Korean J Gastroenterol.
2024 Apr;83(4):157-162. 10.4166/kjg.2024.021.
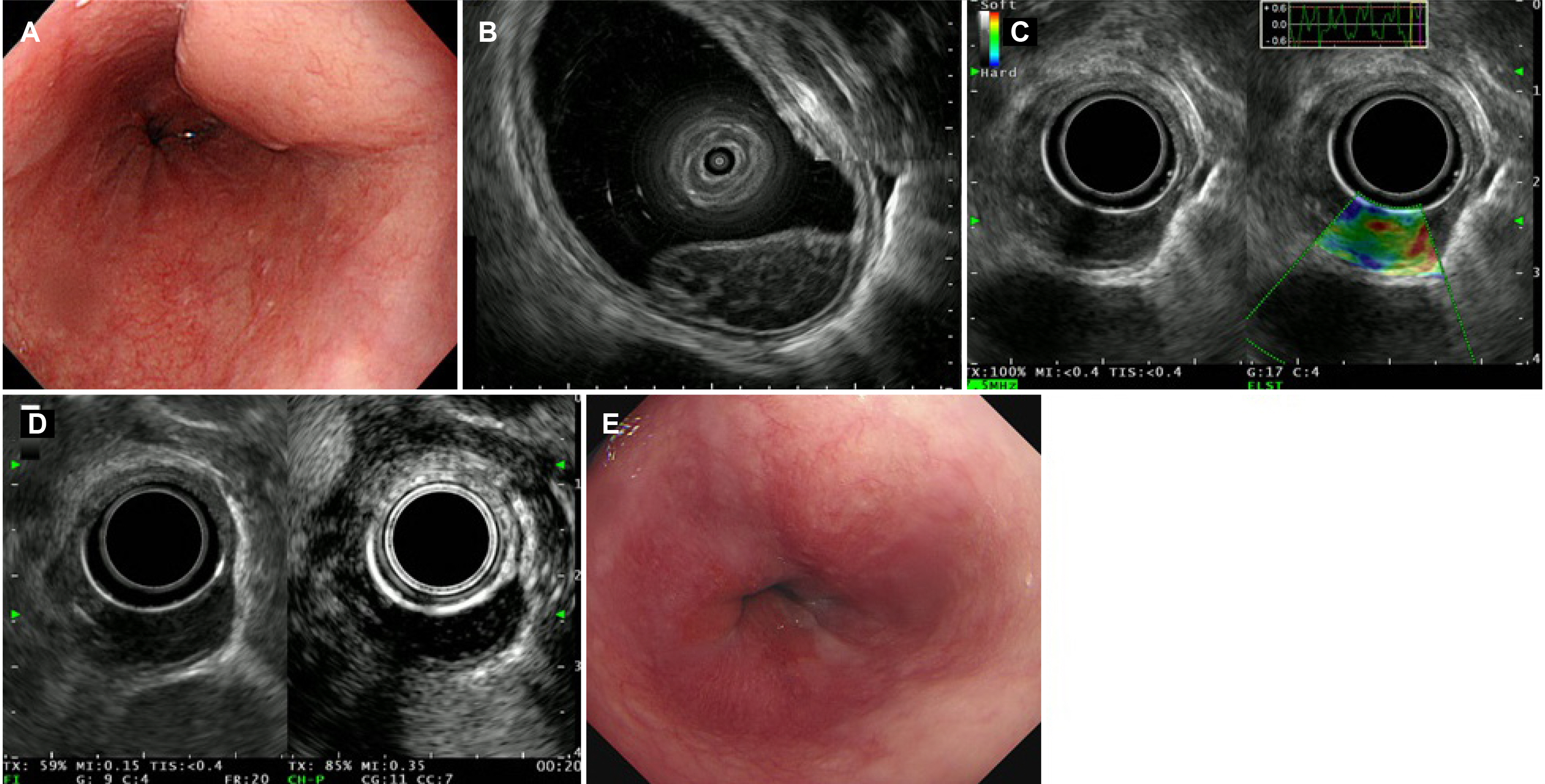
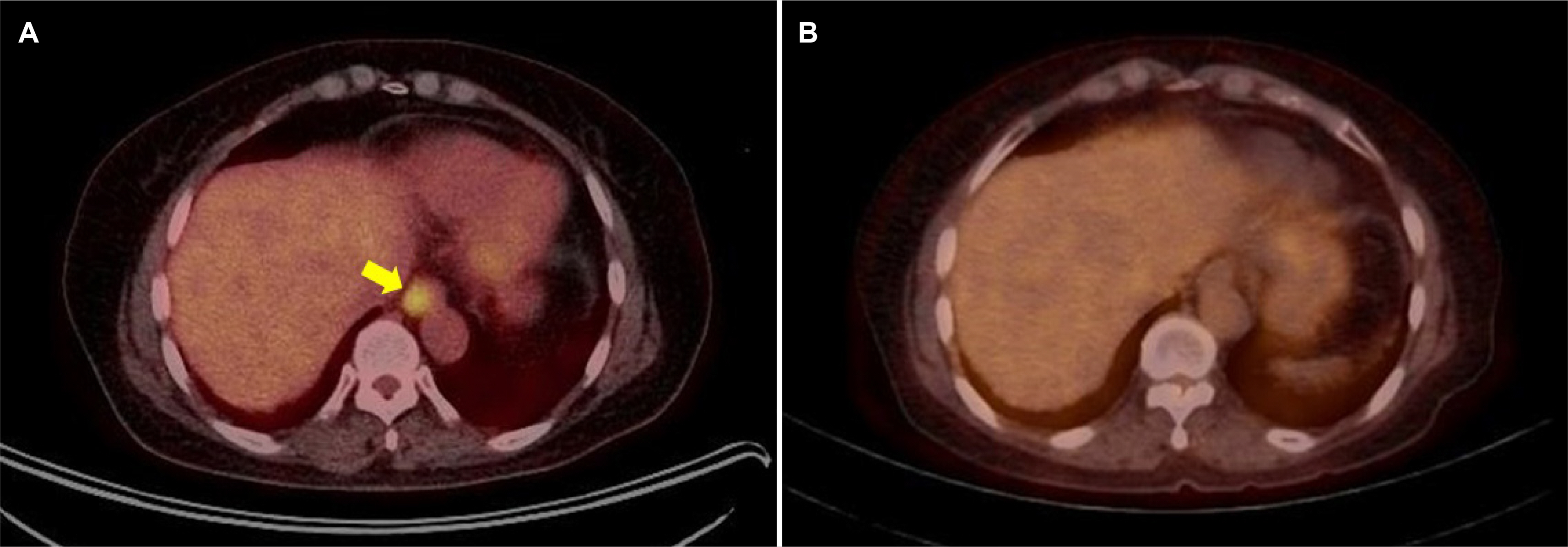
A Case of Esophageal MALT Lymphoma Mimicking a Subepithelial Tumor
- Affiliations
-
- 1Division of Gastroenterology, Pusan National University Hospital, Busan, Korea
- 2Department of Internal Medicine, Pusan National University School of Medicine, Busan, Korea
- 3Biomedical Research Institute, Pusan National University Hospital, Busan, Korea
- 4Department of Pathology, Pusan National University Hospital, Busan, Korea
- KMID: 2555649
- DOI: http://doi.org/10.4166/kjg.2024.021
Abstract
- Mucosa-associated lymphoid tissue (MALT) lymphoma, also known as extranodal marginal zone lymphoma, is a low-grade B-cell lymphoma that can develop in the mucosal layer of various organs, including the gastrointestinal tract, salivary glands, lungs, and skin. The most common site is the gastrointestinal tract, particularly the stomach. On the other hand, primary esophageal lymphomas are extremely rare. MALT lymphomas can undergo histological transformation into more aggressive B-cell lymphomas, such as diffuse large B-cell lymphoma, resulting in a poor prognosis. This paper reports a rare case of primary esophageal MALT lymphoma mimicking a subepithelial tumor located in the lower esophagus that was treated successfully with radiotherapy. MALT lymphoma should be included in a differential diagnosis when subepithelial tumors are found in the esophagus, particularly if endoscopic ultrasonography reveals the tumor to be located in the deep mucosal and submucosal layers. Following the precise diagnosis, accurate staging and appropriate treatment are crucial. Regular follow-up is necessary to assess the possibility of recurrence or transformation to high-grade lymphoma.
Figure
Reference
-
1. Ma Q, Zhang C, Fang S, et al. 2017; Primary esophageal mucosa-associated lymphoid tissue lymphoma: A case report and review of literature. Medicine (Baltimore). 96:e6478. DOI: 10.1097/MD.0000000000006478. PMID: 28353588. PMCID: PMC5380272.2. Baek DH, Kim GH, Song GA, et al. 2012; Primary esophageal mucosa-associated lymphoid tissue lymphoma treated with endoscopic resection. Gastrointest Endosc. 75:1282–1283. DOI: 10.1016/j.gie.2011.06.003. PMID: 21820112.
Article3. Codipilly DC, Fang H, Alexander JA, Katzka DA, Ravi K. 2018; Subepithelial esophageal tumors: a single-center review of resected and surveilled lesions. Gastrointest Endosc. 87:370–377. DOI: 10.1016/j.gie.2017.07.043. PMID: 28782509.
Article4. Choe Y, Cho YK, Kim GH, et al. 2023; Prevalence, natural progression, and clinical practices of upper gastrointestinal subepithelial lesions in Korea: a multicenter study. Clin Endosc. 56:744–753. DOI: 10.5946/ce.2023.005. PMID: 37621066. PMCID: PMC10665619.
Article5. Deprez PH, Moons LMG, OʼToole D, et al. 2022; Endoscopic management of subepithelial lesions including neuroendocrine neoplasms: European Society of Gastrointestinal Endoscopy (ESGE) Guideline. Endoscopy. 54:412–429. DOI: 10.1055/a-1751-5742. PMID: 35180797.
Article6. Lee KH, Yoo CK, Lee HL, et al. 2021; The pathologic confirmation in subepithelial tumors. Korean J Helicobacter Up Gastrointest Res. 21:215–219. DOI: 10.7704/kjhugr.2020.0067.
Article7. Kobayashi S, Iwamuro M, Nishida K, et al. 2018; Primary localized esophageal mucosa-associated lymphoid tissue lymphoma treated by endoscopic submucosal dissection. Intern Med. 57:2347–2352. DOI: 10.2169/internalmedicine.0487-17. PMID: 29607943. PMCID: PMC6148167.
Article8. Ishikawa E, Nakamura M, Satou A, Shimada K, Nakamura S. 2022; Mucosa-associated lymphoid tissue (MALT) lymphoma in the gastrointestinal tract in the modern era. Cancers (Basel). 14:446. DOI: 10.3390/cancers14020446. PMID: 35053607. PMCID: PMC8773811.
Article9. Moriya K, Tamura H, Nakamura K, Hosone M, Inokuchi K. 2016; A primary esophageal MALT lymphoma patient with Helicobacter pylori infection achieved complete remission after H. pylori eradication without anti-lymphoma treatment. Leuk Res Rep. 7:2–5. DOI: 10.1016/j.lrr.2016.12.001. PMID: 28053856. PMCID: PMC5196236.
Article10. Xia Y, Wang Y, Han J, Liu M. 2021; En Bloc resection of primary large esophageal mucosa-associated lymphoid tissue lymphoma by endoscopic submucosal dissection: A case report. Front Med (Lausanne). 8:757485. DOI: 10.3389/fmed.2021.757485. PMID: 34722592. PMCID: PMC8548363.
Article11. Oría IC, Pizzala JE, Villaverde AM, et al. 2021; Primary lymphoma of the entire esophagus diagnosed by endoscopic ultrasound-guided fine needle aspiration (EUS-FNA). Radiol Case Rep. 16:1242–1244. DOI: 10.1016/j.radcr.2021.02.051. PMID: 33868528. PMCID: PMC8041659.
Article12. Kim GH, Choi BG, Lee JN, et al. 2010; [2 cases of gastric mucosa-associated lymphoid tissue lymphoma presenting as a submucosal tumor-like lesion]. Korean J Gastroenterol. 56:103–108. Korean. DOI: 10.4166/kjg.2010.56.2.103. PMID: 20729622.
Article13. Bang JH, Kang JH, Kim SH, et al. 2023; Primary esophageal mucosa-associated lymphoid tissue lymphoma: A rare case report and review of other published data. Korean J Helicobacter Up Gastrointest Res. 23:207–213. DOI: 10.7704/kjhugr.2023.0026.
Article14. Choi J. 2022; Successful endoscopic resection of gastric mucosa-associated lymphoid tissue lymphoma unresponsive to Helicobacter pylori eradication therapy. Clin Endosc. 55:136–140. DOI: 10.5946/ce.2020.232. PMID: 33190433. PMCID: PMC8831412.
Article15. Kishi K, Maeda H, Nakamura Y, Shirai S, Sato M. 2012; Radiotherapy for mucosa-associated lymphoid tissue (MALT) lymphoma of the esophagus: a case report with a diagnostic and therapeutic discussion. Int J Clin Oncol. 17:174–180. DOI: 10.1007/s10147-011-0265-8. PMID: 21660505.
Article16. Kitamoto Y, Hasegawa M, Ishikawa H, et al. 2003; Mucosa-associated lymphoid tissue lymphoma of the esophagus: a case report. J Clin Gastroenterol. 36:414–416. DOI: 10.1097/00004836-200305000-00011. PMID: 12702984.
Article17. Yano S, Usui N, Dobashi N, et al. 2009; A case of primary esophageal mucosa-associated lymphoid tissue lymphoma with a numerical abnormality of 18q21 detected by fluorescence in situ hybridization. Ann Hematol. 88:703–704. DOI: 10.1007/s00277-008-0653-y. PMID: 19052745.
Article18. Hosaka S, Nakamura N, Akamatsu T, et al. 2002; A case of primary low grade mucosa associated lymphoid tissue (MALT) lymphoma of the oesophagus. Gut. 51:281–284. DOI: 10.1136/gut.51.2.281. PMID: 12117895. PMCID: PMC1773320.
Article19. Kudo K, Ota M, Narumiya K, Shirai Y, Ohki T, Yamamoto M. 2014; Primary esophageal mucosa-associated lymphoid tissue lymphoma treated by endoscopic submucosal dissection. Dig Endosc. 26:478–481. DOI: 10.1111/den.12138. PMID: 23772967.
Article20. Bardisi ES, Alghanmi N, Merdad AA. 2014; Primary mucosa-associated lymphoid tissue lymphoma of the esophagus masquerading as a benign tumor. Ann Med Surg (Lond). 3:39–42. DOI: 10.1016/j.amsu.2014.05.001. PMID: 25568784. PMCID: PMC4268481.
Article21. Miyazaki T, Kato H, Masuda N, et al. 2004; Mucosa-associated lymphoid tissue lymphoma of the esophagus: case report and review of the literature. Hepatogastroenterology. 51:750–753. PMID: 15143908.22. Lee DS, Ahn YC, Eom DW, Lee SJ. 2016; Primary esophageal mucosa-associated lymphoid tissue lymphoma diagnosed by using stacked forceps biopsy. Dis Esophagus. 29:887–890. DOI: 10.1111/dote.12309. PMID: 25626120.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Colonic Mucosa-associated Lymphoid Tissue Lymphoma Treated by Radiation Therapy: Report of a Case and Literature Review
- A Case of Laryngeal Mucosa Associated Lymphoid Tissue Lymphoma Mimicking Laryngeal Amyloidosis
- Successful Endoscopic Resection of Residual Colonic Mucosa-Associated Lymphoid Tissue Lymphoma after Polypectomy
- A Case of Low-grade Gastric MALT Lymphoma Mimicking as a Advanced Gastric Cancer
- Primary Mucosa-associated Lymphoid Tissue Lymphoma Metachronously Involving Esophagus and Stomach