Clin Endosc.
2024 May;57(3):317-328. 10.5946/ce.2023.205.
Efficacy and safety of endoscopic submucosal dissection for colorectal dysplasia in patients with inflammatory bowel disease: a systematic review and meta-analysis
- Affiliations
-
- 1Department of Internal Medicine, Chicago Medical School at Rosalind Franklin University of Medicine and Science, North Chicago, IL, USA
- 2Department of Gastroenterology and Hepatology, University of Utah School of Medicine, Salt Lake City, UT, USA
- 3Department of Gastroenterology & Hepatology, Orlando Gastroenterology PA, Orlando, FL, USA
- 4Department of Gastroenterology and Hepatology, Cleveland Clinic Florida, Weston, FL, USA
- 5Gastroenterology and Hepatology Section, Baylor College of Medicine, Houston, TX, USA
- 6Department of Gastroenterology, Hepatology, and Nutrition, University of Florida, Gainesville, FL, USA
- 7Division of Gastroenterology, Hepatology and Nutrition, Allegheny Health Network, Pittsburgh, PA, USA
- KMID: 2555892
- DOI: http://doi.org/10.5946/ce.2023.205
Abstract
- Background/Aims
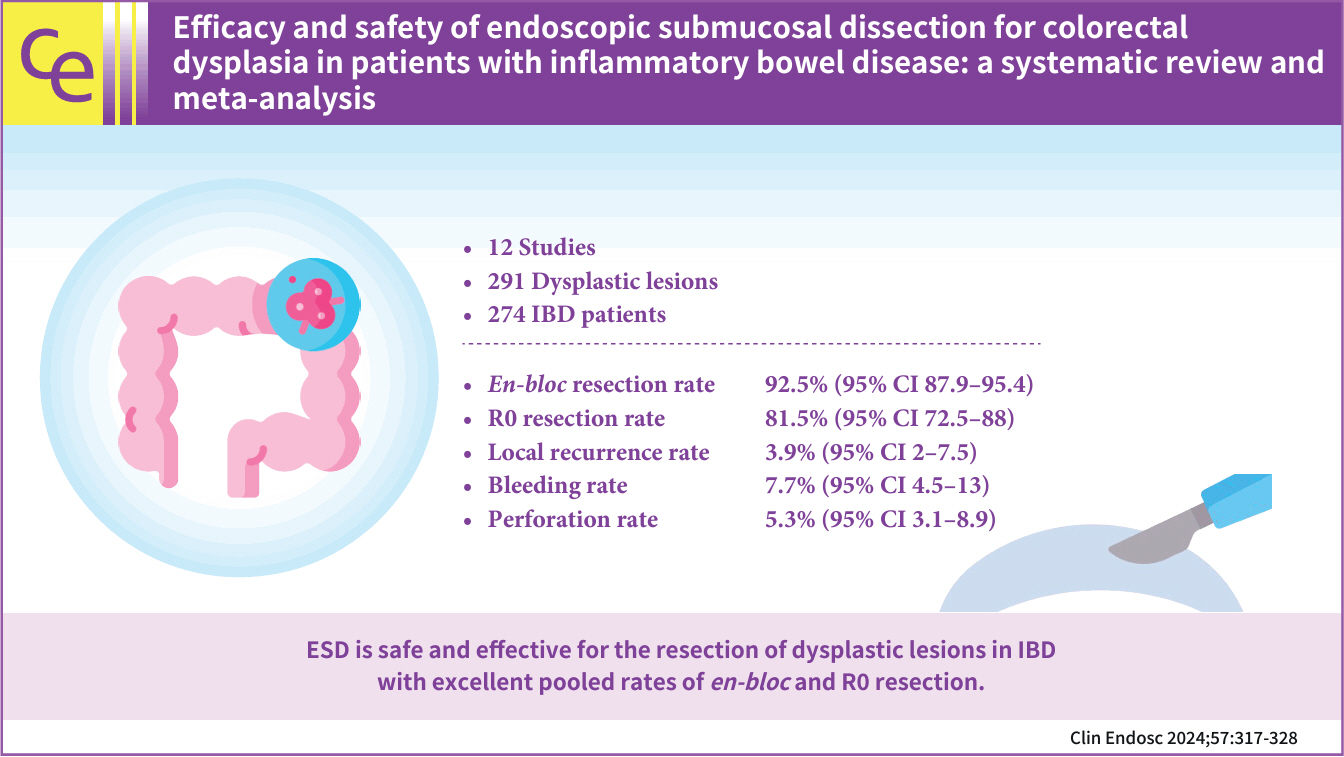
In this meta-analysis, we studied the safety and efficacy of endoscopic submucosal dissection (ESD) for colorectal dysplasia in patients with inflammatory bowel disease (IBD).
Methods
Multiple databases were searched, and studies were retrieved based on pre-specified criteria until October 2022. The outcomes assessed were resection rates, procedural complications, local recurrence, metachronous tumors, and the need for surgery after ESD in IBD. Standard meta-analysis methods were followed using the random-effects model, and I2% was used to assess heterogeneity.
Results
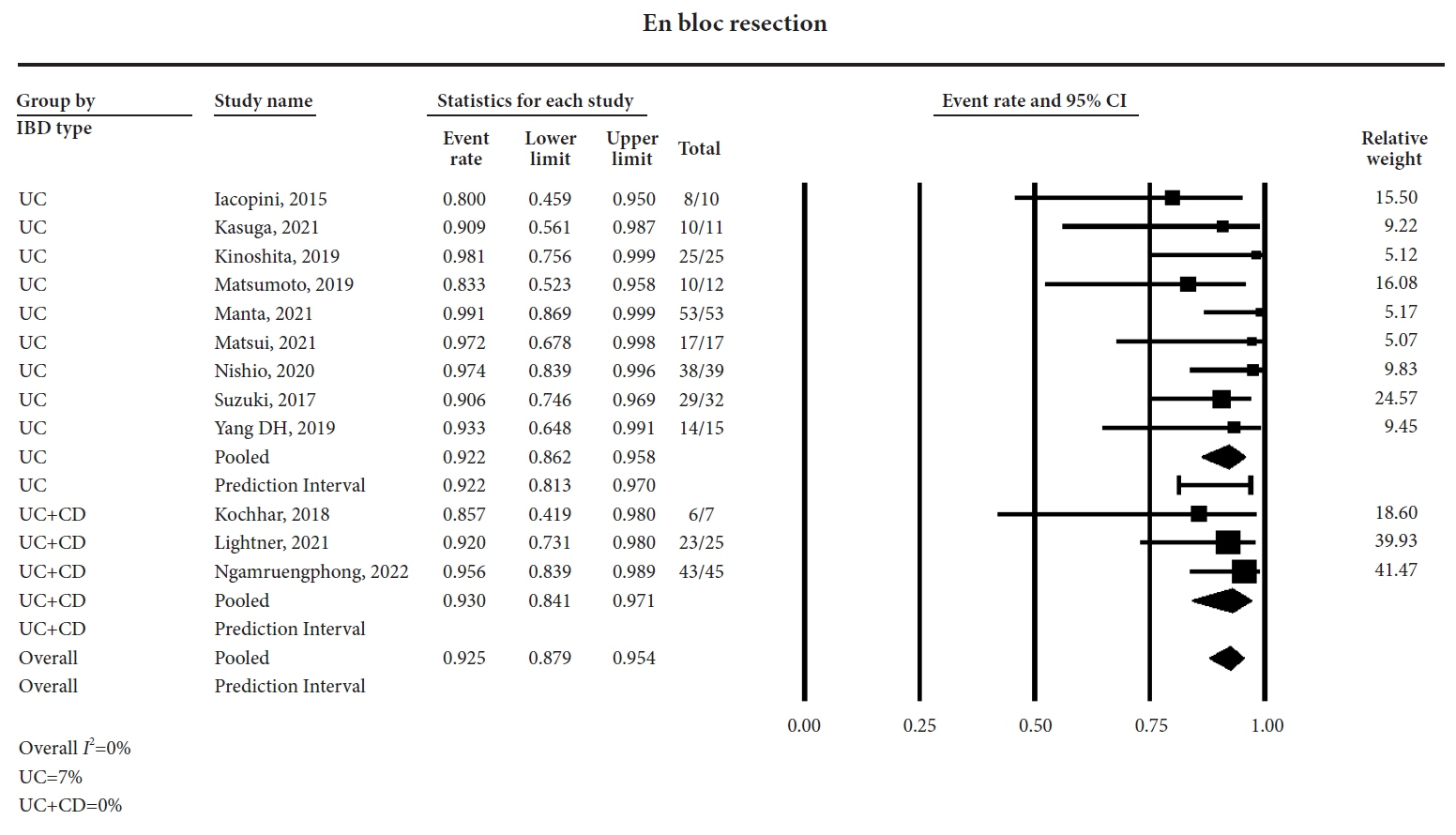
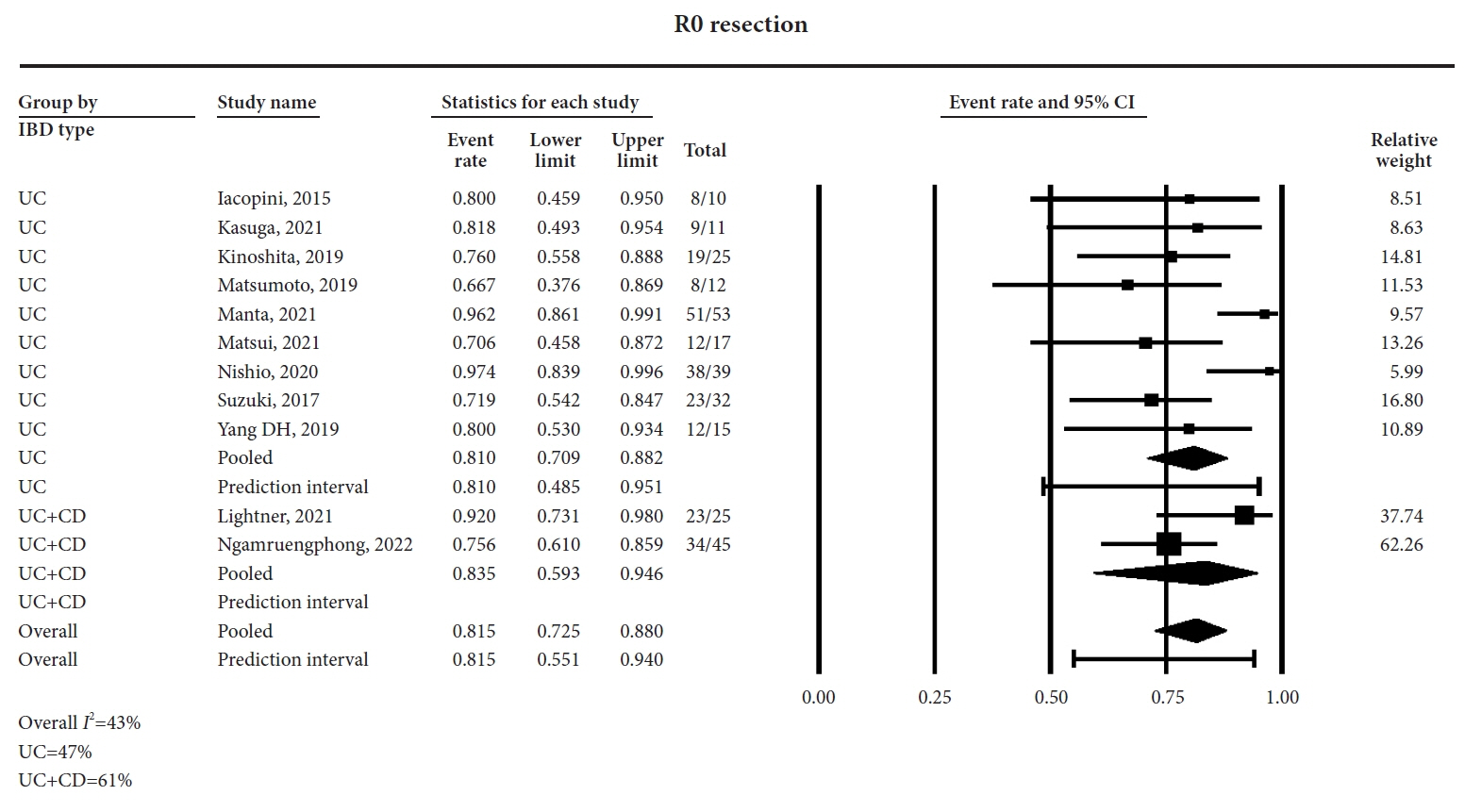
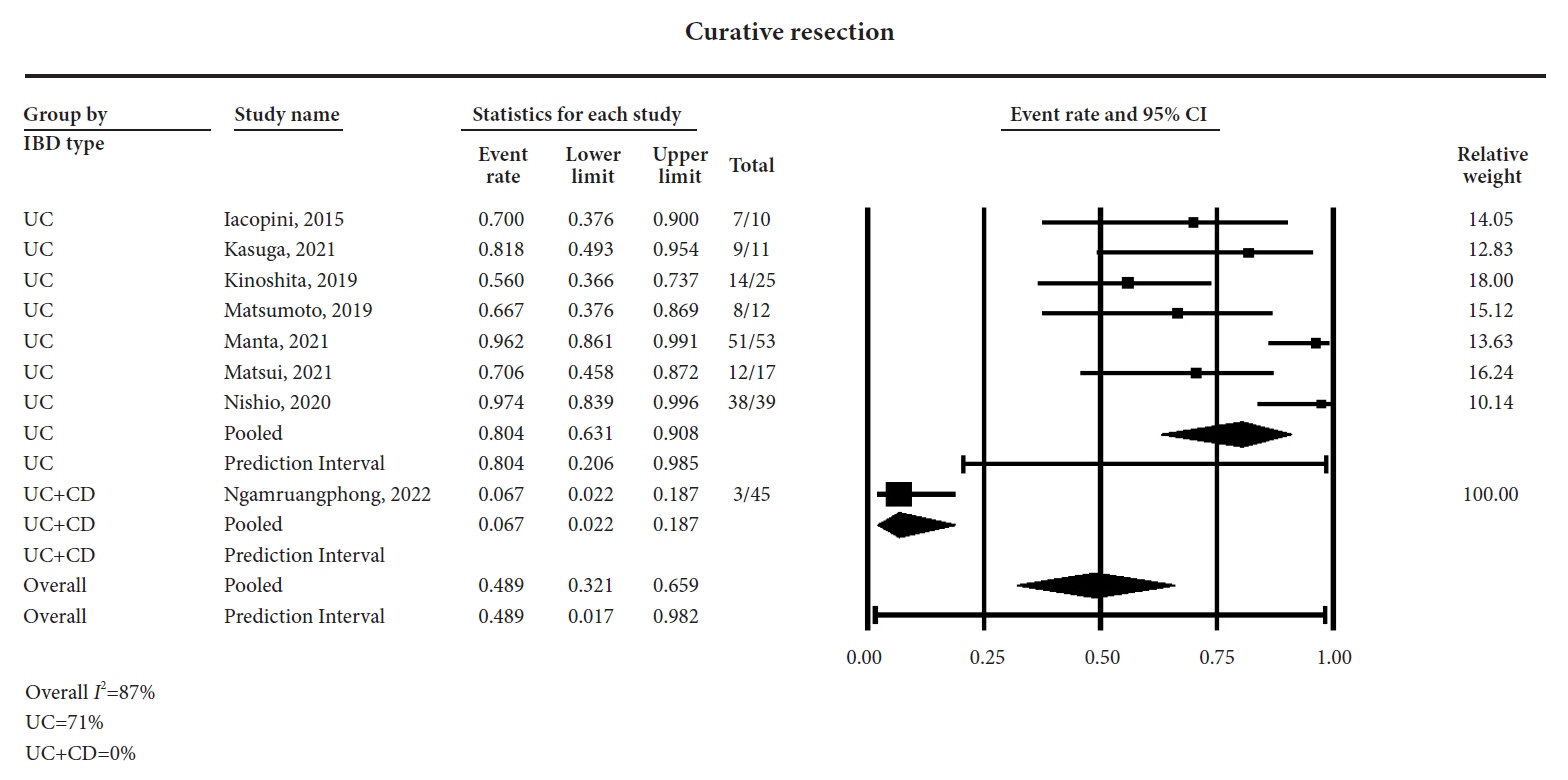
Twelve studies comprising 291 dysplastic lesions in 274 patients were included with a median follow-up of 25 months. The pooled en-bloc resection, R0 resection, and curative resection rates were 92.5% (95% confidence interval [CI], 87.9%–95.4%; I2=0%), 81.5% (95% CI, 72.5%–88%; I2=43%), and 48.9% (95% CI, 32.1%–65.9%; I2=87%), respectively. The local recurrence rate was 3.9% (95% CI, 2%–7.5%; I2=0%). The pooled rates of bleeding and perforation were 7.7% (95% CI, 4.5%–13%; I2=10%) and 5.3% (95% CI, 3.1%–8.9%; I2=0%), respectively. The rates of metachronous recurrence and additional surgery following ESD were 10% (95% CI, 5.2%–18.2%; I2=55%) and 13% (95% CI, 8.5%–19.3%; I2=54%), respectively.
Conclusions
ESD is safe and effective for the resection of dysplastic lesions in IBD with an excellent pooled rate of en-bloc and R0 resection.
Figure
Reference
-
1. Jess T, Simonsen J, Jørgensen KT, et al. Decreasing risk of colorectal cancer in patients with inflammatory bowel disease over 30 years. Gastroenterology. 2012; 143:375–381.
Article2. Eaden JA, Abrams KR, Mayberry JF. The risk of colorectal cancer in ulcerative colitis: a meta-analysis. Gut. 2001; 48:526–535.
Article3. Choi CH, Rutter MD, Askari A, et al. Forty-year analysis of colonoscopic surveillance program for neoplasia in ulcerative colitis: an updated overview. Am J Gastroenterol. 2015; 110:1022–1034.
Article4. Pimentel-Nunes P, Dinis-Ribeiro M, Ponchon T, et al. Endoscopic submucosal dissection: European Society of Gastrointestinal Endoscopy (ESGE) Guideline. Endoscopy. 2015; 47:829–854.
Article5. Laine L, Kaltenbach T, Barkun A, et al. SCENIC international consensus statement on surveillance and management of dysplasia in inflammatory bowel disease. Gastroenterology. 2015; 148:639–651.
Article6. American Society for Gastrointestinal Endoscopy Standards of Practice Committee, Shergill AK, Lightdale JR, et al. The role of endoscopy in inflammatory bowel disease. Gastrointest Endosc. 2015; 81:1101–1121.
Article7. Rutter MD, Riddell RH. Colorectal dysplasia in inflammatory bowel disease: a clinicopathologic perspective. Clin Gastroenterol Hepatol. 2014; 12:359–367.
Article8. Draganov PV, Wang AY, Othman MO, et al. AGA institute clinical practice update: endoscopic submucosal dissection in the United States. Clin Gastroenterol Hepatol. 2019; 17:16–25.
Article9. Uraoka T, Parra-Blanco A, Yahagi N. Colorectal endoscopic submucosal dissection in Japan and Western countries. Dig Endosc. 2012; 24 Suppl 1:80–83.
Article10. Hurlstone DP, Sanders DS, Atkinson R, et al. Endoscopic mucosal resection for flat neoplasia in chronic ulcerative colitis: can we change the endoscopic management paradigm? Gut. 2007; 56:838–846.
Article11. Wang J, Zhang XH, Ge J, et al. Endoscopic submucosal dissection vs endoscopic mucosal resection for colorectal tumors: a meta-analysis. World J Gastroenterol. 2014; 20:8282–8287.
Article12. Page MJ, McKenzie JE, Bossuyt PM, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. Syst Rev. 2021; 10:89.
Article13. Stroup DF, Berlin JA, Morton SC, et al. Meta-analysis of observational studies in epidemiology: a proposal for reporting. Meta-analysis Of Observational Studies in Epidemiology (MOOSE) group. JAMA. 2000; 283:2008–2012.
Article14. Stang A. Critical evaluation of the Newcastle-Ottawa scale for the assessment of the quality of nonrandomized studies in meta-analyses. Eur J Epidemiol. 2010; 25:603–605.
Article15. Iacopini F, Saito Y, Yamada M, et al. Curative endoscopic submucosal dissection of large nonpolypoid superficial neoplasms in ulcerative colitis (with videos). Gastrointest Endosc. 2015; 82:734–738.
Article16. Kasuga K, Yamada M, Shida D, et al. Treatment outcomes of endoscopic submucosal dissection and surgery for colorectal neoplasms in patients with ulcerative colitis. United European Gastroenterol J. 2021; 9:964–972.
Article17. Kochhar G, Steele S, Sanaka M, et al. Endoscopic submucosal dissection for flat colonic polyps in patients with inflammatory bowel disease: a single-center experience. Inflamm Bowel Dis. 2018; 24:e14–e15.
Article18. Kinoshita S, Nishizawa T, Yahagi N, et al. Endoscopic submucosal dissection in patients with ulcerative colitis. Digestion. 2019; 99:27–32.
Article19. Lightner AL, Vaidya P, Allende D, et al. Endoscopic submucosal dissection is safe and feasible, allowing for ongoing surveillance and organ preservation in patients with inflammatory bowel disease. Colorectal Dis. 2021; 23:2100–2107.
Article20. Matsumoto K, Oka S, Tanaka S, et al. Long-term outcomes after endoscopic submucosal dissection for ulcerative colitis-associated dysplasia. Digestion. 2021; 102:205–215.
Article21. Manta R, Zullo A, Telesca DA, et al. Endoscopic submucosal dissection for visible dysplasia treatment in ulcerative colitis patients: cases series and systematic review of literature. J Crohns Colitis. 2021; 15:165–168.
Article22. Matsui A, Hoteya S, Hayasaka J, et al. Real-world experience of endoscopic submucosal dissection for ulcerative colitis-associated neoplasia. Inflamm Intest Dis. 2021; 6:70–77.
Article23. Ngamruengphong S, Aihara H, Friedland S, et al. Endoscopic submucosal dissection for colorectal dysplasia in inflammatory bowel disease: a US multicenter study. Endosc Int Open. 2022; 10:E354–E360.
Article24. Nishio M, Hirasawa K, Ozeki Y, et al. An endoscopic treatment strategy for superficial tumors in patients with ulcerative colitis. J Gastroenterol Hepatol. 2021; 36:498–506.
Article25. Suzuki N, Toyonaga T, East JE. Endoscopic submucosal dissection of colitis-related dysplasia. Endoscopy. 2017; 49:1237–1242.
Article26. Yang DH, Kim J, Song EM, et al. Outcomes of ulcerative colitis-associated dysplasia patients referred for potential endoscopic submucosal dissection. J Gastroenterol Hepatol. 2019; 34:1581–1589.
Article27. Puhan MA, Schünemann HJ, Murad MH, et al. A GRADE Working Group approach for rating the quality of treatment effect estimates from network meta-analysis. BMJ. 2014; 349:g5630.
Article28. Alkandari A, Thayalasekaran S, Bhandari M, et al. Endoscopic resections in inflammatory bowel disease: a multicentre European outcomes study. J Crohns Colitis. 2019; 13:1394–1400.
Article29. Yadav S, Loftus EV Jr, Harmsen WS, et al. Outcome of endoscopic resection of colonic polyps larger than 10 mm in patients with inflammatory bowel disease. Endosc Int Open. 2019; 7:E994–E1001.
Article30. Yu JX, Lin JL, Oliver M, et al. Trends in EMR for nonmalignant colorectal polyps in the United States. Gastrointest Endosc. 2020; 91:124–131.
Article31. Akintoye E, Kumar N, Aihara H, et al. Colorectal endoscopic submucosal dissection: a systematic review and meta-analysis. Endosc Int Open. 2016; 4:E1030–E1044.
Article32. Patel N, Patel K, Ashrafian H, et al. Colorectal endoscopic submucosal dissection: systematic review of mid-term clinical outcomes. Dig Endosc. 2016; 28:405–416.
Article33. Mohapatra S, Sankaramangalam K, Lopimpisuth C, et al. Advanced endoscopic resection for colorectal dysplasia in inflammatory bowel disease: a meta-analysis. Endosc Int Open. 2022; 10:E593–E601.
Article34. Chen W, Zhang YL, Zhao Y, et al. Endoscopic resection for non-polypoid dysplasia in inflammatory bowel disease: a systematic review and meta-analysis. Surg Endosc. 2021; 35:1534–1543.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Endoscopic Submucosal Dissection for Colitis-Associated Dysplasia
- Endoscopic Therapeutic Approach for Dysplasia in Inflammatory Bowel Disease
- International Digestive Endoscopy Network to Strengthen Network for Lower Gastrointestinal Diseases Including Inflammatory Bowel Disease and Colorectal Cancer
- Debates on Colorectal Endoscopic Submucosal Dissection - Traction for Effective Dissection: Gravity Is Enough
- Non-conventional dysplastic subtypes in inflammatory bowel disease: a review of their diagnostic characteristics and potential clinical implications