Insulin Resistance, Non-Alcoholic Fatty Liver Disease and Type 2 Diabetes Mellitus: Clinical and Experimental Perspective
- Affiliations
-
- 1Division of Endocrinology and Metabolism, Department of Internal Medicine, Korea University Ansan Hospital, Korea University College of Medicine, Ansan, Korea
- 2Division of Endocrinology and Metabolism, Department of Internal Medicine, Changwon Fatima Hospital, Changwon, Korea
- 3Division of Endocrinology and Metabolism, Department of Internal Medicine, Kangbuk Samsung Hospital, Sungkyunkwan University School of Medicine, Seoul, Korea
- KMID: 2555765
- DOI: http://doi.org/10.4093/dmj.2023.0350
Abstract
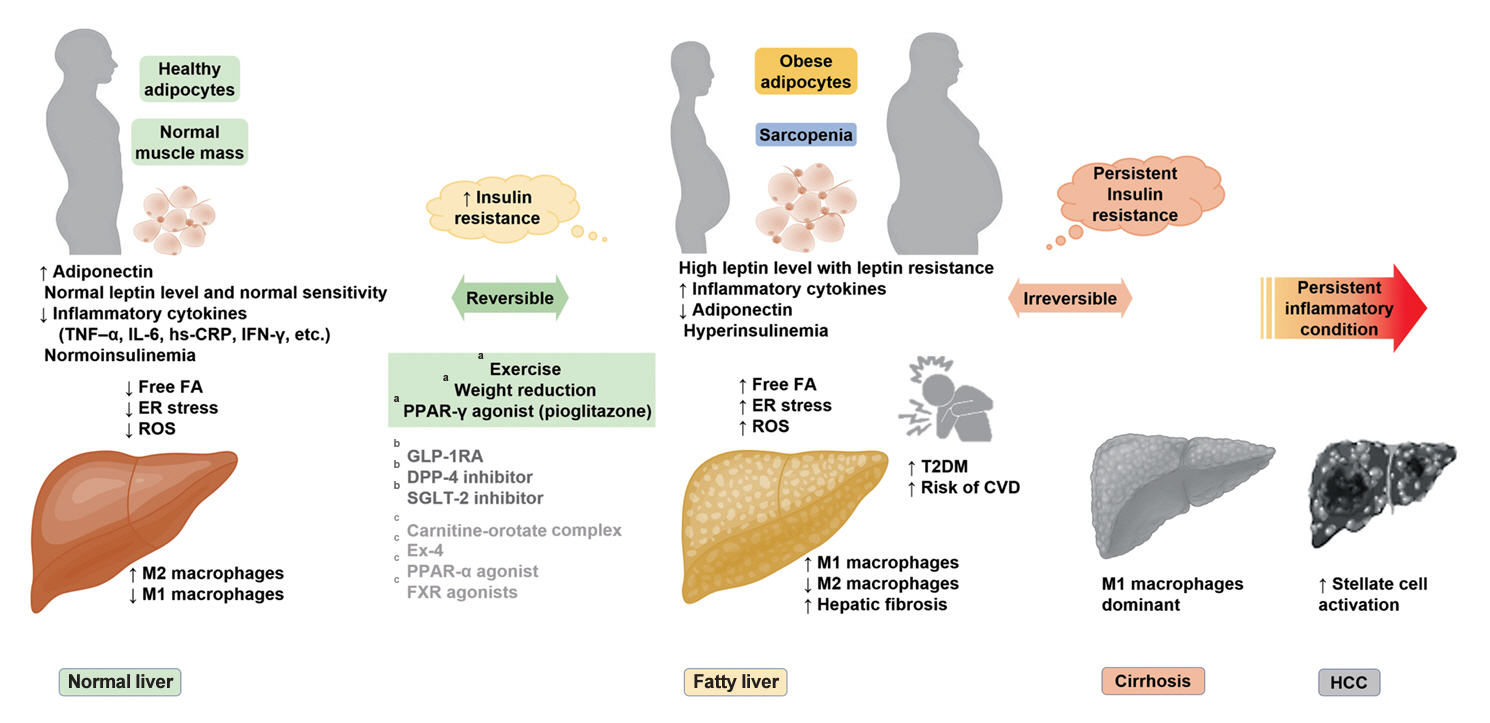
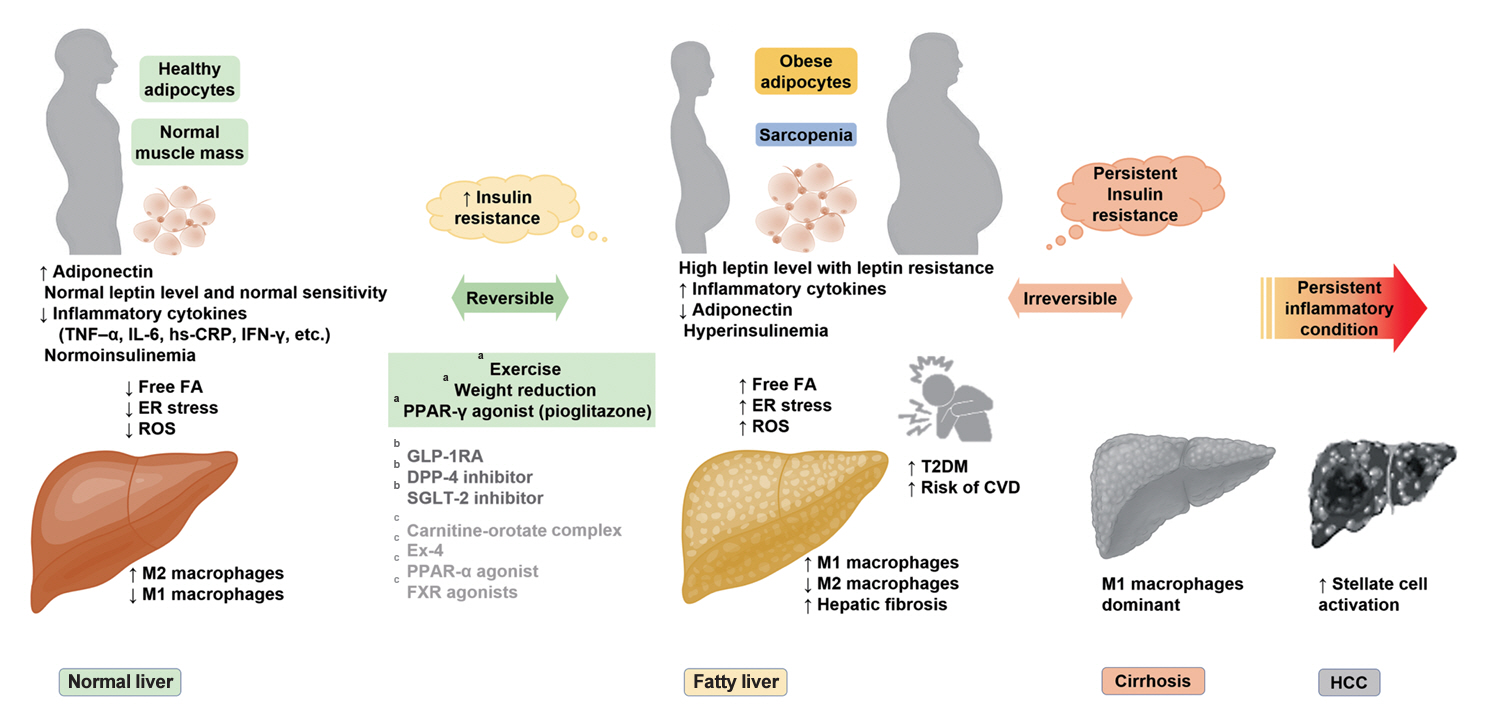
- It has been generally accepted that insulin resistance (IR) and reduced insulin secretory capacity are the basic pathogenesis of type 2 diabetes mellitus (T2DM). In addition to genetic factors, the persistence of systemic inflammation caused by obesity and the associated threat of lipotoxicity increase the risk of T2DM. In particular, the main cause of IR is obesity and subjects with T2DM have a higher body mass index (BMI) than normal subjects according to recent studies. The prevalence of T2DM with IR has increased with increasing BMI during the past three decades. According to recent studies, homeostatic model assessment of IR was increased compared to that of the 1990s. Rising prevalence of obesity in Korea have contributed to the development of IR, non-alcoholic fatty liver disease and T2DM and cutting this vicious cycle is important. My colleagues and I have investigated this pathogenic mechanism on this theme through clinical and experimental studies over 20 years and herein, I would like to summarize some of our studies with deep gratitude for receiving the prestigious 2023 Sulwon Award.
Figure
Cited by 3 articles
-
Metabolic Dysfunction-Associated Steatotic Liver Disease in Type 2 Diabetes Mellitus: A Review and Position Statement of the Fatty Liver Research Group of the Korean Diabetes Association
Jaehyun Bae, Eugene Han, Hye Won Lee, Cheol-Young Park, Choon Hee Chung, Dae Ho Lee, Eun-Hee Cho, Eun-Jung Rhee, Ji Hee Yu, Ji Hyun Park, Ji-Cheol Bae, Jung Hwan Park, Kyung Mook Choi, Kyung-Soo Kim, Mi Hae Seo, Minyoung Lee, Nan-Hee Kim, So Hun Kim, Won-Young Lee, Woo Je Lee, Yeon-Kyung Choi, Yong-ho Lee, You-Cheol Hwang, Young Sang Lyu, Byung-Wan Lee, Bong-Soo Cha
Diabetes Metab J. 2024;48(6):1015-1028. doi: 10.4093/dmj.2024.0541.Comparison of SPISE and METS-IR and Other Markers to Predict Insulin Resistance and Elevated Liver Transaminases in Children and Adolescents
Kyungchul Song, Eunju Lee, Hye Sun Lee, Hana Lee, Ji-Won Lee, Hyun Wook Chae, Yu-Jin Kwon
Diabetes Metab J. 2025;49(2):264-274. doi: 10.4093/dmj.2024.0302.Extracellular Vesicle-Mediated Network in the Pathogenesis of Obesity, Diabetes, Steatotic Liver Disease, and Cardiovascular Disease
Joonyub Lee, Won Gun Choi, Marie Rhee, Seung-Hwan Lee
Diabetes Metab J. 2025;49(3):348-367. doi: 10.4093/dmj.2025.0184.
Reference
-
1. Defronzo RA. Banting lecture. From the triumvirate to the ominous octet: a new paradigm for the treatment of type 2 diabetes mellitus. Diabetes. 2009; 58:773–95.2. Park SW, Yun YS, Song YD, Lee HC, Huh KB. Pathogenetic heterogeneity of type 2 diabetes mellitus in Korea. J Korean Diabetes Assoc. 1999; 23:62–9.3. Yoon KH. Pathogenesis of type 2 diabetes in Korea. Korean Diabetes J. 2000; 24:397–403.4. Yang YS, Han BD, Han K, Jung JH, Son JW; Taskforce Team of the Obesity Fact Sheet of the Korean Society for the Study of Obesity. Obesity fact sheet in Korea, 2021: trends in obesity prevalence and obesity-related comorbidity incidence stratified by age from 2009 to 2019. J Obes Metab Syndr. 2022; 31:169–77.
Article5. Son JW, Park CY, Kim S, Lee HK, Lee YS; Insulin Resistance as Primary Pathogenesis in Newly Diagnosed, Drug Naïve Type 2 Diabetes Patients in Korea (SURPRISE) Study Group. Changing clinical characteristics according to insulin resistance and insulin secretion in newly diagnosed type 2 diabetic patients in Korea. Diabetes Metab J. 2015; 39:387–94.
Article6. Kim JD, Lee WY. Insulin secretory capacity and insulin resistance in Korean type 2 diabetes mellitus patients. Endocrinol Metab (Seoul). 2016; 31:354–60.
Article7. Han E, Han KD, Lee YH, Kim KS, Hong S, Park JH, et al. Fatty liver & diabetes statistics in Korea: nationwide data 2009 to 2017. Diabetes Metab J. 2023; 47:347–55.
Article8. Rhee EJ, Park SE, Chang Y, Ryu S, Lee WY. Baseline glycemic status and mortality in 241,499 Korean metropolitan subjects: a Kangbuk Samsung Health Study. Metabolism. 2016; 65:68–77.
Article9. Eslam M, Sanyal AJ, George J; International Consensus Panel. MAFLD: a consensus-driven proposed nomenclature for metabolic associated fatty liver disease. Gastroenterology. 2020; 158:1999–2014.
Article10. Koo DJ, Lee WY. The crosstalk between insulin resistance and nonalcoholic fatty liver disease/metabolic dysfunction-associated fatty liver disease: a culprit or a consequence? Cardiovasc Prev Pharmacother. 2022; 4:132–41.
Article11. Targher G, Day CP, Bonora E. Risk of cardiovascular disease in patients with nonalcoholic fatty liver disease. N Engl J Med. 2010; 363:1341–50.
Article12. Bhatia LS, Curzen NP, Calder PC, Byrne CD. Non-alcoholic fatty liver disease: a new and important cardiovascular risk factor? Eur Heart J. 2012; 33:1190–200.
Article13. Yang HK, Lee JH, Choi IY, Kwon HS, Shin JA, Jeong SH, et al. The insulin resistance but not the insulin secretion parameters have changed in the Korean population during the last decade. Diabetes Metab J. 2015; 39:117–25.
Article14. Cho JK, Kim HM, Lim SK, Whang Y, Lee HC, Huh KB. A study on change of body weight non-insulin dependent diabetes mellitus. J Korean Diabetes Assoc. 1986; 10:89–93.15. Park YS, Shin CS, Kim YS, Kim SY, Cho BY, Lee HK, et al. The etiologic heterogenecity of diabetes mellitus in Korean adults. Korean J Intern Med. 1991; 40:91–103.16. Song TH, Choi BR, Tak SM, Kang JW, Kim CE, Moon FC, et al. A retrospective study on body weight of diabetes in Korea. J Korean Diabetes Assoc. 1990; 14:229–33.17. Lee KU, Ryu JS, Kim YT, Shong YK, Kim GS, Lee M, et al. Clinical characteristics of Korean diabetic patients classified by fasting plasma C-peptide level and degree of obesity. Korean J Intern Med. 1992; 42:315–21.18. Park JY, Kim HK, Kim MS, Park KS, Kim SY, Cho BY, et al. Body weight changes of non-insulin dependent diabetic patients in Korea. J Korean Diabetes Assoc. 1993; 17:51–8.19. Shin CS, Lee HK, Koh CS, Kim YI, Shin YS, Yoo KY, et al. Risk factors for the development of NIDDM in Yonchon County, Korea. Diabetes Care. 1997; 20:1842–6.
Article20. Lee TH. Prevalence of obesity in Korean non-insulin-dependent diabetic patients. Diabetes Res Clin Pract. 1996; 32:71–80.
Article21. Park JY, Lee KU, Kim CH, Kim HK, Hong SK, Park KS, et al. Past and current obesity in Koreans with non-insulin-dependent diabetes mellitus. Diabetes Res Clin Pract. 1997; 35:49–56.
Article22. Kim DJ, Hahm JR, Jeong IK, Yang TY, Oh EY, Choi YH, et al. Insulin secretion and insulin sensitivity in Korean subjects with impaired glucose intolerance. J Korean Diabetes Assoc. 2000; 24:356–64.23. Kim DJ, Song KE, Park JW, Cho HK, Lee KW, Huh KB. Clinical characteristics of Korean type 2 diabetic patients in 2005. Diabetes Res Clin Pract. 2007; 77 Suppl 1:S252–7.
Article24. Yoon KH, Shin JA, Kwon HS, Lee SH, Min KW, Ahn YB, et al. Comparison of the efficacy of glimepiride, metformin, and rosiglitazone monotherapy in Korean drug-naïve type 2 diabetic patients: the practical evidence of antidiabetic monotherapy study. Diabetes Metab J. 2011; 35:26–33.
Article25. Jung CH, Son JW, Kang S, Kim WJ, Kim HS, Kim HS, et al. Diabetes fact sheets in Korea, 2020: an appraisal of current status. Diabetes Metab J. 2021; 45:1–10.
Article26. Ryu S, Sung KC, Chang Y, Lee WY, Rhee EJ. Spectrum of insulin sensitivity in the Korean population. Metabolism. 2005; 54:1644–51.
Article27. Lee DY, Rhee EJ, Chang Y, Sohn CI, Shin HC, Ryu S, et al. Impact of systemic inflammation on the relationship between insulin resistance and all-cause and cancer-related mortality. Metabolism. 2018; 81:52–62.
Article28. Shoelson SE, Herrero L, Naaz A. Obesity, inflammation, and insulin resistance. Gastroenterology. 2007; 132:2169–80.
Article29. Miyazaki Y, Glass L, Triplitt C, Wajcberg E, Mandarino LJ, DeFronzo RA. Abdominal fat distribution and peripheral and hepatic insulin resistance in type 2 diabetes mellitus. Am J Physiol Endocrinol Metab. 2002; 283:E1135–43.
Article30. Cnop M, Landchild MJ, Vidal J, Havel PJ, Knowles NG, Carr DR, et al. The concurrent accumulation of intra-abdominal and subcutaneous fat explains the association between insulin resistance and plasma leptin concentrations: distinct metabolic effects of two fat compartments. Diabetes. 2002; 51:1005–15.31. Cnop M, Havel PJ, Utzschneider KM, Carr DB, Sinha MK, Boyko EJ, et al. Relationship of adiponectin to body fat distribution, insulin sensitivity and plasma lipoproteins: evidence for independent roles of age and sex. Diabetologia. 2003; 46:459–69.
Article32. Bajaj M, Suraamornkul S, Piper P, Hardies LJ, Glass L, Cersosimo E, et al. Decreased plasma adiponectin concentrations are closely related to hepatic fat content and hepatic insulin resistance in pioglitazone-treated type 2 diabetic patients. J Clin Endocrinol Metab. 2004; 89:200–6.
Article33. Dandona P, Aljada A, Bandyopadhyay A. Inflammation: the link between insulin resistance, obesity and diabetes. Trends Immunol. 2004; 25:4–7.
Article34. Hotamisligil GS, Shargill NS, Spiegelman BM. Adipose expression of tumor necrosis factor-alpha: direct role in obesity-linked insulin resistance. Science. 1993; 259:87–91.
Article35. Dandona P, Weinstock R, Thusu K, Abdel-Rahman E, Aljada A, Wadden T. Tumor necrosis factor-alpha in sera of obese patients: fall with weight loss. J Clin Endocrinol Metab. 1998; 83:2907–10.36. Mohamed-Ali V, Goodrick S, Rawesh A, Katz DR, Miles JM, Yudkin JS, et al. Subcutaneous adipose tissue releases interleukin-6, but not tumor necrosis factor-alpha, in vivo. J Clin Endocrinol Metab. 1997; 82:4196–200.37. Kubaszek A, Pihlajamaki J, Komarovski V, Lindi V, Lindstrom J, Eriksson J, et al. Promoter polymorphisms of the TNF-alpha (G-308A) and IL-6 (C-174G) genes predict the conversion from impaired glucose tolerance to type 2 diabetes: the Finnish Diabetes Prevention Study. Diabetes. 2003; 52:1872–6.38. Ozcan U, Cao Q, Yilmaz E, Lee AH, Iwakoshi NN, Ozdelen E, et al. Endoplasmic reticulum stress links obesity, insulin action, and type 2 diabetes. Science. 2004; 306:457–61.
Article39. Furukawa S, Fujita T, Shimabukuro M, Iwaki M, Yamada Y, Nakajima Y, et al. Increased oxidative stress in obesity and its impact on metabolic syndrome. J Clin Invest. 2004; 114:1752–61.
Article40. Summers SA. Ceramides in insulin resistance and lipotoxicity. Prog Lipid Res. 2006; 45:42–72.
Article41. Shoelson SE, Lee J, Goldfine AB. Inflammation and insulin resistance. J Clin Invest. 2006; 116:1793–801.
Article42. Hirosumi J, Tuncman G, Chang L, Gorgun CZ, Uysal KT, Maeda K, et al. A central role for JNK in obesity and insulin resistance. Nature. 2002; 420:333–6.
Article43. Barnes PJ, Karin M. Nuclear factor-kappaB: a pivotal transcription factor in chronic inflammatory diseases. N Engl J Med. 1997; 336:1066–71.
Article44. Seppala-Lindroos A, Vehkavaara S, Hakkinen AM, Goto T, Westerbacka J, Sovijarvi A, et al. Fat accumulation in the liver is associated with defects in insulin suppression of glucose production and serum free fatty acids independent of obesity in normal men. J Clin Endocrinol Metab. 2002; 87:3023–8.
Article45. Kelley DE, McKolanis TM, Hegazi RA, Kuller LH, Kalhan SC. Fatty liver in type 2 diabetes mellitus: relation to regional adiposity, fatty acids, and insulin resistance. Am J Physiol Endocrinol Metab. 2003; 285:E906–16.
Article46. Rhee EJ, Lee WY, Cho YK, Kim BI, Sung KC. Hyperinsulinemia and the development of nonalcoholic fatty liver disease in nondiabetic adults. Am J Med. 2011; 124:69–76.
Article47. Anstee QM, Targher G, Day CP. Progression of NAFLD to diabetes mellitus, cardiovascular disease or cirrhosis. Nat Rev Gastroenterol Hepatol. 2013; 10:330–44.
Article48. Birkenfeld AL, Shulman GI. Nonalcoholic fatty liver disease, hepatic insulin resistance, and type 2 diabetes. Hepatology. 2014; 59:713–23.
Article49. Donnelly KL, Smith CI, Schwarzenberg SJ, Jessurun J, Boldt MD, Parks EJ. Sources of fatty acids stored in liver and secreted via lipoproteins in patients with nonalcoholic fatty liver disease. J Clin Invest. 2005; 115:1343–51.50. Roden M. Mechanisms of disease: hepatic steatosis in type 2 diabetes. Pathogenesis and clinical relevance. Nat Clin Pract Endocrinol Metab. 2006; 2:335–48.51. Shimano H, Horton JD, Shimomura I, Hammer RE, Brown MS, Goldstein JL. Isoform 1c of sterol regulatory element binding protein is less active than isoform 1a in livers of transgenic mice and in cultured cells. J Clin Invest. 1997; 99:846–54.
Article52. Yahagi N, Shimano H, Hasty AH, Matsuzaka T, Ide T, Yoshikawa T, et al. Absence of sterol regulatory element-binding protein-1 (SREBP-1) ameliorates fatty livers but not obesity or insulin resistance in Lep(ob)/Lep(ob) mice. J Biol Chem. 2002; 277:19353–7.53. Tamura S, Shimomura I. Contribution of adipose tissue and de novo lipogenesis to nonalcoholic fatty liver disease. J Clin Invest. 2005; 115:1139–42.
Article54. Wolfrum C, Asilmaz E, Luca E, Friedman JM, Stoffel M. Foxa2 regulates lipid metabolism and ketogenesis in the liver during fasting and in diabetes. Nature. 2004; 432:1027–32.
Article55. Koliaki C, Szendroedi J, Kaul K, Jelenik T, Nowotny P, Jankowiak F, et al. Adaptation of hepatic mitochondrial function in humans with non-alcoholic fatty liver is lost in steatohepatitis. Cell Metab. 2015; 21:739–46.
Article56. Yamaguchi K, Yang L, McCall S, Huang J, Yu XX, Pandey SK, et al. Inhibiting triglyceride synthesis improves hepatic steatosis but exacerbates liver damage and fibrosis in obese mice with nonalcoholic steatohepatitis. Hepatology. 2007; 45:1366–74.
Article57. Hebbard L, George J. Animal models of nonalcoholic fatty liver disease. Nat Rev Gastroenterol Hepatol. 2011; 8:35–44.
Article58. Gruben N, Shiri-Sverdlov R, Koonen DP, Hofker MH. Nonalcoholic fatty liver disease: a main driver of insulin resistance or a dangerous liaison? Biochim Biophys Acta. 2014; 1842:2329–43.
Article59. Lam TK, Carpentier A, Lewis GF, van de Werve G, Fantus IG, Giacca A. Mechanisms of the free fatty acid-induced increase in hepatic glucose production. Am J Physiol Endocrinol Metab. 2003; 284:E863–73.
Article60. Gao Z, Zhang X, Zuberi A, Hwang D, Quon MJ, Lefevre M, et al. Inhibition of insulin sensitivity by free fatty acids requires activation of multiple serine kinases in 3T3-L1 adipocytes. Mol Endocrinol. 2004; 18:2024–34.
Article61. Lee JY, Sohn KH, Rhee SH, Hwang D. Saturated fatty acids, but not unsaturated fatty acids, induce the expression of cyclooxygenase-2 mediated through Toll-like receptor 4. J Biol Chem. 2001; 276:16683–9.
Article62. Shi H, Kokoeva MV, Inouye K, Tzameli I, Yin H, Flier JS. TLR4 links innate immunity and fatty acid-induced insulin resistance. J Clin Invest. 2006; 116:3015–25.
Article63. Knebel B, Haas J, Hartwig S, Jacob S, Kollmer C, Nitzgen U, et al. Liver-specific expression of transcriptionally active SREBP-1c is associated with fatty liver and increased visceral fat mass. PLoS One. 2012; 7:e31812.
Article64. Ibdah JA, Perlegas P, Zhao Y, Angdisen J, Borgerink H, Shadoan MK, et al. Mice heterozygous for a defect in mitochondrial trifunctional protein develop hepatic steatosis and insulin resistance. Gastroenterology. 2005; 128:1381–90.
Article65. Palma R, Pronio A, Romeo M, Scognamiglio F, Ventriglia L, Ormando VM, et al. The role of insulin resistance in fueling NAFLD pathogenesis: from molecular mechanisms to clinical implications. J Clin Med. 2022; 11:3649.
Article66. Scorletti E, Carr RM. A new perspective on NAFLD: focusing on lipid droplets. J Hepatol. 2022; 76:934–45.
Article67. Jung CH, Rhee EJ, Kwon H, Chang Y, Ryu S, Lee WY. Visceral-to-subcutaneous abdominal fat ratio is associated with nonalcoholic fatty liver disease and liver fibrosis. Endocrinol Metab (Seoul). 2020; 35:165–76.
Article68. Jung I, Koo DJ, Lee MY, Moon SJ, Kwon H, Park SE, et al. Increased risk of nonalcoholic fatty liver disease in individuals with high weight variability. Endocrinol Metab (Seoul). 2021; 36:845–54.
Article69. Xu L, Li D. Body-weight fluctuations and outcomes in coronary disease. N Engl J Med. 2017; 377:94.
Article70. Gaggini M, Morelli M, Buzzigoli E, DeFronzo RA, Bugianesi E, Gastaldelli A. Non-alcoholic fatty liver disease (NAFLD) and its connection with insulin resistance, dyslipidemia, atherosclerosis and coronary heart disease. Nutrients. 2013; 5:1544–60.
Article71. Bedogni G, Miglioli L, Masutti F, Tiribelli C, Marchesini G, Bellentani S. Prevalence of and risk factors for nonalcoholic fatty liver disease: the Dionysos nutrition and liver study. Hepatology. 2005; 42:44–52.
Article72. Sorrentino P, Terracciano L, D’Angelo S, Ferbo U, Bracigliano A, Vecchione R. Predicting fibrosis worsening in obese patients with NASH through parenchymal fibronectin, HOMA-IR, and hypertension. Am J Gastroenterol. 2010; 105:336–44.
Article73. Pais R, Charlotte F, Fedchuk L, Bedossa P, Lebray P, Poynard T, et al. A systematic review of follow-up biopsies reveals disease progression in patients with non-alcoholic fatty liver. J Hepatol. 2013; 59:550–6.
Article74. Gomez de la Cuesta S, Aller de la Fuente R, Tafur Sanchez C, Izaola O, Garcia Sanchez C, Mora N, et al. Analytical, anthropometric and dietary factors associated with the development of fibrosis in patients with nonalcoholic fatty liver disease. Rev Esp Enferm Dig. 2018; 110:292–8.
Article75. McPherson S, Hardy T, Henderson E, Burt AD, Day CP, Anstee QM. Evidence of NAFLD progression from steatosis to fibrosing-steatohepatitis using paired biopsies: implications for prognosis and clinical management. J Hepatol. 2015; 62:1148–55.
Article76. Bae JC, Beste LA, Utzschneider KM. The impact of insulin resistance on hepatic fibrosis among United States adults with non-alcoholic fatty liver disease: NHANES 2017 to 2018. Endocrinol Metab (Seoul). 2022; 37:455–65.
Article77. Koo DJ, Lee MY, Jung I, Moon SJ, Kwon H, Park SE, et al. Baseline homeostasis model assessment of insulin resistance associated with fibrosis progression in patients with nonalcoholic fatty liver disease without diabetes: a cohort study. PLoS One. 2021; 16:e0255535.
Article78. Koo DJ, Lee MY, Jung I, Moon SJ, Kwon H, Park SE, et al. Changes in insulin resistance index and the risk of liver fibrosis in patients with nonalcoholic fatty liver disease without diabetes: Kangbuk Samsung Health Study. Endocrinol Metab (Seoul). 2021; 36:1016–28.
Article79. Lee JI, Kim MC, Moon BS, Song YS, Han EN, Lee HS, et al. The relationship between 10-year cardiovascular risk calculated using the pooled cohort equation and the severity of nonalcoholic fatty liver disease. Endocrinol Metab (Seoul). 2016; 31:86–92.
Article80. Lee MK, Rhee EJ, Kim MC, Moon BS, Lee JI, Song YS, et al. Metabolic health is more important than obesity in the development of nonalcoholic fatty liver disease: a 4-year retrospective study. Endocrinol Metab (Seoul). 2015; 30:522–30.
Article81. Jeon WS, Park SE, Rhee EJ, Park CY, Oh KW, Park SW, et al. Association of serum adipocyte-specific fatty acid binding protein with fatty liver index as a predictive indicator of nonalcoholic fatty liver disease. Endocrinol Metab (Seoul). 2013; 28:283–7.
Article82. Seo YY, Cho YK, Bae JC, Seo MH, Park SE, Rhee EJ, et al. Tumor necrosis factor-α as a predictor for the development of nonalcoholic fatty liver disease: a 4-year follow-up study. Endocrinol Metab (Seoul). 2013; 28:41–5.
Article83. Jung I, Lee DY, Lee MY, Kwon H, Rhee EJ, Park CY, et al. Autonomic imbalance increases the risk for non-alcoholic fatty liver disease. Front Endocrinol (Lausanne). 2021; 12:752944.
Article84. Lee YH, Bang H, Park YM, Bae JC, Lee BW, Kang ES, et al. Non-laboratory-based self-assessment screening score for non-alcoholic fatty liver disease: development, validation and comparison with other scores. PLoS One. 2014; 9:e107584.
Article85. Koo DJ, Lee MY, Jung I, Moon SJ, Kwon H, Rhee EJ, et al. Increased risk of NAFLD in adults with glomerular hyperfiltration: an 8-year cohort study based on 147,162 Koreans. J Pers Med. 2022; 12:1142.
Article86. Kim HM, Lee YH. The leg fat to total fat ratio is associated with lower risks of non-alcoholic fatty liver disease and less severe hepatic fibrosis: results from nationwide surveys (KNHANES 2008-2011). Endocrinol Metab (Seoul). 2021; 36:1232–42.
Article87. Lee CH, Seto WK, Ieong K, Lui DT, Fong CH, Wan HY, et al. Development of a non-invasive liver fibrosis score based on transient elastography for risk stratification in patients with type 2 diabetes. Endocrinol Metab (Seoul). 2021; 36:134–45.
Article88. Cho Y, Lee YH. State-of-the-art overview of the pharmacological treatment of non-alcoholic steatohepatitis. Endocrinol Metab (Seoul). 2022; 37:38–52.
Article89. Lee MJ, Kim EH, Bae SJ, Kim GA, Park SW, Choe J, et al. Age-related decrease in skeletal muscle mass is an independent risk factor for incident nonalcoholic fatty liver disease: a 10-year retrospective cohort study. Gut Liver. 2019; 13:67–76.
Article90. Eslam M, Sarin SK, Wong VW, Fan JG, Kawaguchi T, Ahn SH, et al. The Asian Pacific Association for the Study of the Liver clinical practice guidelines for the diagnosis and management of metabolic associated fatty liver disease. Hepatol Int. 2020; 14:889–919.
Article91. Bae JC, Suh S, Park SE, Rhee EJ, Park CY, Oh KW, et al. Regular exercise is associated with a reduction in the risk of NAFLD and decreased liver enzymes in individuals with NAFLD independent of obesity in Korean adults. PLoS One. 2012; 7:e46819.
Article92. Lee BW, Lee YH, Park CY, Rhee EJ, Lee WY, Kim NH, et al. Non-alcoholic fatty liver disease in patients with type 2 diabetes mellitus: a position statement of the Fatty Liver Research Group of the Korean Diabetes Association. Diabetes Metab J. 2020; 44:382–401.
Article93. Andre P, Balkau B, Born C, Charles MA, Eschwege E; D.E.S.I.R. study group. Three-year increase of gamma-glutamyltransferase level and development of type 2 diabetes in middle-aged men and women: the D.E.S.I.R. cohort. Diabetologia. 2006; 49:2599–603.
Article94. Kim CH, Park JY, Lee KU, Kim JH, Kim HK. Association of serum gamma-glutamyltransferase and alanine aminotransferase activities with risk of type 2 diabetes mellitus independent of fatty liver. Diabetes Metab Res Rev. 2009; 25:64–9.95. Ko SH, Baeg MK, Han KD, Ko SH, Ahn YB. Increased liver markers are associated with higher risk of type 2 diabetes. World J Gastroenterol. 2015; 21:7478–87.
Article96. Ballestri S, Zona S, Targher G, Romagnoli D, Baldelli E, Nascimbeni F, et al. Nonalcoholic fatty liver disease is associated with an almost twofold increased risk of incident type 2 diabetes and metabolic syndrome. Evidence from a systematic review and meta-analysis. J Gastroenterol Hepatol. 2016; 31:936–44.
Article97. Ekstedt M, Franzen LE, Mathiesen UL, Thorelius L, Holmqvist M, Bodemar G, et al. Long-term follow-up of patients with NAFLD and elevated liver enzymes. Hepatology. 2006; 44:865–73.
Article98. Bae JC, Cho YK, Lee WY, Seo HI, Rhee EJ, Park SE, et al. Impact of nonalcoholic fatty liver disease on insulin resistance in relation to HbA1c levels in nondiabetic subjects. Am J Gastroenterol. 2010; 105:2389–95.
Article99. Bae JC, Rhee EJ, Lee WY, Park SE, Park CY, Oh KW, et al. Combined effect of nonalcoholic fatty liver disease and impaired fasting glucose on the development of type 2 diabetes: a 4-year retrospective longitudinal study. Diabetes Care. 2011; 34:727–9.100. Bae JC, Han JM, Cho JH, Kwon H, Park SE, Park CY, et al. The persistence of fatty liver has a differential impact on the development of diabetes: the Kangbuk Samsung Health Study. Diabetes Res Clin Pract. 2018; 135:1–6.
Article101. Bae JC, Kim SK, Han JM, Kwon S, Lee DY, Kim J, et al. Additive effect of non-alcoholic fatty liver disease on the development of diabetes in individuals with metabolic syndrome. Diabetes Res Clin Pract. 2017; 129:136–43.
Article102. Choi JH, Rhee EJ, Bae JC, Park SE, Park CY, Cho YK, et al. Increased risk of type 2 diabetes in subjects with both elevated liver enzymes and ultrasonographically diagnosed nonalcoholic fatty liver disease: a 4-year longitudinal study. Arch Med Res. 2013; 44:115–20.
Article103. Chung SM, Kang MK, Moon JS, Park JG. Performance of simple fibrosis score in non-alcoholic fatty liver disease with and without type 2 diabetes. Endocrinol Metab (Seoul). 2023; 38:277–81.
Article104. Kim J, Lee M, Kim SY, Kim JH, Nam JS, Chun SW, et al. Nonlaboratory-based simple screening model for nonalcoholic fatty liver disease in patients with type 2 diabetes developed using multi-center cohorts. Endocrinol Metab (Seoul). 2021; 36:823–34.
Article105. Barb D, Repetto EM, Stokes ME, Shankar SS, Cusi K. Type 2 diabetes mellitus increases the risk of hepatic fibrosis in individuals with obesity and nonalcoholic fatty liver disease. Obesity (Silver Spring). 2021; 29:1950–60.
Article106. ElSayed NA, Aleppo G, Aroda VR, Bannuru RR, Brown FM, Bruemmer D, et al. 4. Comprehensive medical evaluation and assessment of comorbidities: standards of care in diabetes: 2023. Diabetes Care. 2023; 46(Suppl 1):S49–67.107. Dyson J, Jaques B, Chattopadyhay D, Lochan R, Graham J, Das D, et al. Hepatocellular cancer: the impact of obesity, type 2 diabetes and a multidisciplinary team. J Hepatol. 2014; 60:110–7.
Article108. Ranjbar G, Mikhailidis DP, Sahebkar A. Effects of newer antidiabetic drugs on nonalcoholic fatty liver and steatohepatitis: think out of the box! Metabolism. 2019; 101:154001.
Article109. Dougherty JA, Guirguis E, Thornby KA. A systematic review of newer antidiabetic agents in the treatment of nonalcoholic fatty liver disease. Ann Pharmacother. 2021; 55:65–79.
Article110. Bae JC. DPP-4 inhibitor in type 2 diabetes mellitus patient with non-alcoholic fatty liver disease: achieving two goals at once? Endocrinol Metab (Seoul). 2022; 37:858–60.
Article111. Bae JC, Lee WY, Yoon KH, Park JY, Son HS, Han KA, et al. Improvement of nonalcoholic fatty liver disease with carnitineorotate complex in type 2 diabetes (CORONA): a randomized controlled trial. Diabetes Care. 2015; 38:1245–52.
Article112. Lee J, Hong SW, Chae SW, Kim DH, Choi JH, Bae JC, et al. Exendin-4 improves steatohepatitis by increasing Sirt1 expression in high-fat diet-induced obese C57BL/6J mice. PLoS One. 2012; 7:e31394.
Article113. Lee J, Hong SW, Park SE, Rhee EJ, Park CY, Oh KW, et al. Exendin-4 attenuates endoplasmic reticulum stress through a SIRT1-dependent mechanism. Cell Stress Chaperones. 2014; 19:649–56.
Article114. Lee J, Hong SW, Park SE, Rhee EJ, Park CY, Oh KW, et al. Exendin-4 regulates lipid metabolism and fibroblast growth factor 21 in hepatic steatosis. Metabolism. 2014; 63:1041–8.
Article115. Lee J, Hong SW, Park SE, Rhee EJ, Park CY, Oh KW, et al. Exendin-4 inhibits the expression of SEPP1 and fetuin-A via improvement of palmitic acid-induced endoplasmic reticulum stress by AMPK. Endocrinol Metab (Seoul). 2015; 30:177–84.
Article116. Lee J, Hong SW, Kim MJ, Moon SJ, Kwon H, Park SE, et al. Dulaglutide ameliorates palmitic acid-induced hepatic steatosis by activating FAM3A signaling pathway. Endocrinol Metab (Seoul). 2022; 37:74–83.
Article117. Lee Y, Kim BR, Kang GH, Lee GJ, Park YJ, Kim H, et al. The effects of PPAR agonists on atherosclerosis and nonalcoholic fatty liver disease in ApoE-/-FXR-/- mice. Endocrinol Metab (Seoul). 2021; 36:1243–53.
Article118. Nguyen G, Park SY, Do DV, Choi DH, Cho EH. Gemigliptin alleviates succinate-induced hepatic stellate cell activation by ameliorating mitochondrial dysfunction. Endocrinol Metab (Seoul). 2022; 37:918–28.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Nonalcoholic Fatty Liver Disease and Diabetes: An Epidemiological Perspective
- GLP-1 Receptor Agonist and Non-Alcoholic Fatty Liver Disease
- Association of Non-alcoholic Fatty Liver Disease with Insulin Resistance in Non-Diabetic, Normal Weight Adults
- Clinical Characteristics of Non-Alcoholic Fatty Liver Disease Based on Analyses from the Kangbuk Samsung Health Study
- Causal Relationship of Non-alcoholic Fatty Liver Disease with Obesity and Insulin Resistance