J Stroke.
2024 May;26(2):339-341. 10.5853/jos.2023.03909.
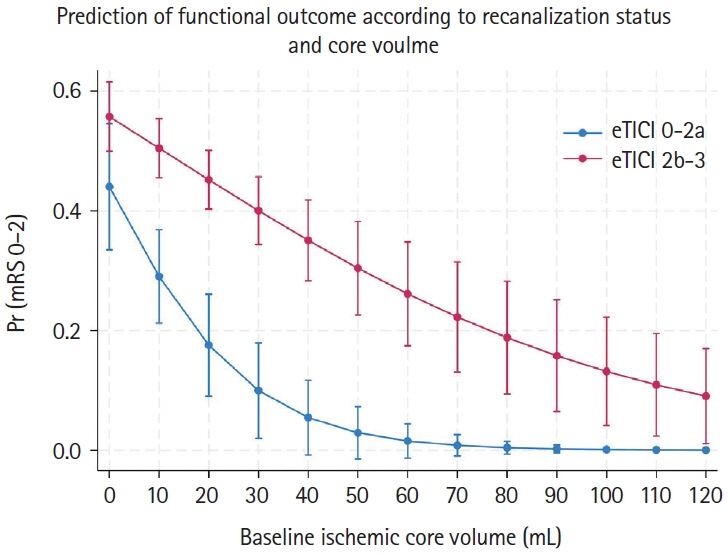
Discrepancy Between Ischemic Changes Observed on Non-Enhanced Computed Tomography and Perfusion Imaging: Implications for Decision-Making in Treatment
- Affiliations
-
- 1Department of Diagnostic and Interventional Neuroradiology, University Medical Center Hamburg-Eppendorf, Hamburg, Germany
- 2Department of Neuroradiology, HELIOS Medical Center, Campus of MSH Medical School Hamburg, Schwerin, Germany
- KMID: 2556056
- DOI: http://doi.org/10.5853/jos.2023.03909
Figure
Reference
-
References
1. Bendszus M, Fiehler J, Subtil F, Bonekamp S, Aamodt AH, Fuentes B, et al. Endovascular thrombectomy for acute ischaemic stroke with established large infarct: multicentre, openlabel, randomised trial. Lancet. 2023; 402:1753–1763.2. Sarraj A, Hassan AE, Abraham MG, Ortega-Gutierrez S, Kasner SE, Hussain MS, et al. Trial of endovascular thrombectomy for large ischemic strokes. N Engl J Med. 2023; 388:1259–1271.
Article3. Jadhav AP, Hacke W, Dippel DWJ, Simonsen CZ, Costalat V, Fiehler J, et al. Select wisely: the ethical challenge of defining large core with perfusion in the early time window. J Neurointerv Surg. 2021; 13:497–499.
Article4. Sarraj A, Hassan AE, Savitz S, Sitton C, Grotta J, Chen P, et al. Outcomes of endovascular thrombectomy vs medical management alone in patients with large ischemic cores: a secondary analysis of the optimizing patient’s selection for endovascular treatment in acute ischemic stroke (SELECT) study. JAMA Neurol. 2019; 76:1147–1156.
Article5. McDonough R, Elsayed S, Meyer L, Ewers T, Bechstein M, Kniep H, et al. Low baseline ischemic water uptake is directly related to overestimation of CT perfusion-derived ischemic core volume. Sci Rep. 2022; 12:20567.6. Goyal M, Ospel JM, Menon B, Almekhlafi M, Jayaraman M, Fiehler J, et al. Challenging the ischemic core concept in acute ischemic stroke imaging. Stroke. 2020; 51:3147–3155.
Article7. Broocks G, Rajput F, Hanning U, Faizy TD, Leischner H, Schön G, et al. Highest lesion growth rates in patients with hyperacute stroke: when time is brain particularly matters. Stroke. 2019; 50:189–192.
Article8. Stösser S, Bode FJ, Meissner JN, Weller JM, Kindler C, Sauer M, et al. Outcome of stroke patients with unknown onset and unknown time last known well undergoing endovascular therapy. Clin Neuroradiol. 2023; 33:107–112.
Article9. Haupt W, Meyer L, Wagner M, McDonough R, Elsayed S, Bechstein M, et al. Assessment of irreversible tissue injury in extensive ischemic stroke—potential of quantitative cerebral perfusion. Transl Stroke Res. 2023; 14:562–571.
Article10. Broocks G, McDonough R, Meyer L, Bechstein M, Kniep H, Schön G, et al. Reversible ischemic lesion hypodensity in acute stroke CT following endovascular reperfusion. Neurology. 2021; 97:e1075–e1084.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Induced Hypertensive Therapy in an Acute Ischemic Stroke Patient with Early Neurological Deterioration
- Recent development of diagnostic imaging of hepatocellular carcinoma
- The Usefulness of Perfusion CT in Acute Cerebral Ischemic Infarction
- Discrepancy in core infarct betweennon-contrast CT and CT perfusionwhen selecting for mechanicalthrombectomy
- Clinical Application of Acute Ischemic Stroke in Perfusion Computed Tomography