J Stroke.
2024 May;26(2):190-202. 10.5853/jos.2023.02649.
Distal Medium Vessel Occlusion Strokes: Understanding the Present and Paving the Way for a Better Future
- Affiliations
-
- 1UPMC Stroke Institute, Department of Neurology, University of Pittsburgh School of Medicine, Pittsburgh, PA, USA
- 2Department of Neurology, Ajou University Medical Center, Ajou University School of Medicine, Suwon, Korea
- 3Department of Neurology, Marcus Stroke and Neuroscience Center, Grady Memorial Hospital, Emory University School of Medicine, Atlanta, GA, USA
- 4UPMC Stroke Institute, Department of Neurosurgery, University of Pittsburgh School of Medicine, Pittsburgh, PA, USA
- 5Department of Neuroradiology, Centro Hospitalar Universitário Lisboa Central, Lisboa, Portugal
- KMID: 2556041
- DOI: http://doi.org/10.5853/jos.2023.02649
Abstract
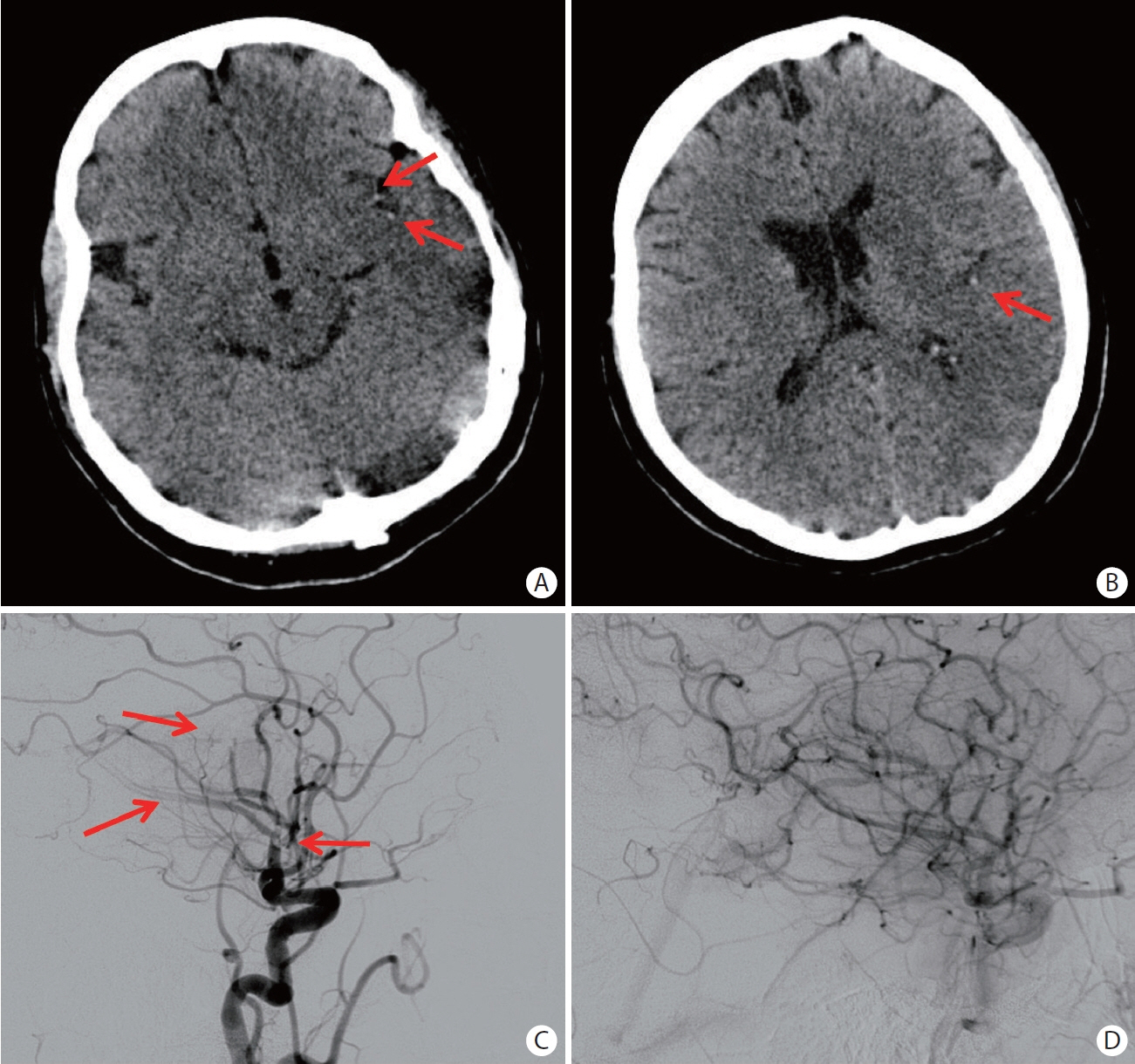
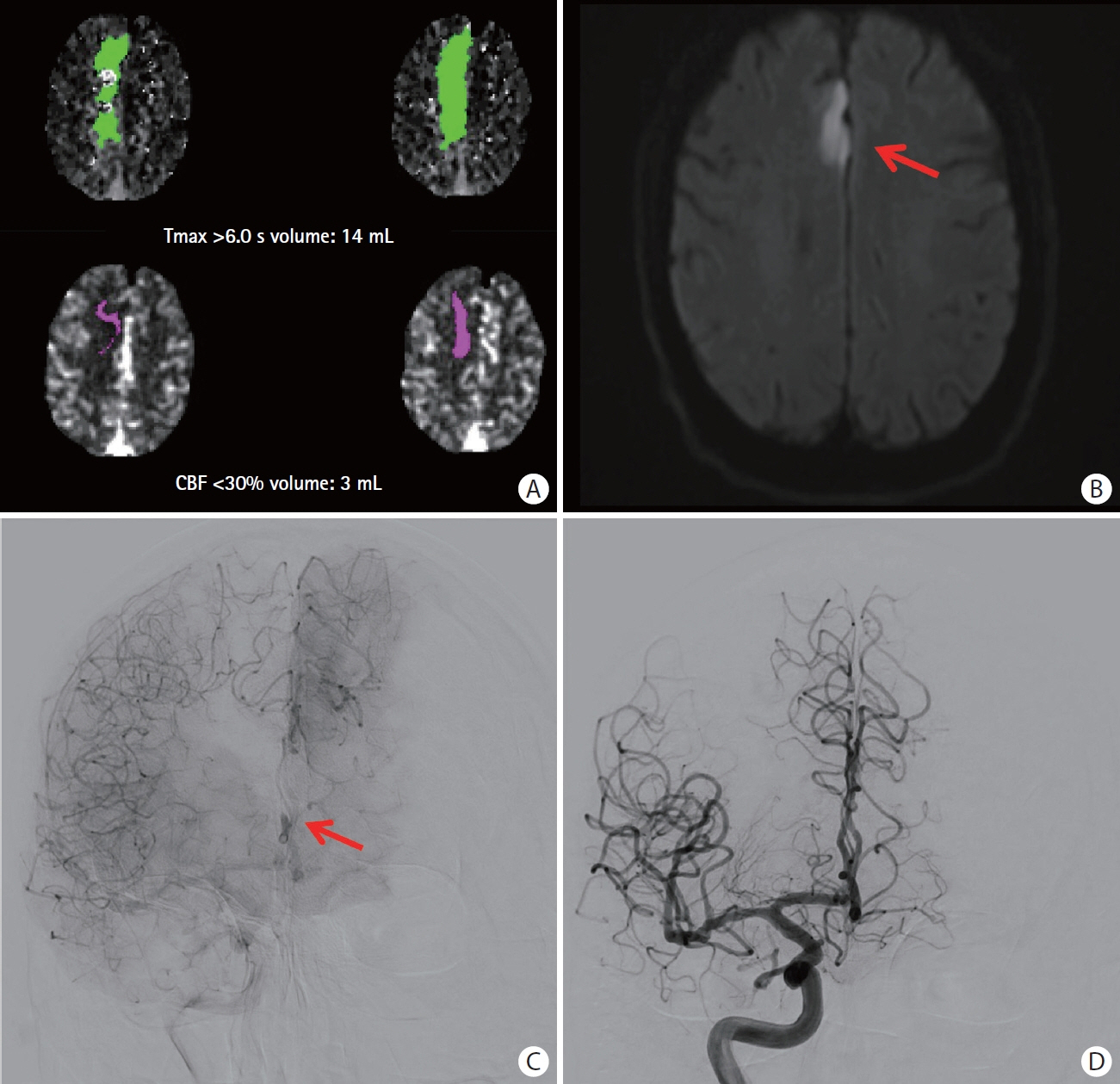
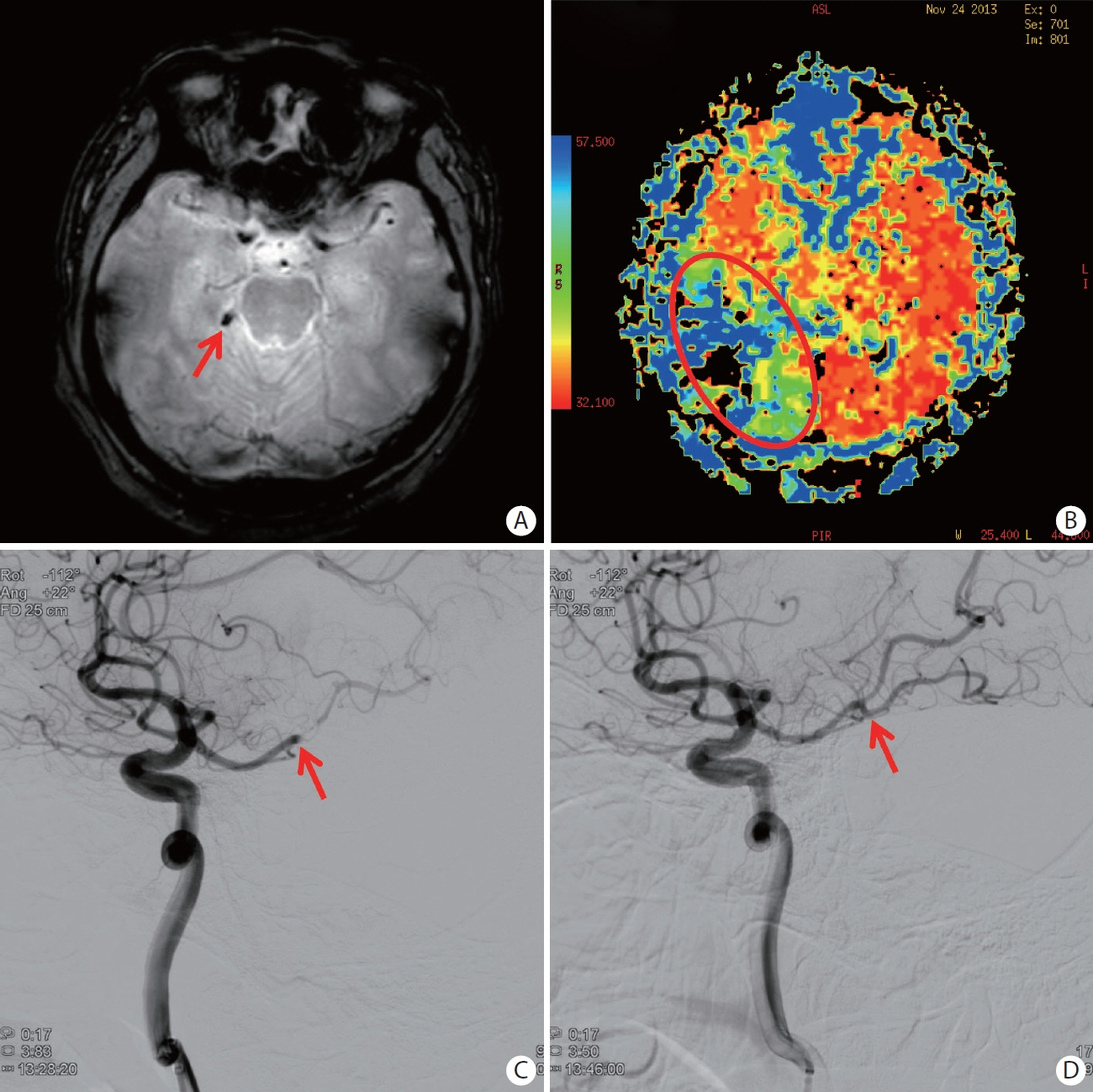
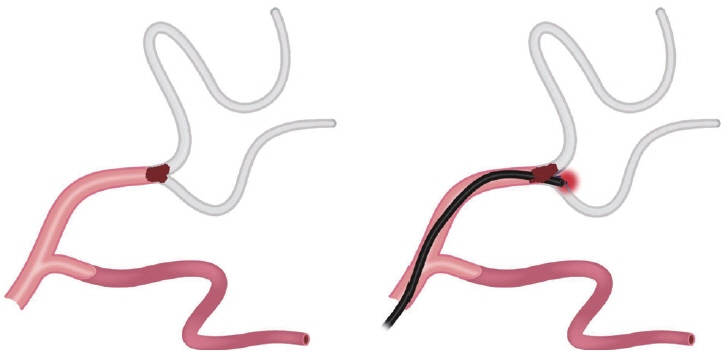
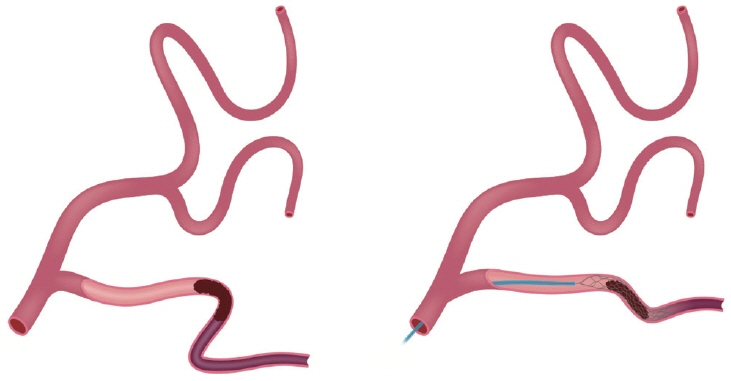
- Distal medium vessel occlusions (DMVOs) are thought to cause as many as 25% to 40% of all acute ischemic strokes and may result in substantial disability amongst survivors. Although intravenous thrombolysis (IVT) is more effective for distal than proximal vessel occlusions, the overall efficacy of IVT remains limited in DMVO with less than 50% of patients achieving reperfusion and about 1/3 to 1/4 of the patients failing to achieve functional independence. Data regarding mechanical thrombectomy (MT) among these patients remains limited. The smaller, thinner, and more tortuous vessels involved in DMVO are presumably associated with higher procedural risks whereas a lower benefit might be expected given the smaller amount of tissue territory at risk. Recent advances in technology have shown promising results in endovascular treatment of DMVOs with room for future improvement. In this review, we discuss some of the key technical and clinical considerations in DMVO treatment including the anatomical and clinical terminology, diagnostic modalities, the role of IVT and MT, existing technology, and technical challenges as well as the contemporary evidence and future treatment directions.
Figure
Reference
-
References
1. Ospel JM, Goyal M. A review of endovascular treatment for medium vessel occlusion stroke. J Neurointerv Surg. 2021; 13:623–630.
Article2. Saver JL, Chapot R, Agid R, Hassan A, Jadhav AP, Liebeskind DS, et al. Thrombectomy for distal, medium vessel occlusions: a consensus statement on present knowledge and promising directions. Stroke. 2020; 51:2872–2884.3. Powers WJ, Rabinstein AA, Ackerson T, Adeoye OM, Bambakidis NC, Becker K, et al. Guidelines for the early management of patients with acute ischemic stroke: 2019 update to the 2018 guidelines for the early management of acute ischemic stroke: a guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2019; 50:e344–e418.
Article4. Turc G, Bhogal P, Fischer U, Khatri P, Lobotesis K, Mazighi M, et al. European Stroke Organisation (ESO) - European Society for Minimally Invasive Neurological Therapy (ESMINT) guidelines on mechanical thrombectomy in acute ischaemic strokeendorsed by Stroke Alliance for Europe (SAFE). Eur Stroke J. 2019; 4:6–12.
Article5. Ospel JM, Menon BK, Demchuk AM, Almekhlafi MA, Kashani N, Mayank A, et al. Clinical course of acute ischemic stroke due to medium vessel occlusion with and without intravenous alteplase treatment. Stroke. 2020; 51:3232–3240.
Article6. Campbell BCV, Ma H, Ringleb PA, Parsons MW, Churilov L, Bendszus M, et al. Extending thrombolysis to 4·5–9 h and wake-up stroke using perfusion imaging: a systematic review and meta-analysis of individual patient data. Lancet. 2019; 394:139–147.7. Goyal M, Menon BK, van Zwam WH, Dippel DW, Mitchell PJ, Demchuk AM, et al. Endovascular thrombectomy after large-vessel ischaemic stroke: a meta-analysis of individual patient data from five randomised trials. Lancet. 2016; 387:1723–1731.8. Menon BK, Hill MD, Davalos A, Roos YBWEM, Campbell BCV, Dippel DWJ, et al. Efficacy of endovascular thrombectomy in patients with M2 segment middle cerebral artery occlusions: meta-analysis of data from the HERMES collaboration. J Neurointerv Surg. 2019; 11:1065–1069.
Article9. Grossberg JA, Rebello LC, Haussen DC, Bouslama M, Bowen M, Barreira CM, et al. Beyond large vessel occlusion strokes: distal occlusion thrombectomy. Stroke. 2018; 49:1662–1668.10. Haussen DC, Al-Bayati AR, Eby B, Ravindran K, Rodrigues GM, Frankel MR, et al. Blind exchange with mini-pinning technique for distal occlusion thrombectomy. J Neurointerv Surg. 2020; 12:392–395.
Article11. Haussen DC, Lima A, Nogueira RG. The Trevo XP 3×20 mm retriever (‘Baby Trevo’) for the treatment of distal intracranial occlusions. J Neurointerv Surg. 2016; 8:295–299.12. Nogueira RG, Mohammaden MH, Haussen DC, Budzik RF, Gupta R, Krajina A, et al. Endovascular therapy in the distal neurovascular territory: results of a large prospective registry. J Neurointerv Surg. 2021; 13:979–984.13. Pérez-García C, Moreu M, Rosati S, Simal P, Egido JA, GomezEscalonilla C, et al. Mechanical thrombectomy in medium vessel occlusions: blind exchange with mini-pinning technique versus mini stent retriever alone. Stroke. 2020; 51:3224–3231.
Article14. Goyal M, Ospel JM, Menon BK, Hill MD. MeVO: the next frontier? J Neurointerv Surg. 2020; 12:545–547.
Article15. Leary MC, Kidwell CS, Villablanca JP, Starkman S, Jahan R, Duckwiler GR, et al. Validation of computed tomographic middle cerebral artery “dot” sign: an angiographic correlation study. Stroke. 2003; 34:2636–2640.
Article16. Park MG, Oh SJ, Baik SK, Jung DS, Park KP. Susceptibility-weighted imaging for detection of thrombus in acute cardioembolic stroke. J Stroke. 2016; 18:73–79.
Article17. Kunz WG, Sommer WH, Havla L, Dorn F, Meinel FG, Dietrich O, et al. Detection of single-phase CTA occult vessel occlusions in acute ischemic stroke using CT perfusion-based wavelettransformed angiography. Eur Radiol. 2017; 27:2657–2664.
Article18. Mattern H, Sciarra A, Godenschweger F, Stucht D, Lüsebrink F, Rose G, et al. Prospective motion correction enables highest resolution time-of-flight angiography at 7T. Magn Reson Med. 2018; 80:248–258.19. Park CA, Kang CK, Kim YB, Cho ZH. Advances in MR angiography with 7T MRI: from microvascular imaging to functional angiography. Neuroimage. 2018; 168:269–278.
Article20. Amukotuwa SA, Wu A, Zhou K, Page I, Brotchie P, Bammer R. Distal medium vessel occlusions can be accurately and rapidly detected using Tmax maps. Stroke. 2021; 52:3308–3317.
Article21. Becks MJ, Manniesing R, Vister J, Pegge SAH, Steens SCA, van Dijk EJ, et al. Brain CT perfusion improves intracranial vessel occlusion detection on CT angiography. J Neuroradiol. 2019; 46:124–129.
Article22. Sousa JA, Sondermann A, Bernardo-Castro S, Varela R, Donato H, Sargento-Freitas J. CTA and CTP for detecting distal medium vessel occlusions: a systematic review and meta-analysis. AJNR Am J Neuroradiol. 2023; 45:51–56.23. Olive-Gadea M, Requena M, Diaz F, Boned S, Garcia-Tornel A, Muchada M, et al. Systematic CT perfusion acquisition in acute stroke increases vascular occlusion detection and thrombectomy rates. J Neurointerv Surg. 2022; 14:1270–1273.24. Mohammaden MH, Doheim MF, Elfil M, Al-Bayati AR, Pinheiro A, Nguyen TN, et al. Direct to angiosuite versus conventional imaging in suspected large vessel occlusion: a systemic review and meta-analysis. Stroke. 2022; 53:2478–2487.
Article25. Requena M, Olivé-Gadea M, Muchada M, Hernández D, Rubiera M, Boned S, et al. Direct to angiography suite without stopping for computed tomography imaging for patients with acute stroke: a randomized clinical trial. JAMA Neurol. 2021; 78:1099–1107.26. Seners P, Turc G, Maïer B, Mas JL, Oppenheim C, Baron JC. Incidence and predictors of early recanalization after intravenous thrombolysis: a systematic review and meta-analysis. Stroke. 2016; 47:2409–2412.
Article27. Menon BK, Al-Ajlan FS, Najm M, Puig J, Castellanos M, Dowlatshahi D, et al. Association of clinical, imaging, and thrombus characteristics with recanalization of visible intracranial occlusion in patients with acute ischemic stroke. JAMA. 2018; 320:1017–1026.28. Tian H, Parsons MW, Levi CR, Lin L, Aviv RI, Spratt NJ, et al. Influence of occlusion site and baseline ischemic core on outcome in patients with ischemic stroke. Neurology. 2019; 92:e2626–e2643.29. Lima FO, Furie KL, Silva GS, Lev MH, Camargo EC, Singhal AB, et al. Prognosis of untreated strokes due to anterior circulation proximal intracranial arterial occlusions detected by use of computed tomography angiography. JAMA Neurol. 2014; 71:151–157.30. Anadani M, Alawieh A, Chalhoub R, Jabbour P, Starke RM, Arthur A, et al. Mechanical thrombectomy for distal occlusions: efficacy, functional and safety outcomes: insight from the STAR collaboration. World Neurosurg. 2021; 151:e871–e879.31. Filioglo A, Simaan N, Honig A, Heldner MR, von Rennenberg R, Pezzini A, et al. Outcomes after reperfusion therapies in patients with ACA stroke: a multicenter cohort study from the EVATRISP collaboration. J Neurol Sci. 2022; 432:120081.32. Dabhi N, Mastorakos P, Sokolowski J, Kellogg RT, Park MS. Mechanical thrombectomy for the treatment of anterior cerebral artery occlusion: a systematic review of the literature. AJNR Am J Neuroradiol. 2022; 43:1730–1735.
Article33. Meyer L, Stracke CP, Jungi N, Wallocha M, Broocks G, Sporns PB, et al. Thrombectomy for primary distal posterior cerebral artery occlusion stroke: the TOPMOST study. JAMA Neurol. 2021; 78:434–444.34. Meyer L, Stracke P, Wallocha M, Broocks G, Sporns P, Piechowiak EI, et al. Aspiration versus stent retriever thrombectomy for distal, medium vessel occlusion stroke in the posterior circulation: a subanalysis of the TOPMOST study. Stroke. 2022; 53:2449–2457.
Article35. Saber H, Desai SM, Haussen D, Al-Bayati A, Majidi S, Mocco J, et al. Endovascular therapy vs medical management for patients with acute stroke with medium vessel occlusion in the anterior circulation. JAMA Netw Open. 2022; 5:e2238154.
Article36. Haussen DC, Eby B, Al-Bayati AR, Grossberg JA, Rodrigues GM, Frankel MR, et al. A comparative analysis of 3MAX aspiration versus 3 mm Trevo Retriever for distal occlusion thrombectomy in acute stroke. J Neurointerv Surg. 2020; 12:279–282.
Article37. Kühn AL, Wakhloo AK, Lozano JD, Massari F, De Macedo Rodrigues K, Marosfoi MG, et al. Two-year single-center experience with the ‘Baby Trevo’ stent retriever for mechanical thrombectomy in acute ischemic stroke. J Neurointerv Surg. 2017; 9:541–546.38. Rikhtegar R, Mosimann PJ, Weber R, Wallocha M, Yamac E, Mirza-Aghazadeh-Attari M, et al. Effectiveness of very low profile thrombectomy device in primary distal medium vessel occlusion, as rescue therapy after incomplete proximal recanalization or following iatrogenic thromboembolic events. J Neurointerv Surg. 2021; 13:1067–1072.39. Bourcier R, Mazighi M, Labreuche J, Fahed R, Blanc R, Gory B, et al. Susceptibility vessel sign in the ASTER trial: higher recanalization rate and more favourable clinical outcome after first line stent retriever compared to contact aspiration. J Stroke. 2018; 20:268–276.
Article40. Mohammaden MH, Haussen DC, Perry da Camara C, Pisani L, Olive Gadea M, Al-Bayati AR, et al. Hyperdense vessel sign as a potential guide for the choice of stent retriever versus contact aspiration as first-line thrombectomy strategy. J Neurointerv Surg. 2021; 13:599–604.
Article41. Kaesmacher J, Bellwald S, Dobrocky T, Meinel TR, Piechowiak EI, Goeldlin M, et al. Safety and efficacy of intra-arterial urokinase after failed, unsuccessful, or incomplete mechanical thrombectomy in anterior circulation large-vessel occlusion stroke. JAMA Neurol. 2020; 77:318–326.42. Mattle HP, Arnold M, Georgiadis D, Baumann C, Nedeltchev K, Benninger D, et al. Comparison of intraarterial and intravenous thrombolysis for ischemic stroke with hyperdense middle cerebral artery sign. Stroke. 2008; 39:379–383.43. Renú A, Millán M, San Román L, Blasco J, Martí-Fàbregas J, Terceño M, et al. Effect of intra-arterial alteplase vs placebo following successful thrombectomy on functional outcomes in patients with large vessel occlusion acute ischemic stroke: the CHOICE randomized clinical trial. JAMA. 2022; 327:826–835.44. Cimflova P, Kappelhof M, Singh N, Kashani N, Ospel JM, McDonough R, et al. Factors influencing thrombectomy decision making for primary medium vessel occlusion stroke. J Neurointerv Surg. 2022; 14:350–355.45. Singh N, Kashani N, Kappelhof M, Cimflova P, Ospel J, McDonough R, et al. Willingness to randomize primary medium vessel occlusions for endovascular treatment. J Neuroradiol. 2022; 49:157–163.
Article46. Kashani N, Cimflova P, Ospel JM, Kappelhof M, Singh N, McDonough RV, et al. Desired qualities of endovascular tools and barriers to treating medium vessel occlusion MeVO: insights from the MeVO-FRONTIERS international survey. Clin Neuroradiol. 2023; 33:155–160.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Suction thrombectomy of distal medium vessel occlusion using microcatheter during mechanical thrombectomy for acute ischemic stroke: A case series
- Emergency management of stroke in the era of mechanical thrombectomy
- Mechanical Thrombectomy in Strokes with Large-Vessel Occlusion Beyond 6 Hours: A Pooled Analysis of Randomized Trials
- A Feasible Technique for Transient Vascular Occlusion by Using a Vessel Loop and Hem-o-Lok Clips in Laparoscopic Partial Nephrectomy
- Endovascular Treatment of Large Vessel Occlusion Strokes Due to Intracranial Atherosclerotic Disease