Ann Hepatobiliary Pancreat Surg.
2024 May;28(2):115-124. 10.14701/ahbps.23-137.
Low versus standard central venous pressure during laparoscopic liver resection: A systematic review, meta-analysis and trial sequential analysis
- Affiliations
-
- 1Department of General Surgery, Weston General Hospital, Weston-Super-Mare, UK
- 2Department of General Surgery, University Hospital of Wales, Cardiff, UK
- 3School of Medicine, Imperial College London, London, UK
- 4Department of General Surgery, University Hospital Coventry & Warwickshire, Coventry, UK
- 5Department of Hepatobiliary and Pancreatic Surgery, Manchester Royal Infirmary Hospital, Manchester, UK
- KMID: 2555924
- DOI: http://doi.org/10.14701/ahbps.23-137
Abstract
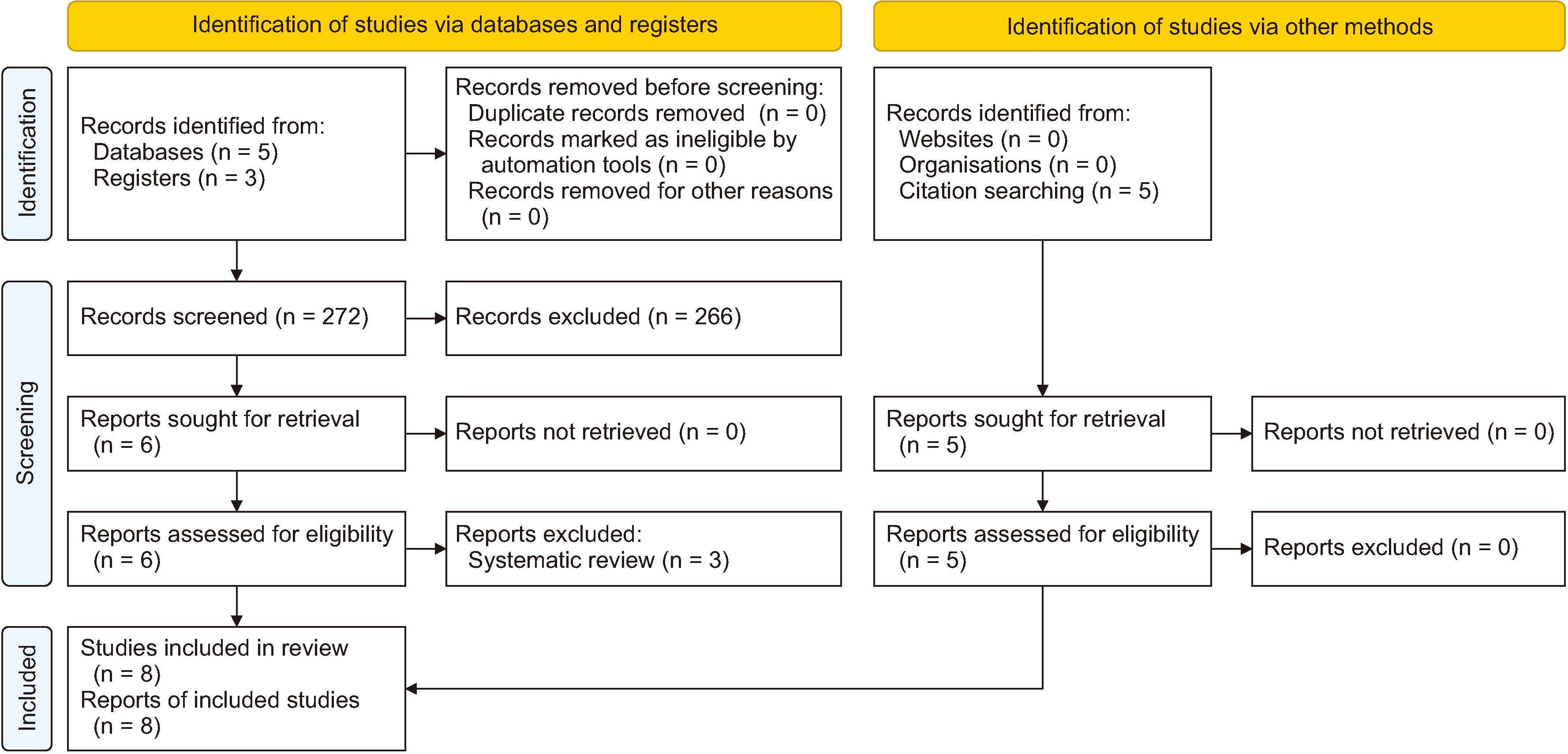
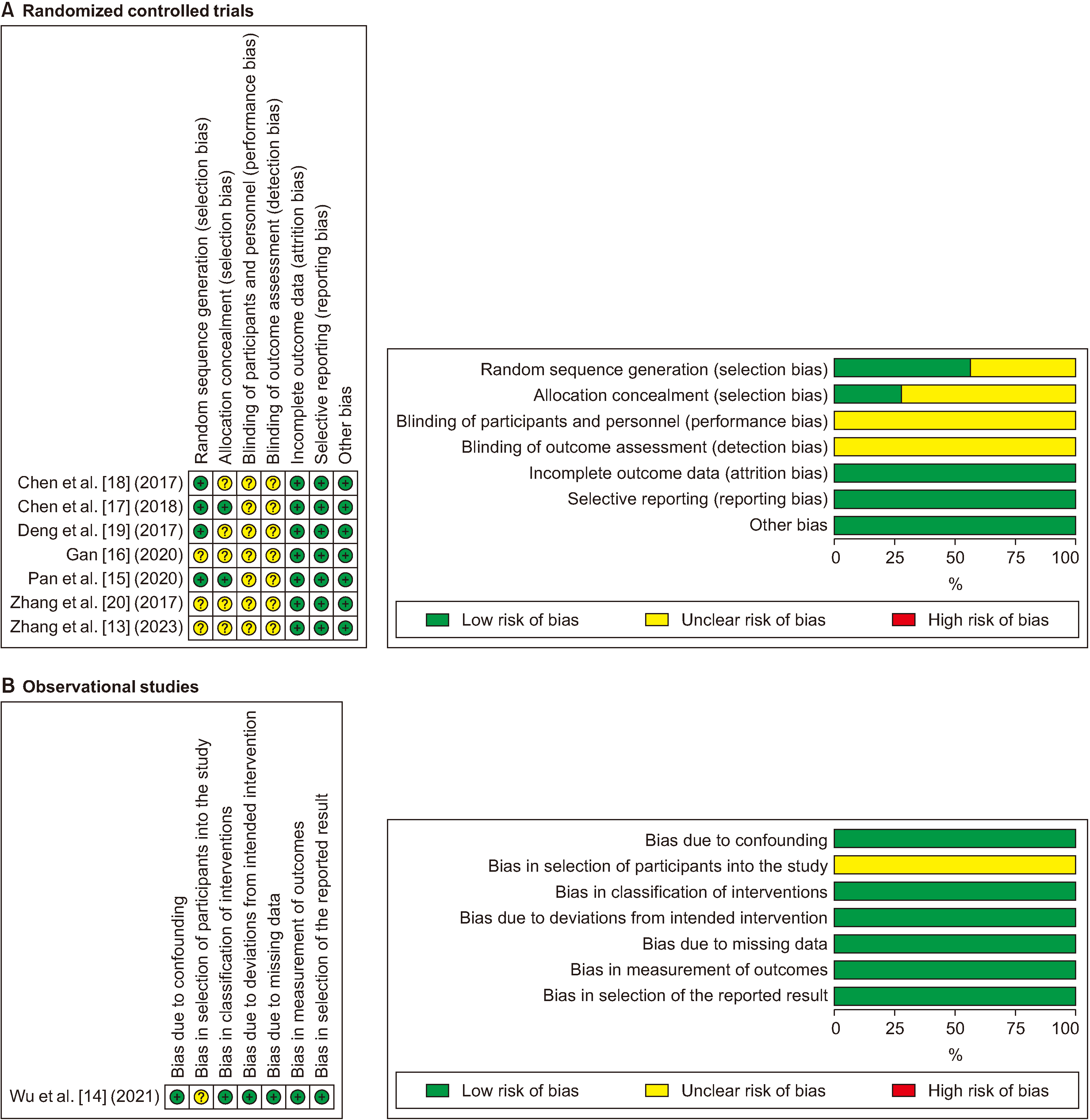
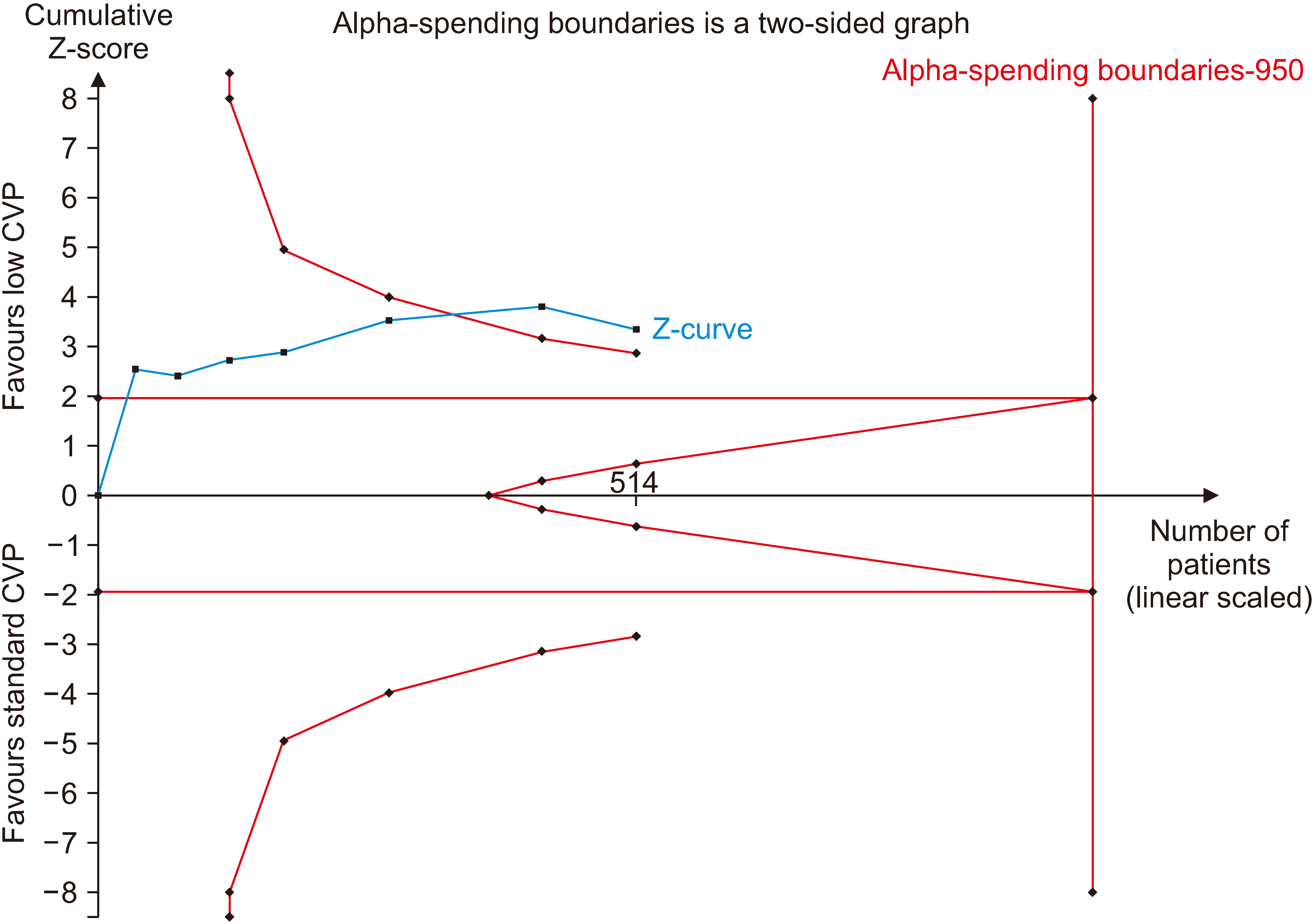
- To compare the outcomes of low central venous pressure (CVP) to standard CVP during laparoscopic liver resection. The study design was a systematic review following the PRISMA statement standards. The available literature was searched to identify all studies comparing low CVP with standard CVP in patients undergoing laparoscopic liver resection. The outcomes included intraoperative blood loss (primary outcome), need for blood transfusion, mean arterial pressure, operative time, Pringle time, and total complications. Random-effects modelling was applied for analyses. Type I and type II errors were assessed by trial sequential analysis (TSA). A total of 8 studies including 682 patients were included (low CVP group, 342; standard CVP group, 340). Low CVP reduced intraoperative blood loss during laparoscopic liver resection (mean difference [MD], –193.49 mL; 95% confidence interval [CI], –339.86 to –47.12; p = 0.01). However, low CVP did not have any effect on blood transfusion requirement (odds ratio [OR], 0.54; 95% CI, 0.28–1.03; p = 0.06), mean arterial pressure (MD, –1.55 mm Hg; 95% CI, –3.85–0.75; p = 0.19), Pringle time (MD, –0.99 minutes; 95% CI, –5.82–3.84; p = 0.69), operative time (MD, –16.38 minutes; 95% CI, –36.68–3.39; p = 0.11), or total complications (OR, 1.92; 95% CI, 0.97–3.80; p = 0.06). TSA suggested that the meta-analysis for the primary outcome was not subject to type I or II errors. Low CVP may reduce intraoperative blood loss during laparoscopic liver resection (moderate certainty); however, this may not translate into shorter operative time, shorter Pringle time, or less need for blood transfusion. Randomized controlled trials with larger sample sizes will provide more robust evidence.
Keyword
Figure
Reference
-
References
1. Jarnagin WR, Gonen M, Fong Y, DeMatteo RP, Ben-Porat L, Little S, et al. 2002; Improvement in perioperative outcome after hepatic resection: analysis of 1,803 consecutive cases over the past decade. Ann Surg. 236:397–406. discussion 406–407. DOI: 10.1097/00000658-200210000-00001. PMID: 12368667. PMCID: PMC1422593.2. Gurusamy KS, Sheth H, Kumar Y, Sharma D, Davidson BR. Methods of vascular occlusion for elective liver resections. Cochrane Database Syst Rev. 2009; (1):CD007632. DOI: 10.1002/14651858.CD006409.pub3. PMID: 19160283. PMCID: PMC10654807.
Article3. Lesurtel M, Selzner M, Petrowsky H, McCormack L, Clavien PA. 2005; How should transection of the liver be performed?: a prospective randomized study in 100 consecutive patients: comparing four different transection strategies. Ann Surg. 242:814–822. DOI: 10.1097/01.sla.0000189121.35617.d7. PMID: 16327491. PMCID: PMC1409877.4. McNally SJ, Revie EJ, Massie LJ, McKeown DW, Parks RW, Garden OJ, et al. 2012; Factors in perioperative care that determine blood loss in liver surgery. HPB (Oxford). 14:236–241. DOI: 10.1111/j.1477-2574.2011.00433.x. PMID: 22404261. PMCID: PMC3371209.
Article5. Liu TS, Shen QH, Zhou XY, Shen X, Lai L, Hou XM, et al. 2021; Application of controlled low central venous pressure during hepatectomy: a systematic review and meta-analysis. J Clin Anesth. 75:110467. DOI: 10.1016/j.jclinane.2021.110467. PMID: 34343737.
Article6. Hajibandeh S, Kotb A, Evans L, Sams E, Naguib A, Hajibandeh S, et al. 2023; Procedural outcomes of laparoscopic caudate lobe resection: a systematic review and meta-analysis. Ann Hepatobiliary Pancreat Surg. 27:6–19. DOI: 10.14701/ahbps.22-045. PMID: 36245071. PMCID: PMC9947369.
Article7. Hajibandeh S, Hajibandeh S, Dave M, Tarazi M, Satyadas T. 2020; Laparoscopic versus open liver resection for tumors in the posterosuperior segments: a systematic review and meta-analysis. Surg Laparosc Endosc Percutan Tech. 30:93–105. DOI: 10.1097/SLE.0000000000000746. PMID: 31929396.
Article8. Rhu J, Kim SJ, Choi GS, Kim JM, Joh JW, Kwon CHD. 2018; Laparoscopic versus open right posterior sectionectomy for hepatocellular carcinoma in a high-volume center: a propensity score matched analysis. World J Surg. 42:2930–2937. DOI: 10.1007/s00268-018-4531-z. PMID: 29426971.
Article9. Liberati A, Altman DG, Tetzlaff J, Mulrow C, Gøtzsche PC, Ioannidis JP, et al. 2009; The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate healthcare interventions: explanation and elaboration. BMJ. 339:b2700. DOI: 10.1136/bmj.b2700. PMID: 19622552. PMCID: PMC2714672.
Article10. Higgins JPT, Savović J, Page MJ, Elbers RG, Sterne JAC. Cochrane handbook for systematic reviews of interventions. Chapter 8: assessing risk of bias in a randomized trial [Internet]. Available from: https://training.cochrane.org/handbook/current/chapter-08. Cochrane;2011. cited 2018 Oct 10.11. Sterne JA, Hernán MA, Reeves BC, Savović J, Berkman ND, Viswanathan M, et al. 2016; ROBINS-I: a tool for assessing risk of bias in non-randomised studies of interventions. BMJ. 355:i4919. DOI: 10.1136/bmj.i4919. PMID: 27733354. PMCID: PMC5062054.
Article12. Schünemann H, Brożek J, Guyatt G, Oxman A. 2013. GRADE handbook for grading quality of evidence and strength of recommendations [Internet]. GRADE;Available from: https://gdt.gradepro.org/app/handbook/handbook.html. cited 2023 Aug 20.13. Zhang Y, Li L, Xu J, Cheng W. 2023; Effects of controlled low central venous pressure combined with dexmedetomidine on the blood loss, renal function and cognitive function in patients undergoing laparoscopic hepatectomy. Signa Vitae. 19:182–187.14. Wu G, Chen T, Chen Z. 2021; Effect of controlled low central venous pressure technique on postoperative hepatic insufficiency in patients undergoing a major hepatic resection. Am J Transl Res. 13:8286–8293.15. Pan YX, Wang JC, Lu XY, Chen JB, He W, Chen JC, et al. 2020; Intention to control low central venous pressure reduced blood loss during laparoscopic hepatectomy: a double-blind randomized clinical trial. Surgery. 167:933–941. DOI: 10.1016/j.surg.2020.02.004. PMID: 32216964.
Article16. Gan Q. 2020; Application effect of controlled low central venous pressure technique in laparoscopic hepatectomy. Chin Mod Med. 27:62–64.17. Chen X, Hu CH, Peng YH, Luo H, Yang P. 2018; Prospective randomized controlled study on controlled low central venous pressure in laparoscopic hepatectomy. Chin J Min Inv Surg. 208:15–19.18. Chen J, Xiao X, Wang JX, Xin CH, Wu JJ, Cai WH. 2017; Clinical application of low central venous pressure in laparoscopic hepatectomy. J Hepatobiliary Surg. 25:423–426.19. Deng DJ, Zhang YN, Zeng ZW, Lin YH, Luo R, Zhang WQ. 2017; Transesophageal echocardiography monitoring for laparoscopic hepatectomy combined with low central venous pressure. Lingnan Mod Clin Surg. 17:528–534.20. Zhang YN, Luo R, Deng JD, Zhang WQ, Lin WX, Zeng ZW, et al. 2017; Clinical application of controlled low central venous pressure in laparoscopic hepatectomy. Lingnan Mod Clin Surg. 17:423–431.21. Hughes MJ, Ventham NT, Harrison EM, Wigmore SJ. 2015; Central venous pressure and liver resection: a systematic review and meta-analysis. HPB (Oxford). 17:863–871. DOI: 10.1111/hpb.12462. PMID: 26292655. PMCID: PMC4571753.
Article22. Wang WD, Liang LJ, Huang XQ, Yin XY. 2006; Low central venous pressure reduces blood loss in hepatectomy. World J Gastroenterol. 12:935–939. DOI: 10.3748/wjg.v12.i6.935. PMID: 16521223. PMCID: PMC4066160.
Article23. Lai PB, Chui PT, Leow CK, Lau WY. 1998; Correlation between blood loss and inferior vena caval pressure during liver resection. Br J Surg. 85:1158. DOI: 10.1046/j.1365-2168.1998.00570.x. PMID: 9501812.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Preoperative dexmedetomidine and intraoperative bradycardia in laparoscopic cholecystectomy: a meta-analysis with trial sequential analysis
- Trial sequential analysis: novel approach for meta-analysis
- An Introduction of the Systematic Review and Meta-Analysis
- Introduction to systematic review and meta-analysis
- Systematic Review and Meta-analysis in Digestive Cancer Research