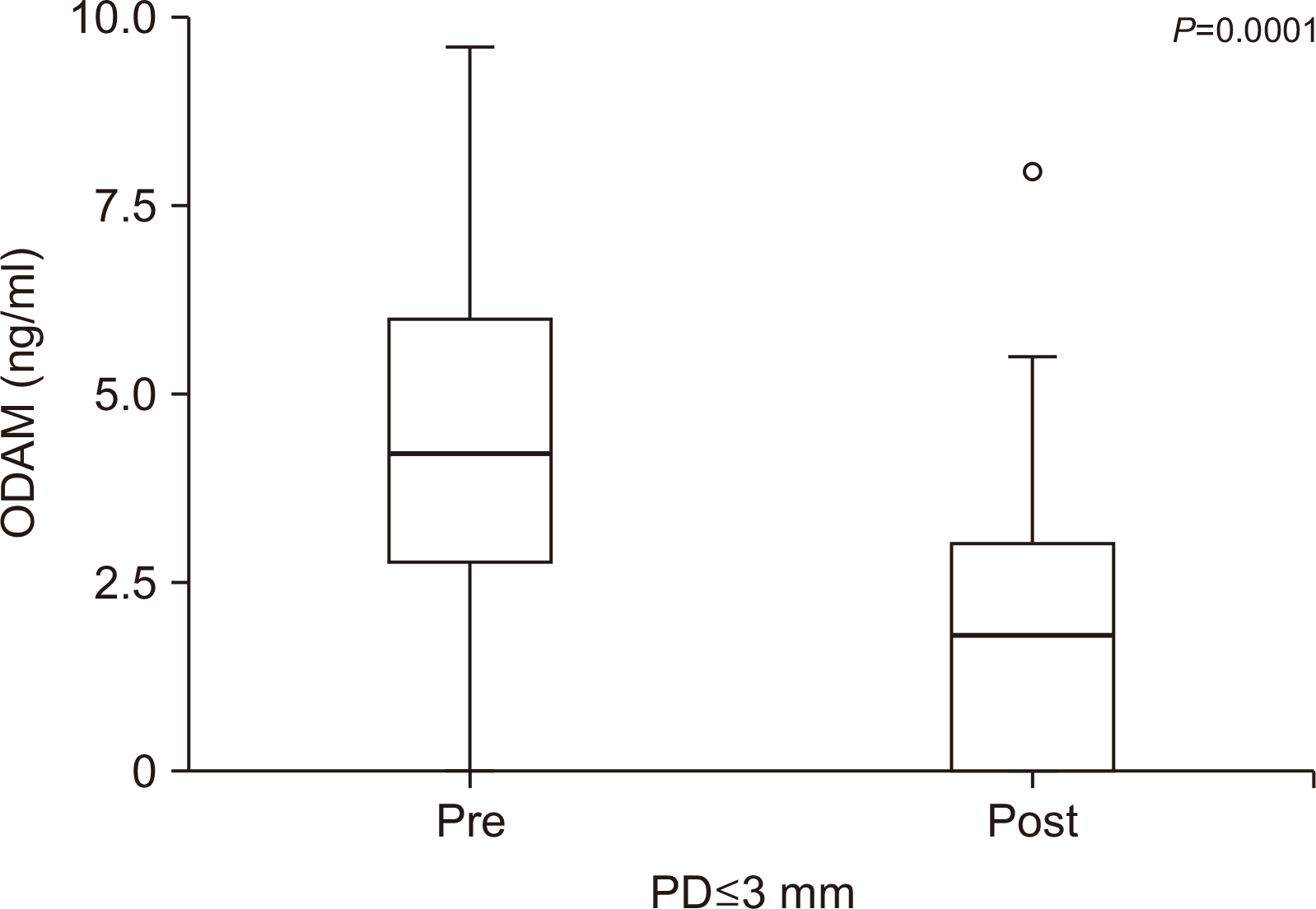
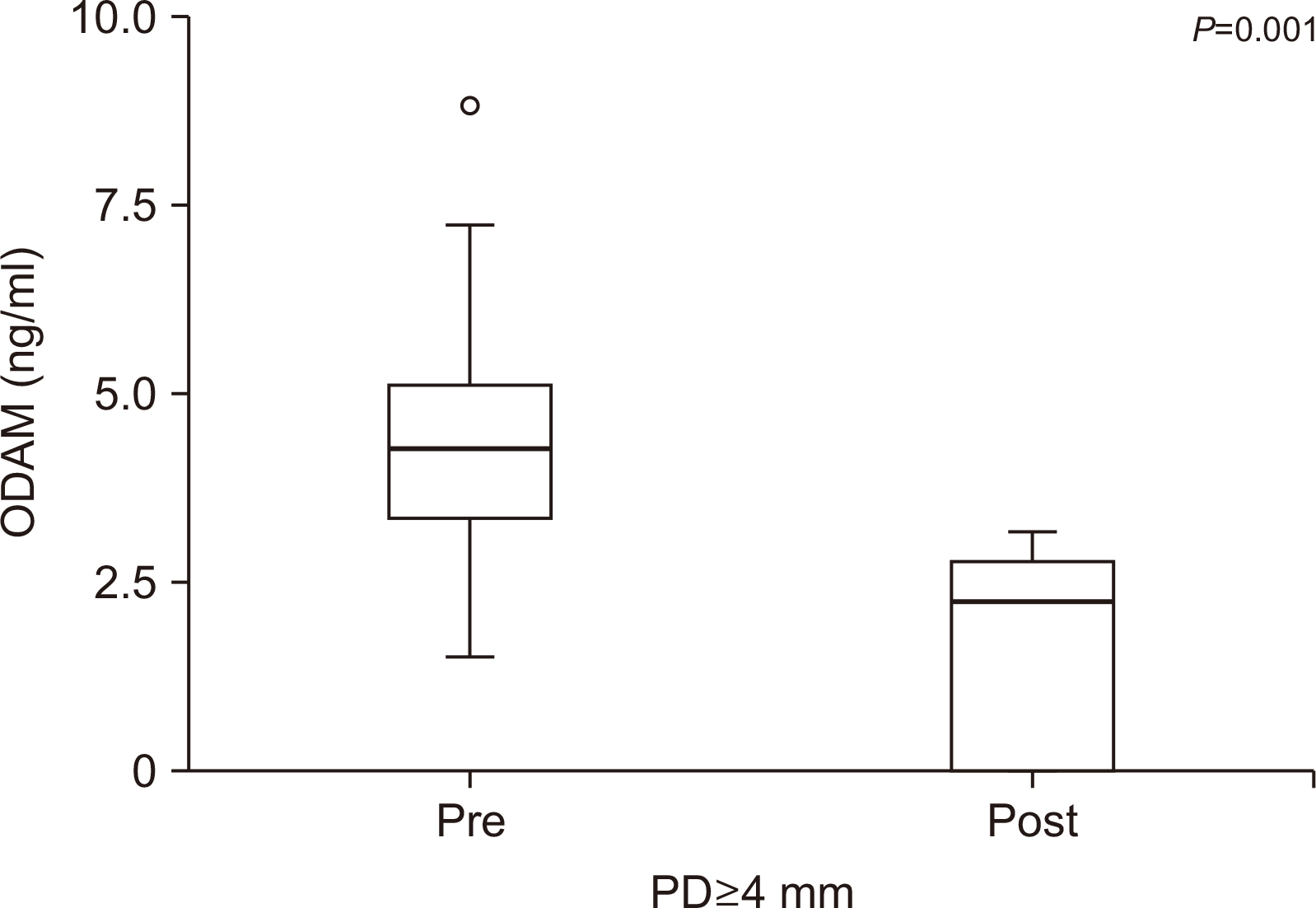
The study included 15 participants who were selected based on inclusion/exclusion criteria. Periodontal indices, including the plaque index, probing depth, modified sulcus bleeding index, and calculus index were measured to evaluate clinical periodontal status and disease progression. Pre- and post-scaling gingival crevicular fluid (GCF) was obtained from 12-20 sites per patient to measure changes in the odontogenic ameloblast-associated protein (ODAM) concentration using an enzyme-linked immunosorbent assay. Additionally, pre- and post-treatment salivary samples were obtained for quantitative analysis of oral microbiome distribution.
Results
All clinical parameters showed significant differences in pre- and post-scaling values and significant changes in the ODAM concentration in the GCF in patients with initial and moderate periodontitis. Quantitative analysis performed after scaling intervention revealed changes in eight oral disease-causing bacteria associated with periodontal disease, including Aggregatibacter, Porphyromonas, Tannerella, Treponema, Prevotella, and Fusobacterium. Specifically, Tannerella forsythia and Fusobacterium nucleatum (well-known major periodontal pathogens) numbers were significantly decreased following non-surgical periodontal therapy. However, no significant association was observed between changes in the salivary oral microbiota and ODAM concentration in the GCF, following treatment.
Conclusions
Based on the findings of this study, we propose the use of ODAM protein and quantitative analysis of periodontal disease-associated bacteria as objective and quantitative biomarkers for evaluation of improvement in periodontal disease following scaling intervention.
Figure
Reference
-
References
1. Bostanci N, Bao K, Greenwood D, Silbereisen A, Belibasakis G. N. 2019; Periodontal disease: from the lenses of light microcopy to the specs of proteomics and next-generation sequencing. Adv Clin Chem. 93:263–290. DOI: 10.1016/bs.acc.2019.07.006. PMID: 31655732.2. Enhos S, Duran I, Erdem S, Buyukbas S. 2009; Relationship between iron-deficiency anemia and periodontal status in female patients. J Periodontol. 80:1750–1755. DOI: 10.1902/jop.2009.090209. PMID: 19905931.3. Malhotra R, Kapoor A, Grover V, Grover D, Kaur A. 2012; Effect of scaling and root planing on erythrocyte count, hemoglobin and hematocrit in patients with chronic periodonta disease. J Dent Hyg. 86:195–203.4. Cheon SY, Won BY. 2011; Affecting factors to oral scaling experience of the part worker. J Korean Soc Dent Hyg. 11:1–12.5. Go EJ. 2020; Elderly's perception and experience of tartar removal and obstacles to periodontal management behavior. J Korean Oral Health Sci. 8:82–89. DOI: 10.33615/jkohs.2020.8.3.82.6. Lee KH, Son JY, Lee HO, Shin SH, Jeon HJ, You HJ, et al. 2017; Factors affecting the recognition about scaling after health insurance benefit business for scaling by national health insurance corporation. J Korean Soc Dent Hyg. 17:355–368. DOI: 10.13065/jksdh.2017.17.03.355.7. Kwon SJ, Choi YJ. 2010; Impact of the type of dental treatment on the dental fear of adolescents in south gyeongsang province. Kor Cont Assoc. 10:277–285. DOI: 10.5392/JKCA.2010.10.2.277.8. Kim JW, Cha IH, Kim SJ, Kim MR. 2016; Biomarkers for Bisphosphonate-related osteonecrosis of the jaw. Clin Implant Dent Relat Res. 18:281–291. DOI: 10.1111/cid.12297. PMID: 25726720.9. Han SK, Kong JH, Kim SG, Lee JH, Han DH. 2019; Exomic and transcriptomic alterations of hereditary gingival fibromatosis. Oral Dis. 25:1374–1383. DOI: 10.1111/odi.13093. PMID: 30907493.10. Kim HD, Lee CS, Cho HJ, Jeon S, Choi YN, Kim S, et al. 2020; Diagnostic ability of salivary matrix metalloproteinase-9 lateral flow test point-of-care test for periodontitis. J Clin Periodontol. 47:1354–1361. DOI: 10.1111/jcpe.13360. PMID: 32841379.11. Lee HK, Kim SJ, Kim YH, Ko Y, Ji S, Park JC. 2018; Odontogenic ameloblast-associated protein (ODAM) in gingival crevicular fluid for site-specific diagnostic value of periodontitis: a pilot study. BMC oral health. 18:148. DOI: 10.1186/s12903-018-0609-0. PMID: 30143043. PMCID: PMC6109327.12. Bhattarai KR, Kim HR, Chae HJ. 2018; Compliance with saliva collection protocol in healthy volunteers: strategeis for managing risk and errors. Int J Med Sci. 15:823–831. DOI: 10.7150/ijms.25146. PMID: 30008593. PMCID: PMC6036086.13. Li X, Liu Y, Yang X, Li C, Song Z. 2022; The oral microbiota: community composition, influencing factors, pathogenesis, and interventions. Front Microbiol. 13:895537. DOI: 10.3389/fmicb.2022.895537. PMID: 35572634. PMCID: PMC9100676.14. Al-Zyoud W, Hajjo R, Abu-Siniyeh A, Hajjaj S. 2019; Salivary microbiome and cigarette smoking: a first of its kind investigation in Jordan. Int J Environ Res Public Health. 17:256. DOI: 10.3390/ijerph17010256. PMID: 31905907. PMCID: PMC6982339.15. Stahringer SS, Clemente JC, Corley RP, Hewitt J, Knights D, Walters W, et al. 2012; Nurture trumps nature in a longitudinal survey of salivary bacterial communities in twins from early adolescence to early adulthood. Genome Res. 22:2146–2152. DOI: 10.1101/gr.140608.112. PMID: 23064750. PMCID: PMC3483544.16. Willis JR, Gabaldon T. 2020; The human oral microbiome in health and disease: from sequences to ecosystmes. Microorg. 8:308. DOI: 10.3390/microorganisms8020308. PMID: 32102216. PMCID: PMC7074908.17. Song KH. 2008; A study on the evaluation of health-and oral health-related quality of life in Korean adults. J Korean Acad Dent Hyg. 10:39–57.18. Kang BW, Kang HK, Gu IY, Kwon HM, Kim KS, Kim SS, et al. 2012. Preventive Dentistry. 4th ed. Koonja;Seoul: p. 22–46.19. Seo SY. 2009. The effects of periodontal patients' oral health perception and degree of practice of oral health on quality of life [master's thesis]. Dankook University;Yongin: [Korean].20. Yoon MM. 2014. A study on knowledge and perception of dental scaling of adult [master's thesis]. Hanyang University;Seoul: [Korean].21. Ha MY. 2015. A study on the changes in consumers' awareness and the rate of scaling in each region after its coverage by the national health insurance scheme [master's thesis]. Dankook University;Seoul: [Korean].22. Paster BJ, Olsen I, Aas JA, Dewhirs FE. 2006; The breadth of bacterial diversity in the human periodontal pocket and other oral sites. Periodontology 2000. 42:80–87. DOI: 10.1111/j.1600-0757.2006.00174.x. PMID: 16930307.23. Socransky SS, Haffajee AD. 2005; Periodontal microbial ecology. Periodontol 2000. 38:135–187. DOI: 10.1111/j.1600-0757.2005.00107.x. PMID: 15853940.24. Lee HK, Ji S, Park SJ, Choung HW, Choi Y, Lee HJ, et al. 2015; Odontogenic ameloblast-associated protein (ODAM) mediates junctional epithelium attachment teeth via integrin-ODAM-Rho Guanine Nucleotide Exchange Factor 5 (ARHGEF5)-RhoA signaling. J Biol Chem. 290:14740–14753. DOI: 10.1074/jbc.M115.648022. PMID: 25911094. PMCID: PMC4505539.25. Hwang GB, Park YH, Seo YM, Bae HS, Ji S, Park JC. 2021; Differential localization of ODAM in periodontitis with similar clinical severities. Korean J Oral Anatomy. 42:37–46.26. Socransky S, Haffajee CS, Dibart S. 1991; Relation of counts of microbial species to clinical status at the sampled site. J Clin Periodontol. 18:766–775. DOI: 10.1111/j.1600-051X.1991.tb00070.x. PMID: 1661305.27. Kumar PS, Griffen AL, Moeschberger ML, Leys EJ. 2005; Identification of candidate periodontal pathogens and beneficial species by quantitative 16S clonal analysis. J Clin Microbiol. 43:3944–3955. DOI: 10.1128/JCM.43.8.3944-3955.2005. PMID: 16081935. PMCID: PMC1233920.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Effects of Periodontal Disease Knowledge and Awareness of Scaling on Scaling Fear in Adults
- The clinical and microbiological effects of non-surgical periodontal treatments in necrotizing periodontal disease: case report
- Analysis of Periodontitis Biomarker Expression in Gingival Crevicular Fluids
- Periodontitis and Periodontal treatment of Hansen's Patients in National Sorokdo Hospital (Case Report)
- The Clinical and Microbiological Study of the Effect of Minocycline Strip Locally Administrated on Adult Periodontitis