Brain Tumor Res Treat.
2024 Apr;12(2):100-108. 10.14791/btrt.2024.0011.
Application of a Standardized Treatment Paradigm as a Strategy to Achieve Optimal Onco-Functional Balance in Glioma Surgery
- Affiliations
-
- 1Division of Neurosurgery, Department of Surgery, National University Health System, Singapore
- 2Yong Loo Lin School of Medicine, National University Singapore, Singapore Departments of 3 Psychological Medicine and 4 Anaesthesia, National University Health System, Singapore
- KMID: 2555868
- DOI: http://doi.org/10.14791/btrt.2024.0011
Abstract
- Background
Gliomas, characterized by their invasive persistence and tendency to affect critical brain regions, pose a challenge in surgical resection due to the risk of neurological deficits. This study focuses on a personalized approach to achieving an optimal onco-functional balance in glioma resections, emphasizing maximal tumor removal while preserving the quality of life.
Methods
A retrospective analysis of 57 awake surgical resections of gliomas at the National University Hospital, Singapore, was conducted. The inclusion criteria were based on diagnosis, functional boundaries determined by direct electrical stimulation, preoperative Karnofsky Performance Status score, and absence of multifocal disease on MRI. The treatment approach included comprehensive neuropsychological evaluation, determination of suitability for awake surgery, and standard asleepawake-asleep anesthesia protocol. Tumor resection techniques and postoperative care were systematically followed.
Results
The study included 53 patients (55.5% male, average age 39 years), predominantly right-handed. Over half reported seizures as their chief complaint. Tumors were mostly low-grade gliomas. Positive mapping of the primary motor cortex was conducted in all cases, with awake surgery completed in 77.2% of cases. New neurological deficits were observed in 26.3% of patients at 1 month after operation; most showed significant improvement at 6 months.
Conclusion
The standardized treatment paradigm effectively achieved an optimal onco-functional balance in glioma patients. While some patients experienced neurological deficits postoperatively, the majority recovered to their preoperative baseline within 3 months. The approach prioritizes patient empowerment and customized utilization of functional mapping techniques, considering the challenge of preserving diverse languages in a multilingual patient population.
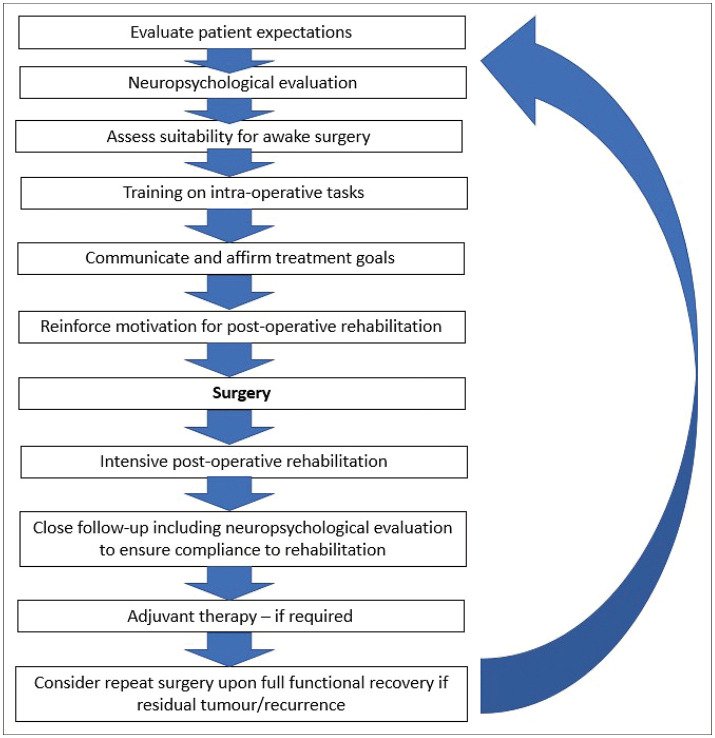
Figure
Reference
-
1. Duffau H, Taillandier L. New concepts in the management of diffuse low-grade glioma: proposal of a multistage and individualized therapeutic approach. Neuro Oncol. 2015; 17:332–342. PMID: 25087230.2. Gupta K, Salunke P. Molecular markers of glioma: an update on recent progress and perspectives. J Cancer Res Clin Oncol. 2012; 138:1971–1981. PMID: 23052697.3. Hervey-Jumper SL, Berger MS. Role of surgical resection in low- and high-grade gliomas. Curr Treat Options Neurol. 2014; 16:284. PMID: 24595756.4. Southwell DG, Birk HS, Han SJ, Li J, Sall JW, Berger MS. Resection of gliomas deemed inoperable by neurosurgeons based on preoperative imaging studies. J Neurosurg. 2018; 129:567–575. PMID: 29125414.5. Weller M, Wick W, Aldape K, Brada M, Berger M, Pfister SM, et al. Glioma. Nat Rev Dis Primers. 2015; 1:15017. PMID: 27188790.6. Kow CY, Kim BJH, Park TI, Chen JCC, Vong CK, Kim JY, et al. Extent of resection affects prognosis for patients with glioblastoma in non-eloquent regions. J Clin Neurosci. 2020; 80:242–249. PMID: 33099354.7. Ammirati M, Vick N, Liao YL, Ciric I, Mikhael M. Effect of the extent of surgical resection on survival and quality of life in patients with supratentorial glioblastomas and anaplastic astrocytomas. Neurosurgery. 1987; 21:201–206. PMID: 2821446.8. Nabors LB, Portnow J, Ahluwalia M, Baehring J, Brem H, Brem S, et al. Central nervous system cancers, version 3.2020, NCCN clinical practice guidelines in oncology. J Natl Compr Canc Netw. 2020; 18:1537–1570. PMID: 33152694.9. Duffau H, Capelle L, Denvil D, Sichez N, Gatignol P, Taillandier L, et al. Usefulness of intraoperative electrical subcortical mapping during surgery for low-grade gliomas located within eloquent brain regions: functional results in a consecutive series of 103 patients. J Neurosurg. 2003; 98:764–778. PMID: 12691401.10. Ahsan SA, Chendeb K, Briggs RG, Fletcher LR, Jones RG, Chakraborty AR, et al. Beyond eloquence and onto centrality: a new paradigm in planning supratentorial neurosurgery. J Neurooncol. 2020; 146:229–238. PMID: 31894519.11. Duffau H, Capelle L, Sichez J, Faillot T, Abdennour L, Law Koune JD, et al. Intra-operative direct electrical stimulations of the central nervous system: the Salpêtrière experience with 60 patients. Acta Neurochir (Wien). 1999; 141:1157–1167. PMID: 10592115.12. Sagar S, Rick J, Chandra A, Yagnik G, Aghi MK. Functional brain mapping: overview of techniques and their application to neurosurgery. Neurosurg Rev. 2019; 42:639–647. PMID: 30006663.13. Lacroix M, Abi-Said D, Fourney DR, Gokaslan ZL, Shi W, DeMonte F, et al. A multivariate analysis of 416 patients with glioblastoma multiforme: prognosis, extent of resection, and survival. J Neurosurg. 2001; 95:190–198.14. Cargnelutti E, Ius T, Skrap M, Tomasino B. What do we know about pre- and postoperative plasticity in patients with glioma? A review of neuroimaging and intraoperative mapping studies. Neuroimage Clin. 2020; 28:102435. PMID: 32980599.15. van Kessel E, Baumfalk AE, van Zandvoort MJE, Robe PA, Snijders TJ. Tumor-related neurocognitive dysfunction in patients with diffuse glioma: a systematic review of neurocognitive functioning prior to anti-tumor treatment. J Neurooncol. 2017; 134:9–18. PMID: 28567586.16. Bertani G, Fava E, Casaceli G, Carrabba G, Casarotti A, Papagno C, et al. Intraoperative mapping and monitoring of brain functions for the resection of low-grade gliomas: technical considerations. Neurosurg Focus. 2009; 27:E4.17. Hervey-Jumper SL, Berger MS. Maximizing safe resection of low- and high-grade glioma. J Neurooncol. 2016; 130:269–282. PMID: 27174197.18. Duffau H. The challenge to remove diffuse low-grade gliomas while preserving brain functions. Acta Neurochir (Wien). 2012; 154:569–574. PMID: 22278663.19. Sanai N, Berger MS. Surgical oncology for gliomas: the state of the art. Nat Rev Clin Oncol. 2018; 15:112–125. PMID: 29158591.20. Duffau H. Lessons from brain mapping in surgery for low-grade glioma: insights into associations between tumour and brain plasticity. Lancet Neurol. 2005; 4:476–486. PMID: 16033690.21. Motomura K, Ohka F, Aoki K, Saito R. Supratotal resection of gliomas with awake brain mapping: maximal tumor resection preserving motor, language, and neurocognitive functions. Front Neurol. 2022; 13:874826. PMID: 35645972.22. Schiffman HF. Bilingualism in South Asia: friend or foe. Cohen J, McAlister KT, Rolstad K, MacSwan J, editors. ISB4: Proceedings of the 4th International Symposium on Bilingualism. Somerville: Cascadilla Press;2005. p. 2104–2114.23. Illes J, Francis WS, Desmond JE, Gabrieli JD, Glover GH, Poldrack R, et al. Convergent cortical representation of semantic processing in bilinguals. Brain Lang. 1999; 70:347–363. PMID: 10600225.24. Halsband U. Bilingual and multilingual language processing. J Physiol Paris. 2006; 99:355–369. PMID: 16723214.25. Klein D, Watkins KE, Zatorre RJ, Milner B. Word and nonword repetition in bilingual subjects: a PET study. Hum Brain Mapp. 2006; 27:153–161. PMID: 16035048.26. Moniz-Garcia D, Bojaxhi E, Borah BJ, Dholakia R, Kim H, Sousa-Pinto B, et al. Awake craniotomy program implementation. JAMA Netw Open. 2024; 7:e2352917. PMID: 38265799.27. Leon-Rojas JE, Ekert JO, Kirkman MA, Sewell D, Bisdas S, Samandouras G. Experience with awake throughout craniotomy in tumour surgery: technique and outcomes of a prospective, consecutive case series with patient perception data. Acta Neurochir (Wien). 2020; 162:3055–3065. PMID: 33006649.28. Groshev A, Padalia D, Patel S, Garcia-Getting R, Sahebjam S, Forsyth PA, et al. Clinical outcomes from maximum-safe resection of primary and metastatic brain tumors using awake craniotomy. Clin Neurol Neurosurg. 2017; 157:25–30. PMID: 28384595.29. Tan CL, Jain S, Chan HM, Loh NW, Teo K. Awake craniotomy for brain tumor resection: patient experience and acceptance in an Asian population. Asia Pac J Clin Oncol. 2023; 19:172–178. PMID: 35678489.30. Tan J, Loh NW, Chan HM, Teo K, Lim MJR. Cognition, emotional states and health-related quality of life in awake craniotomy for glioma: a case series. World Neurosurg. 2023; 179:e428–e443. PMID: 37660841.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Assessment of Lower Limb Motor Function, Ambulation, and Balance After Stroke
- Narrative Review of Clinical Impact of Head-Hip Offset Following Adult Spinal Deformity Surgery
- Treatment of Adult Gliomas: A Current Update
- Recent Update in Pharmacological Agents for Optic Pathway Glioma
- Clinical observation on brainstem glioma in childhood