J Korean Neurosurg Soc.
2024 Mar;67(2):137-145. 10.3340/jkns.2023.0168.
Narrative Review of Clinical Impact of Head-Hip Offset Following Adult Spinal Deformity Surgery
- Affiliations
-
- 1Department of Neurosurgery, Spine Center, Seoul National University Bundang Hospital, Seoul National University College of Medicine, Seongnam, Korea
- KMID: 2553119
- DOI: http://doi.org/10.3340/jkns.2023.0168
Abstract
- In adult spinal deformity (ASD) surgery, mechanical failure (MF) has been a significant concern for spine surgeons as well as patients. Despite earnest endeavors to prevent MF, the absence of a definitive consensus persists, owing to the intricate interplay of multifarious factors associated with this complication. Previous approaches centered around global spinal alignment have yielded limited success in entirely forestalling MF. These methodologies, albeit valuable, exhibited limitations by neglecting to encompass global balance and compensatory mechanisms within their purview. In response to this concern, an in-depth comprehension of global balance and compensatory mechanisms emerges as imperative. In this discourse, the center of gravity and the gravity line are gaining attention in recent investigations pertaining to global balance. This narrative review aims to provide an overview of the global balance and a comprehensive understanding of related concepts and knowledge. Moreover, it delves into the clinical ramifications of the contemporary optimal correction paradigm to furnish an encompassing understanding of global balance and the current optimal correction strategies within the context of ASD surgery. By doing so, it endeavors to furnish spine surgeons with a guiding compass, enriching their decision-making process as they navigate the intricate terrain of ASD surgical interventions.
Keyword
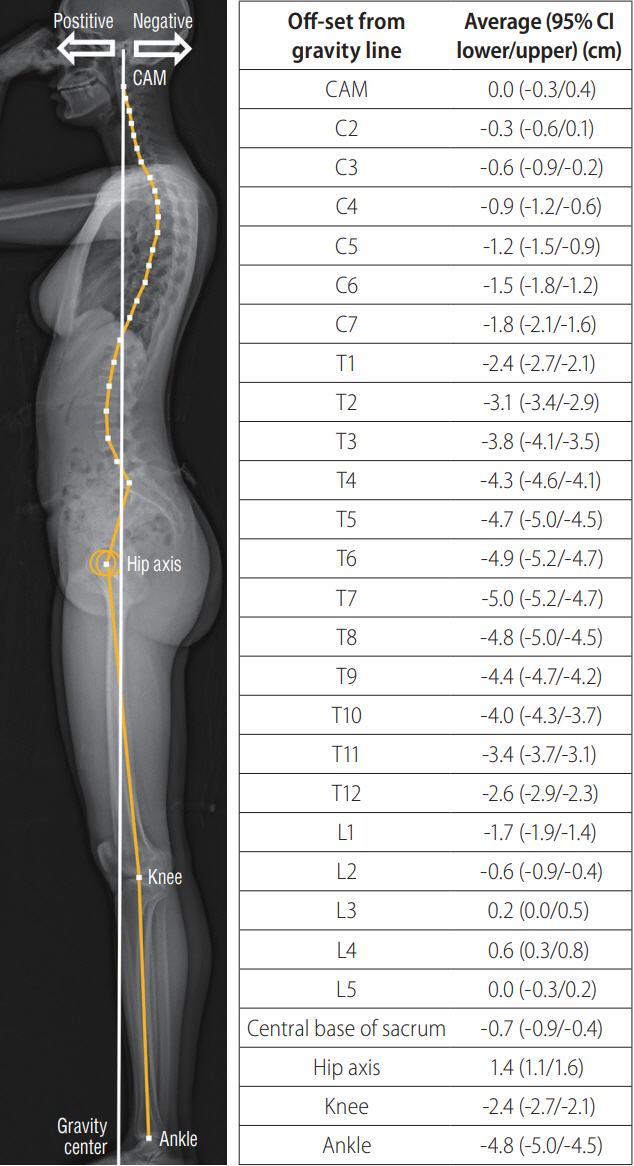
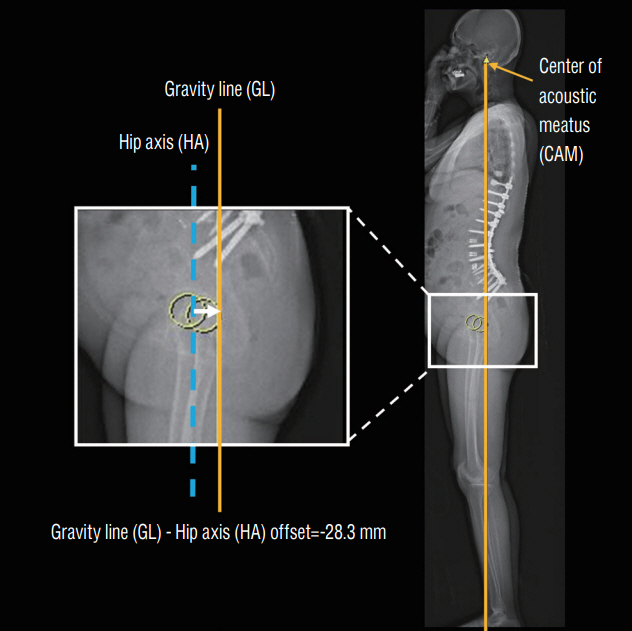
Figure
Reference
-
References
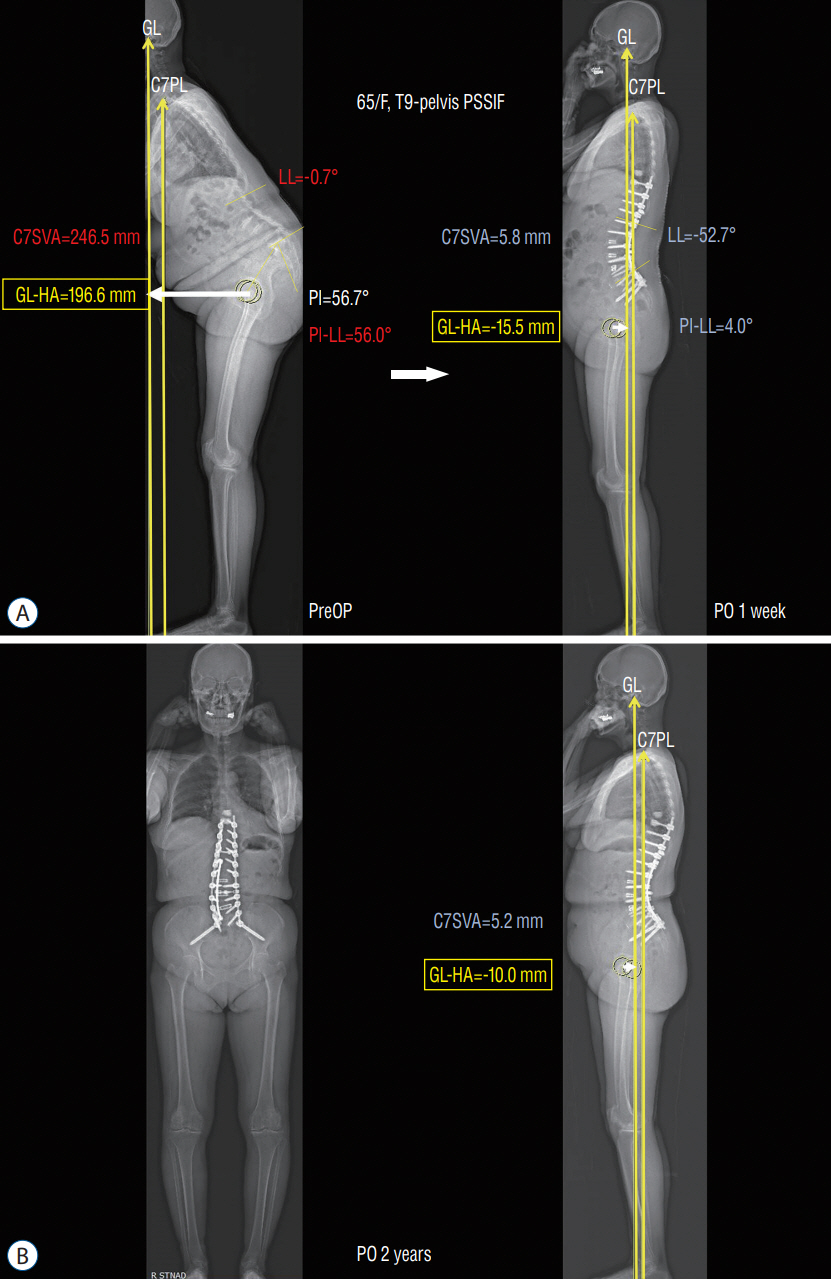
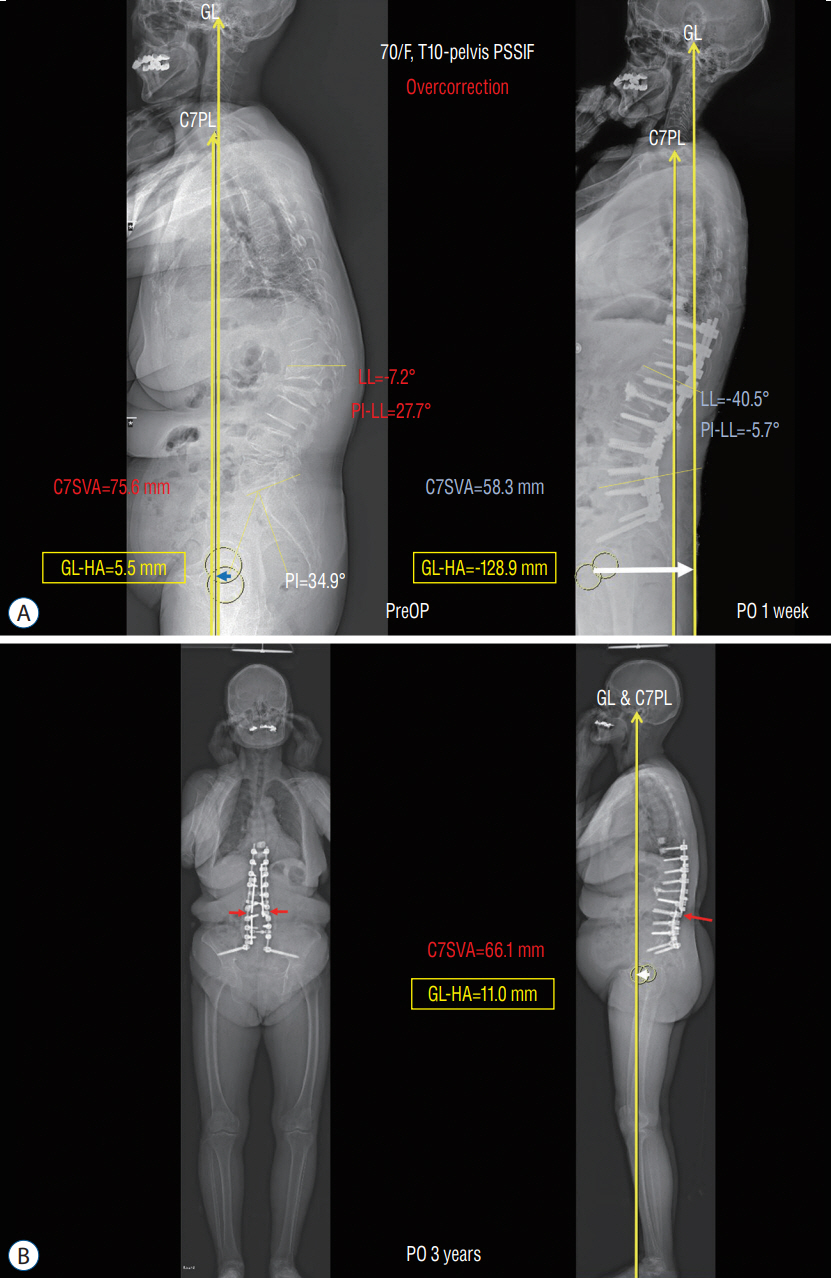
1. An S, Hyun SJ, Lee JK, Yang SH, Kim KJ. Postoperative gravity line-hip axis offset as a substantial risk factor for mechanical failure after adult spinal deformity correction surgery. Neurosurgery. 92:998–1005. 2023.2. Bari TJ, Ohrt-Nissen S, Hansen LV, Dahl B, Gehrchen M. Ability of the global alignment and proportion score to predict mechanical failure following adult spinal deformity surgery-validation in 149 patients with two-year follow-up. Spine deform. 7:331–337. 2019.3. Barrey C, Roussouly P, Le Huec JC, D’Acunzi G, Perrin G. Compensatory mechanisms contributing to keep the sagittal balance of the spine. Eur Spine J 22 Suppl. 6(Suppl 6):S834–S841. 2013.4. Baum GR, Ha AS, Cerpa M, Zuckerman SL, Lin JD, Menger RP, et al. Does the Global Alignment and Proportion score overestimate mechanical complications after adult spinal deformity correction? J Neurosurg Spine. 34:96–102. 2020.5. Charpak G. Prospects for the use in medicine of new detectors of ionizing radiation. Bull Acad Natl Med. 180:161–168. discussion 168. 1996.6. Dubousset J. Three-dimensional analysis of the scoliotic deformity. In : Weinstein SL, editor. The pediatric spine: principles and practice. ed 1. New York: Raven Press;1994. p. 479–496.7. Ferrero E, Liabaud B, Challier V, Lafage R, Diebo BG, Vira S, et al. Role of pelvic translation and lower-extremity compensation to maintain gravity line position in spinal deformity. J Neurosurg Spine. 24:436–446. 2016.8. Garg B, Mehta N, Bansal T, Malhotra R. EOS® imaging: concept and current applications in spinal disorders. J Clin Orthop Trauma. 11:786–793. 2020.9. Glattes RC, Bridwell KH, Lenke LG, Kim YJ, Rinella A, Edwards C 2nd. Proximal junctional kyphosis in adult spinal deformity following long instrumented posterior spinal fusion: incidence, outcomes, and risk factor analysis. Spine (Phila Pa 1976). 30:1643–1649. 2005.10. Ha Y, Maruo K, Racine L, Schairer WW, Hu SS, Deviren V, et al. Proximal junctional kyphosis and clinical outcomes in adult spinal deformity surgery with fusion from the thoracic spine to the sacrum: a comparison of proximal and distal upper instrumented vertebrae. J Neurosurg Spine. 19:360–369. 2013.11. Hasegawa K, Okamoto M, Hatsushikano S, Shimoda H, Ono M, Homma T, et al. Standing sagittal alignment of the whole axial skeleton with reference to the gravity line in humans. J Anat. 230:619–630. 2017.12. Hasegawa K, Okamoto M, Hatsushikano S, Shimoda H, Ono M, Watanabe K. Normative values of spino-pelvic sagittal alignment, balance, age, and health-related quality of life in a cohort of healthy adult subjects. Eur Spine J. 25:3675–3686. 2016.13. Hyun SJ, Jung JM. Spinal deformity surgery : it becomes an essential part of neurosurgery. J Korean Neurosurg Soc. 61:661–668. 2018.14. Hyun SJ, Kim KJ, Jahng TA. The differential effect of cervical kyphosis correction surgery on global sagittal alignment and health-related quality of life according to head- and trunk-balanced subtype. J Neurosurg Spine. 34:839–848. 2021.15. Hyun SJ, Rhim SC. Clinical outcomes and complications after pedicle subtraction osteotomy for fixed sagittal imbalance patients : a long-term follow-up data. J Korean Neurosurg Soc. 47:95–101. 2010.16. Kim CW, Hyun SJ, Kim KJ. Systematic review of reciprocal changes after spinal reconstruction surgery : do not miss the forest for the trees. J Korean Neurosurg Soc. 64:843–852. 2021.17. Kim KR, Le Huec JC, Jang HJ, Noh SH, Park JY, Ha Y, et al. Which is more predictive value for mechanical complications: fixed thoracolumbar alignment (T1 pelvic angle) versus dynamic global balance parameter (odontoid-hip axis angle). Neurospine. 18:597–607. 2021.18. Kim YC, Lenke LG, Lee SJ, Gum JL, Wilartratsami S, Blanke KM. The cranial sagittal vertical axis (CrSVA) is a better radiographic measure to predict clinical outcomes in adult spinal deformity surgery than the C7 SVA: a monocentric study. Eur Spine J. 26:2167–2175. 2017.19. Kim YJ, Bridwell KH, Lenke LG, Glattes CR, Rhim S, Cheh G. Proximal junctional kyphosis in adult spinal deformity after segmental posterior spinal instrumentation and fusion: minimum five-year follow-up. Spine (Phila Pa 1976). 33:2179–2184. 2008.20. Lafage V, Schwab F, Patel A, Hawkinson N, Farcy JP. Pelvic tilt and truncal inclination: two key radiographic parameters in the setting of adults with spinal deformity. Spine (Phila Pa 1976). 34:E599–E606. 2009.21. Le Huec JC, Hasegawa K. Normative values for the spine shape parameters using 3D standing analysis from a database of 268 asymptomatic Caucasian and Japanese subjects. Eur Spine J. 25:3630–3637. 2016.22. Le Huec JC, Saddiki R, Franke J, Rigal J, Aunoble S. Equilibrium of the human body and the gravity line: the basics. Eur Spine J 20 Suppl. 5(Suppl 5):558–563. 2011.23. Le Huec JC, Thompson W, Mohsinaly Y, Barrey C, Faundez A. Sagittal balance of the spine. Eur Spine J. 28:1889–1905. 2019.24. Lee JH, Kim JU, Jang JS, Lee SH. Analysis of the incidence and risk factors for the progression of proximal junctional kyphosis following surgical treatment for lumbar degenerative kyphosis: minimum 2-year follow-up. Br J Neurosurg. 28:252–258. 2014.25. Lee JK, Hyun SJ, Kim KJ. Reciprocal changes in the whole-body following realignment surgery in adult spinal deformity. Asian Spine J. 16:958–967. 2022.26. Lee JK, Hyun SJ, Yang SH, Kim KJ. Reciprocal changes following cervical realignment surgery. Neurospine. 19:853–861. 2022.27. Marks M, Stanford C, Newton P. Which lateral radiographic positioning technique provides the most reliable and functional representation of a patient’s sagittal balance? Spine (Phila Pa 1976). 34:949–954. 2009.28. Marks MC, Stanford CF, Mahar AT, Newton PO. Standing lateral radiographic positioning does not represent customary standing balance. Spine (Phila Pa 1976). 28:1176–1182. 2003.29. Maruo K, Ha Y, Inoue S, Samuel S, Okada E, Hu SS, et al. Predictive factors for proximal junctional kyphosis in long fusions to the sacrum in adult spinal deformity. Spine (Phila Pa 1976). 38:E1469–E1476. 2013.30. Melhem E, Assi A, El Rachkidi R, Ghanem I. EOS® biplanar X-ray imaging: concept, developments, benefits, and limitations. J Child Orthop. 10:1–14. 2016.31. Mendoza-Lattes S, Ries Z, Gao Y, Weinstein SL. Proximal junctional kyphosis in adult reconstructive spine surgery results from incomplete restoration of the lumbar lordosis relative to the magnitude of the thoracic kyphosis. Iowa Orthop J. 31:199–206. 2011.32. Mohanty S, Lai C, Mikhail C, Greisberg G, Hassan FM, Stephan SR, et al. Outcomes and reoperation rates of adult spinal deformity patients with baseline sagittal malalignment based on the cranial axis to the hip at 2 years postoperatively. J Neurosurg Spine. 39:301–310. 2023.33. Noh SH, Ha Y, Obeid I, Park JY, Kuh SU, Chin DK, et al. Modified global alignment and proportion scoring with body mass index and bone mineral density (GAPB) for improving predictions of mechanical complications after adult spinal deformity surgery. Spine J. 20:776–784. 2020.34. Roussouly P, Gollogly S, Noseda O, Berthonnaud E, Dimnet J. The vertical projection of the sum of the ground reactive forces of a standing patient is not the same as the C7 plumb line: a radiographic study of the sagittal alignment of 153 asymptomatic volunteers. Spine (Phila Pa 1976). 31:E320–E325. 2006.35. Roussouly P, Pinheiro-Franco JL. Biomechanical analysis of the spinopelvic organization and adaptation in pathology. Eur Spine J 20 Suppl. 5(Suppl 5):609–618. 2011.36. Schwab F, Lafage V, Boyce R, Skalli W, Farcy JP. Gravity line analysis in adult volunteers: age-related correlation with spinal parameters, pelvic parameters, and foot position. Spine (Phila Pa 1976). 31:E959–E967. 2006.37. Schwab F, Ungar B, Blondel B, Buchowski J, Coe J, Deinlein D, et al. Scoliosis Research Society-Schwab adult spinal deformity classification: a validation study. Spine (Phila Pa 1976). 37:1077–1082. 2012.38. Soroceanu A, Diebo BG, Burton D, Smith JS, Deviren V, Shaffrey C, et al. Radiographical and implant-related complications in adult spinal deformity surgery: incidence, patient risk factors, and impact on health-related quality of life. Spine (Phila Pa 1976). 40:1414–1421. 2015.39. Vernazza S, Alexandrov A, Massion J. Is the center of gravity controlled during upper trunk movements? Neurosci Lett. 206:77–80. 1996.40. Yagi M, Akilah KB, Boachie-Adjei O. Incidence, risk factors and classification of proximal junctional kyphosis: surgical outcomes review of adult idiopathic scoliosis. Spine (Phila Pa 1976). 36:E60–E68. 2011.41. Yagi M, Daimon K, Hosogane N, Okada E, Suzuki S, Tsuji O, et al. Predictive probability of the global alignment and proportion score for the development of mechanical failure following adult spinal deformity surgery in Asian patients. Spine (Phila Pa 1976). 46:E80–E86. 2021.42. Yagi M, King AB, Boachie-Adjei O. Incidence, risk factors, and natural course of proximal junctional kyphosis: surgical outcomes review of adult idiopathic scoliosis. Minimum 5 years of follow-up. Spine (Phila Pa 1976). 37:1479–1489. 2012.43. Yagi M, Takeda K, Machida M, Asazuma T. Discordance of gravity line and C7PL in patient with adult spinal deformity--factors affecting the occiput-trunk sagittal discordance. Spine J. 15:213–221. 2015.44. Yilgor C, Sogunmez N, Boissiere L, Yavuz Y, Obeid I, Kleinstück F, et al. Global Alignment and Proportion (GAP) score: development and validation of a new method of analyzing spinopelvic alignment to predict mechanical complications after adult spinal deformity surgery. J Bone Joint Surg Am. 99:1661–1672. 2017.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Reliability of the Sundsvall Method for Femoral Offset Evaluation
- Concepts and Techniques to Prevent Cervical Spine Deformity After Spine Surgery: A Narrative Review
- Minimally Invasive Spinal Surgery for Adult Spinal Deformity
- Radiological Evaluation and Classification of Adult Spinal Deformity
- Roentgenographic Study on Shape and Size of the Femoral Head of Normal Korean Adults