Diabetes Metab J.
2024 May;48(3):463-472. 10.4093/dmj.2023.0310.
2023 Diabetic Kidney Disease Fact Sheet in Korea
- Affiliations
-
- 1Department of Internal Medicine, Korea University College of Medicine, Seoul, Korea
- 2Department of Internal Medicine, Soonchunhyang University Gumi Hospital, Soonchunhyang University College of Medicine, Gumi, Korea
- 3Samsung Biomedical Research Institute, Sungkyunkwan University School of Medicine, Suwon, Korea
- 4Department of Statistics and Actuarial Science, Soongsil University, Seoul, Korea
- 5Department of Internal Medicine, Keimyung University School of Medicine, Daegu, Korea
- KMID: 2555777
- DOI: http://doi.org/10.4093/dmj.2023.0310
Abstract
- Background
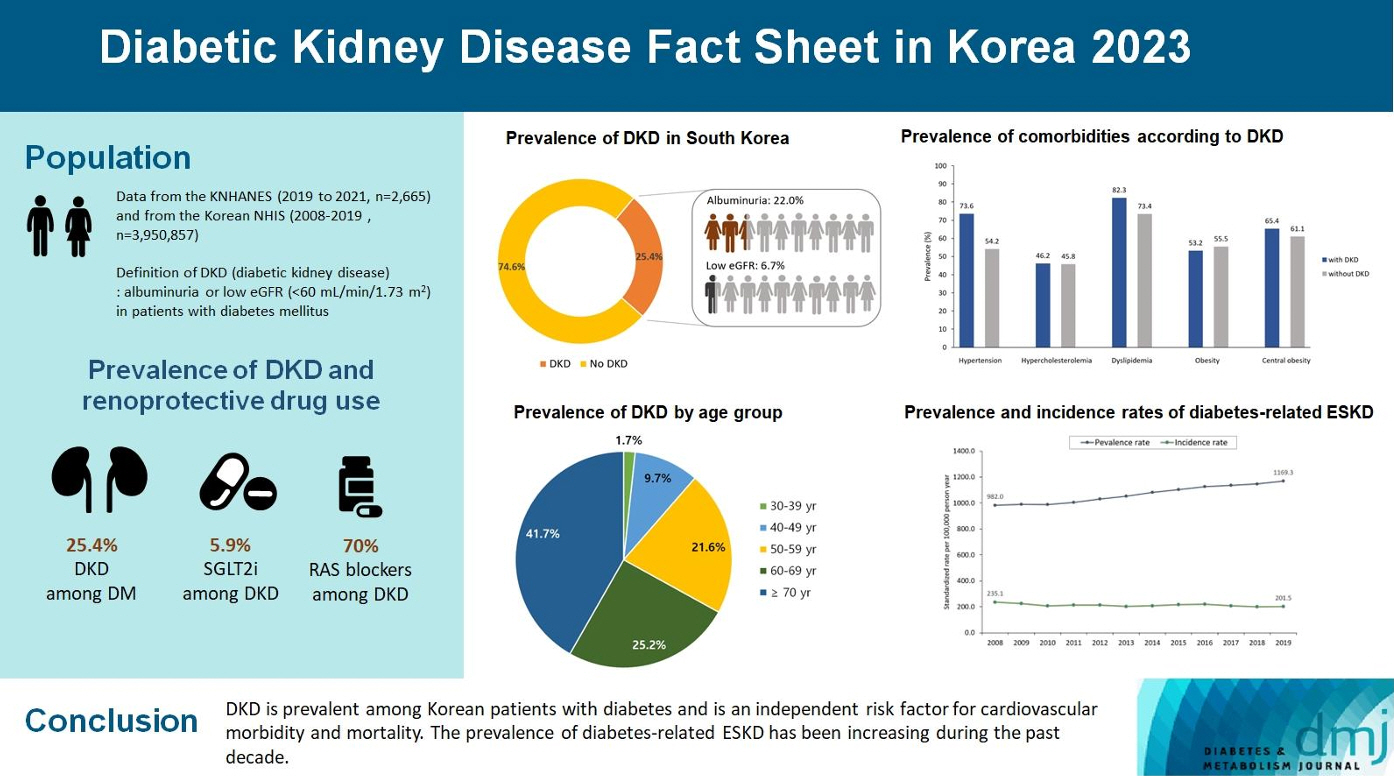
To investigate the prevalence, incidence, comorbidities, and management status of diabetic kidney disease (DKD) and diabetes-related end-stage kidney disease (ESKD) in South Korea.
Methods
We used the Korea National Health and Nutrition Examination Survey data (2019 to 2021, n=2,665) for the evaluation of prevalence, comorbidities, control rate of glycemia and comorbidities in DKD, and the Korean Health Insurance Service-customized database (2008 to 2019, n=3,950,857) for the evaluation of trends in the incidence and prevalence rate of diabetes-related ESKD, renin-angiotensin system (RAS) blockers and sodium glucose cotransporter 2 (SGLT2) inhibitors use for DKD, and the risk of atherosclerotic cardiovascular disease (ASCVD) and mortality according to DKD stages. DKD was defined as albuminuria or low estimated glomerular filtration rate (eGFR) <60 mL/min/1.73 m2 in patients with diabetes mellitus.
Results
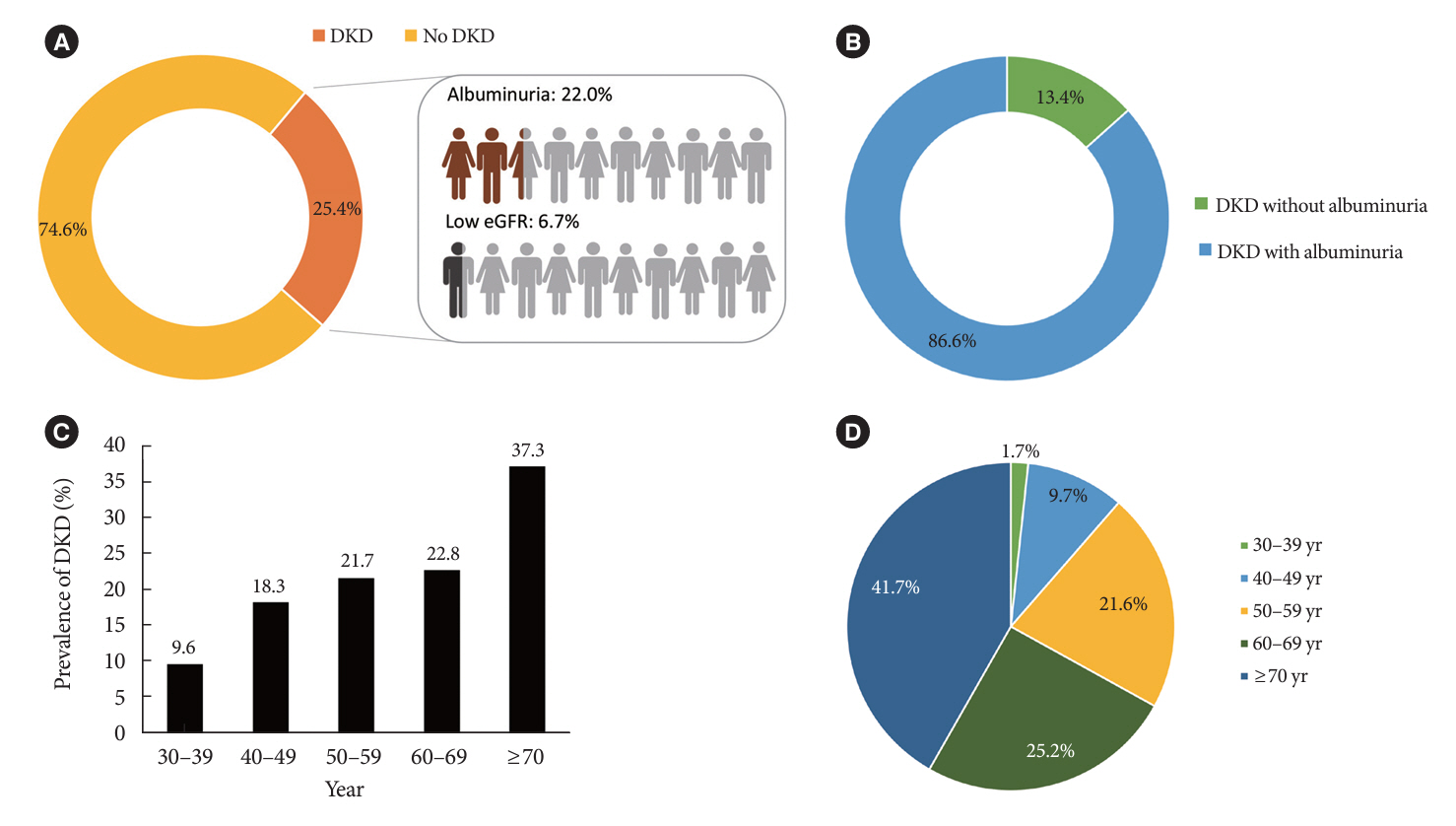
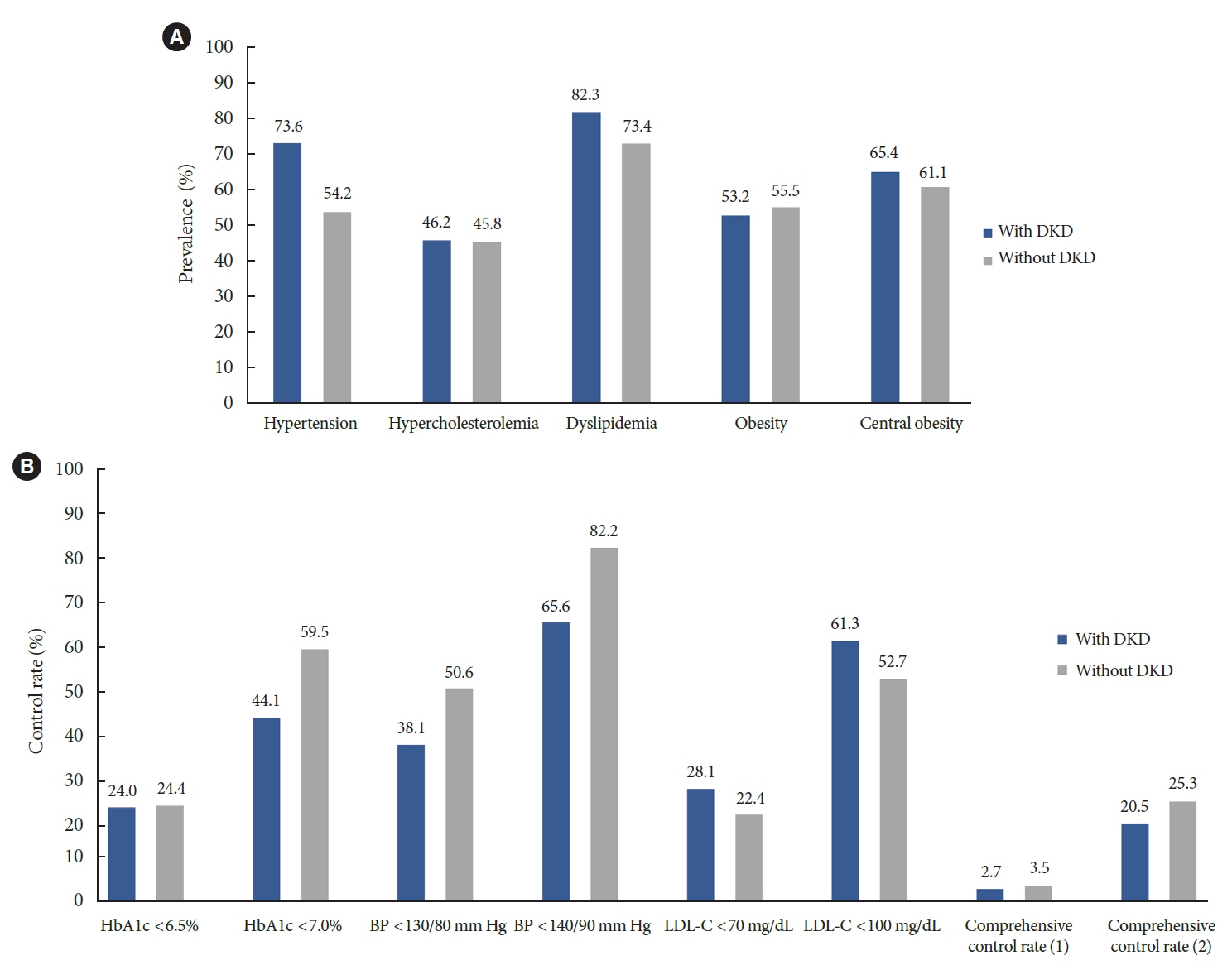
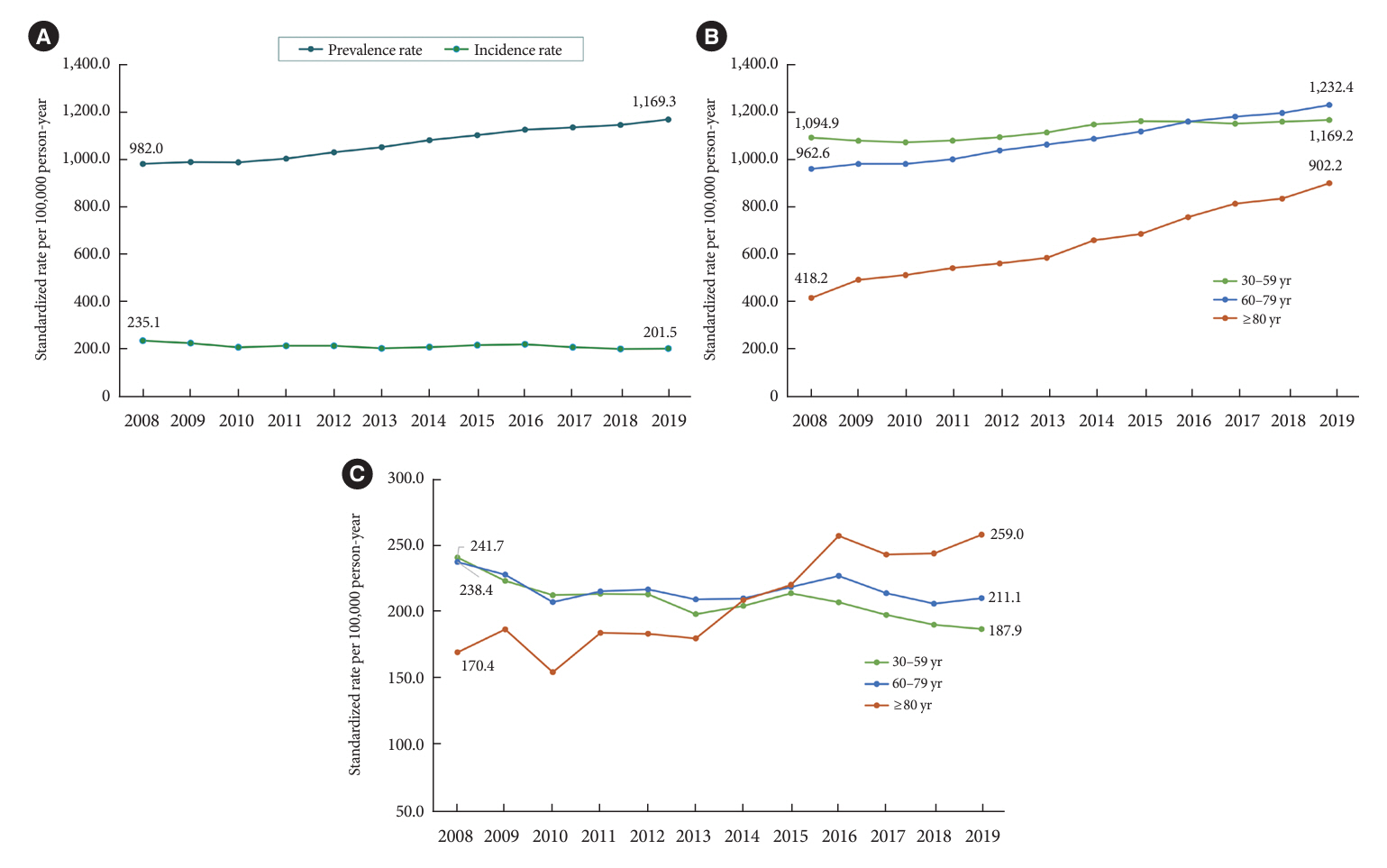
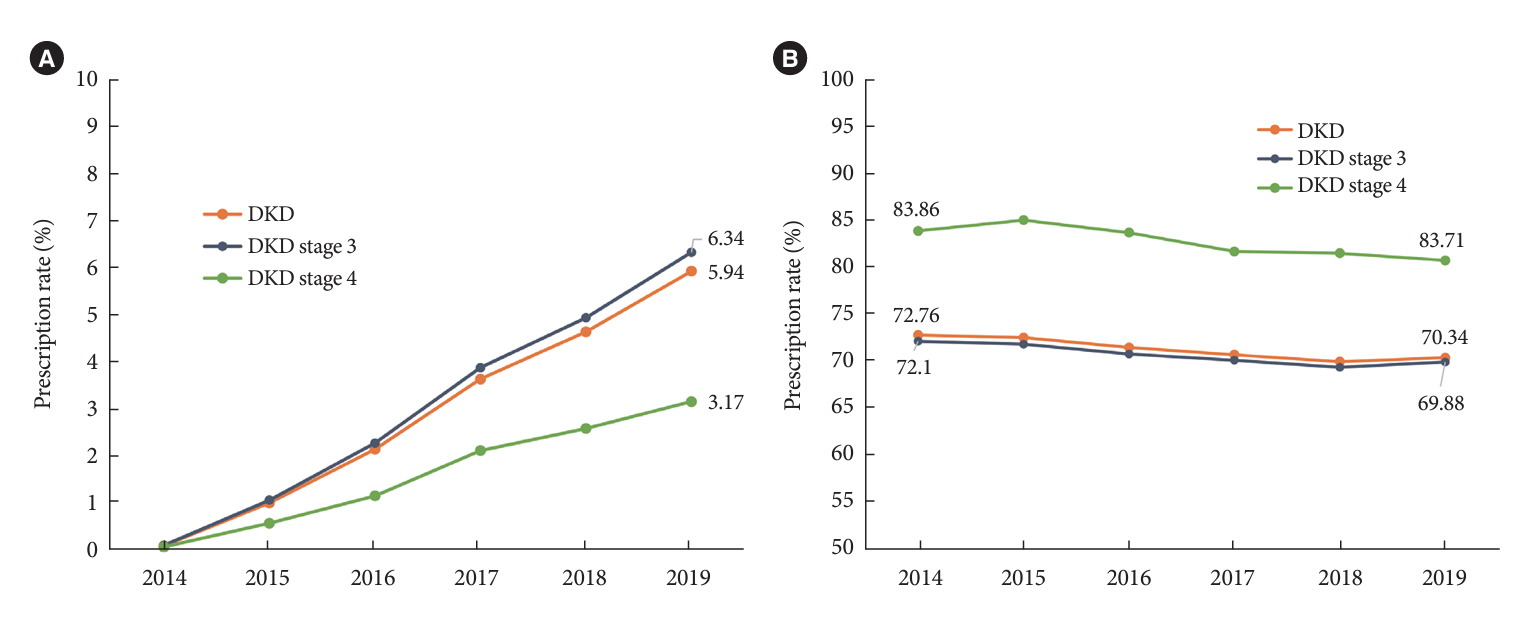
The prevalence of DKD was 25.4% (albuminuria, 22.0%; low eGFR, 6.73%) in patients with diabetes mellitus aged ≥30 years. Patients with DKD had a higher rate of comorbidities, including hypertension, dyslipidemia, and central obesity; however, their control rates were lower than those without DKD. Prescription rate of SGLT2 inhibitors with reduced eGFR increased steadily, reaching 5.94% in 2019. Approximately 70% of DKD patients were treated with RAS blockers. The prevalence rate of diabetesrelated ESKD has been steadily increasing, with a higher rate in older adults. ASCVD and mortality were significantly associated with an in increase in DKD stage.
Conclusion
DKD is prevalent among Korean patients with diabetes and is an independent risk factor for cardiovascular morbidity and mortality, which requiring intensive management of diabetes and comorbidities. The prevalence of diabetes-related ESKD has been increasing, especially in the older adults, during past decade.
Figure
Reference
-
1. Thomas MC, Brownlee M, Susztak K, Sharma K, Jandeleit-Dahm KA, Zoungas S, et al. Diabetic kidney disease. Nat Rev Dis Primers. 2015; 1:15018.
Article2. Koye DN, Magliano DJ, Nelson RG, Pavkov ME. The global epidemiology of diabetes and kidney disease. Adv Chronic Kidney Dis. 2018; 25:121–32.
Article3. Mogensen CE, Christensen CK, Vittinghus E. The stages in diabetic renal disease: with emphasis on the stage of incipient diabetic nephropathy. Diabetes. 1983; 32 Suppl 2:64–78.
Article4. Thomas MC, Macisaac RJ, Jerums G, Weekes A, Moran J, Shaw JE, et al. Nonalbuminuric renal impairment in type 2 diabetic patients and in the general population (national evaluation of the frequency of renal impairment cO-existing with NIDDM [NEFRON] 11). Diabetes Care. 2009; 32:1497–502.
Article5. Retnakaran R, Cull CA, Thorne KI, Adler AI, Holman RR; UKPDS Study Group. Risk factors for renal dysfunction in type 2 diabetes: U.K. Prospective Diabetes Study 74. Diabetes. 2006; 55:1832–9.6. Ninomiya T, Perkovic V, de Galan BE, Zoungas S, Pillai A, Jardine M, et al. Albuminuria and kidney function independently predict cardiovascular and renal outcomes in diabetes. J Am Soc Nephrol. 2009; 20:1813–21.
Article7. Levey AS, Grams ME, Inker LA. Uses of GFR and albuminuria level in acute and chronic kidney disease. N Engl J Med. 2022; 386:2120–8.
Article8. Persson F, Rossing P. Diagnosis of diabetic kidney disease: state of the art and future perspective. Kidney Int Suppl (2011). 2018; 8:2–7.
Article9. Afkarian M, Zelnick LR, Hall YN, Heagerty PJ, Tuttle K, Weiss NS, et al. Clinical manifestations of kidney disease among US adults with diabetes, 1988-2014. JAMA. 2016; 316:602–10.
Article10. Guo K, Zhang L, Zhao F, Lu J, Pan P, Yu H, et al. Prevalence of chronic kidney disease and associated factors in Chinese individuals with type 2 diabetes: cross-sectional study. J Diabetes Complications. 2016; 30:803–10.
Article11. Yang CW, Park JT, Kim YS, Kim YL, Lee YS, Oh YS, et al. Prevalence of diabetic nephropathy in primary care type 2 diabetic patients with hypertension: data from the Korean Epidemiology Study on Hypertension III (KEY III study). Nephrol Dial Transplant. 2011; 26:3249–55.
Article12. Ahn JH, Yu JH, Ko SH, Kwon HS, Kim DJ, Kim JH, et al. Prevalence and determinants of diabetic nephropathy in Korea: Korea National Health and Nutrition Examination Survey. Diabetes Metab J. 2014; 38:109–19.
Article13. Palsson R, Patel UD. Cardiovascular complications of diabetic kidney disease. Adv Chronic Kidney Dis. 2014; 21:273–80.
Article14. Sasso FC, De Nicola L, Carbonara O, Nasti R, Minutolo R, Salvatore T, et al. Cardiovascular risk factors and disease management in type 2 diabetic patients with diabetic nephropathy. Diabetes Care. 2006; 29:498–503.
Article15. Hur KY, Moon MK, Park JS, Kim SK, Lee SH, Yun JS, et al. 2021 Clinical practice guidelines for diabetes mellitus of the Korean Diabetes Association. Diabetes Metab J. 2021; 45:461–81.
Article16. ElSayed NA, Aleppo G, Aroda VR, Bannuru RR, Brown FM, Bruemmer D, et al. 11. Chronic kidney disease and risk management: standards of care in diabetes-2023. Diabetes Care. 2023; 46(Suppl 1):S191–202.17. Neumiller JJ, Alicic RZ, Tuttle KR. Overcoming barriers to implementing new therapies for diabetic kidney disease: lessons learned. Adv Chronic Kidney Dis. 2021; 28:318–27.
Article18. Yildirim T, Arici M, Piskinpasa S, Aybal-Kutlugun A, Yilmaz R, Altun B, et al. Major barriers against renin-angiotensin-aldosterone system blocker use in chronic kidney disease stages 3-5 in clinical practice: a safety concern? Ren Fail. 2012; 34:1095–9.
Article19. Garcia-Donaire JA, Ruilope LM. Cardiovascular and renal links along the cardiorenal continuum. Int J Nephrol. 2011; 2011:975782.20. Kweon S, Kim Y, Jang MJ, Kim Y, Kim K, Choi S, et al. Data resource profile: the Korea National Health and Nutrition Examination Survey (KNHANES). Int J Epidemiol. 2014; 43:69–77.
Article21. Lee J, Lee JS, Park SH, Shin SA, Kim K. Cohort profile: the National Health Insurance Service-National Sample Cohort (NHIS-NSC), South Korea. Int J Epidemiol. 2017; 46:e15.
Article22. Kyoung DS, Kim HS. Understanding and utilizing claim data from the Korean National Health Insurance Service (NHIS) and Health Insurance Review & Assessment (HIRA) database for research. J Lipid Atheroscler. 2022; 11:103–10.
Article23. Michels WM, Grootendorst DC, Verduijn M, Elliott EG, Dekker FW, Krediet RT. Performance of the Cockcroft-Gault, MDRD, and new CKD-EPI formulas in relation to GFR, age, and body size. Clin J Am Soc Nephrol. 2010; 5:1003–9.
Article24. Ko SH, Han K, Lee YH, Noh J, Park CY, Kim DJ, et al. Past and current status of adult type 2 diabetes mellitus management in Korea: a National Health Insurance Service database analysis. Diabetes Metab J. 2018; 42:93–100.
Article25. Afkarian M, Sachs MC, Kestenbaum B, Hirsch IB, Tuttle KR, Himmelfarb J, et al. Kidney disease and increased mortality risk in type 2 diabetes. J Am Soc Nephrol. 2013; 24:302–8.
Article26. Penno G, Solini A, Bonora E, Fondelli C, Orsi E, Zerbini G, et al. HbA1c variability as an independent correlate of nephropathy, but not retinopathy, in patients with type 2 diabetes: the Renal Insufficiency And Cardiovascular Events (RIACE) Italian multicenter study. Diabetes Care. 2013; 36:2301–10.27. Kume S, Araki SI, Ugi S, Morino K, Koya D, Nishio Y, et al. Secular changes in clinical manifestations of kidney disease among Japanese adults with type 2 diabetes from 1996 to 2014. J Diabetes Investig. 2019; 10:1032–40.28. Yang YS, Kim HL, Kim SH, Moon MK; Committee of Clinical Practice Guideline; Korean Diabetes Association and Clinical Practice Guideline Committee; Korean Society of Lipid and Atherosclerosis. Lipid management in Korean people with type 2 diabetes mellitus: Korean Diabetes Association and Korean Society of Lipid and Atherosclerosis consensus statement. J Lipid Atheroscler. 2023; 12:12–22.
Article29. Bauer F, Seibert FS, Rohn B, Babel N, Westhoff TH. Estimation of LDL cholesterol in chronic kidney disease. Eur J Prev Cardiol. 2021; 28:1402–8.
Article30. Kalantar-Zadeh K, Jafar TH, Nitsch D, Neuen BL, Perkovic V. Chronic kidney disease. Lancet. 2021; 398:786–802.
Article31. Lee MJ, Ha KH, Kim DJ, Park I. Trends in the incidence, prevalence, and mortality of end-stage kidney disease in South Korea. Diabetes Metab J. 2020; 44:933–7.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Diagnosis and test for diabetic kidney disease
- Fact Sheet on Cardiac Rehabilitation for Cardiovascular Disease in South Korea
- Prevalence and Current Management of Cardiovascular Risk Factors in Korean Adults Based on Fact Sheets
- Synopsis of the Korean Society of Nephrology 2023 Practical Recommendations for the Management of Diabetic Kidney Disease
- 2021 Korean Diabetes Association Clinical Practice Guidelines for Diabetes: Diabetic Kidney Disease