Acute Crit Care.
2024 Feb;39(1):169-178. 10.4266/acc.2023.01102.
Clinical implications of pleural effusion following left ventricular assist device implantation
- Affiliations
-
- 1Division of Cardiology, Department of Internal Medicine, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Korea
- 2Department of Thoracic and Cardiovascular Surgery, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Korea
- KMID: 2555236
- DOI: http://doi.org/10.4266/acc.2023.01102
Abstract
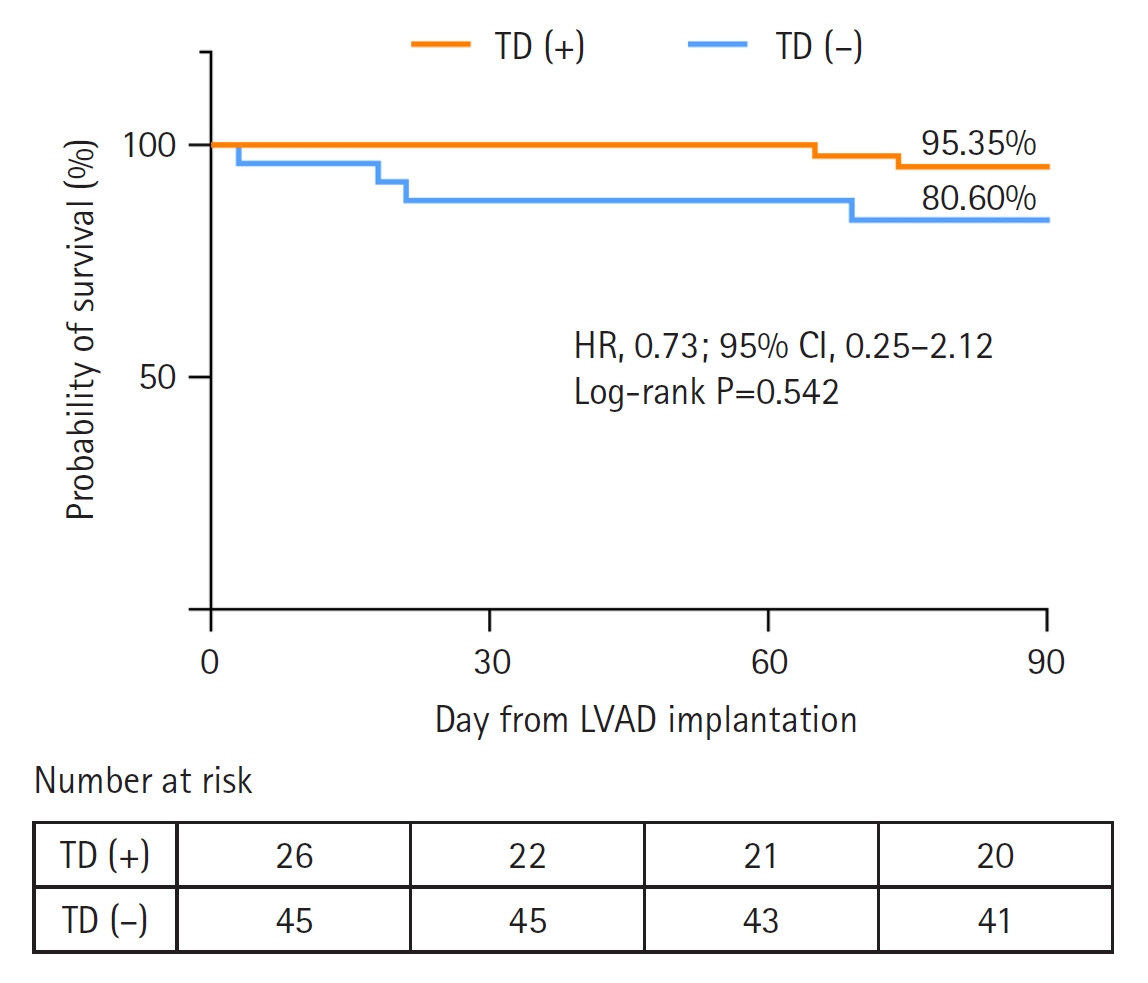
- Background
Studies on the association between pleural effusion (PE) and left ventricular assist devices (LVADs) are limited. This study aimed to examine the characteristics and the clinical impact of PE following LVAD implantation. Methods: This study is a prospective analysis of patients who underwent LVAD implantation from June 2015 to December 2022. We investigated the prognostic impact of therapeutic drainage (TD) on clinical outcomes. We also compared the characteristics and clinical outcomes between early and late PE and examined the factors related to the development of late PE. Results: A total of 71 patients was analyzed. The TD group (n=45) had a longer ward stay (days; median [interquartile range]: 31.0 [23.0–46.0] vs. 21.0 [16.0–34.0], P=0.006) and total hospital stay (47.0 [36.0–82.0] vs. 31.0 [22.0–48.0], P=0.002) compared to the no TD group (n=26). Early PE was mostly exudate, left-sided, and neutrophil-dominant even though predominance of lymphocytes was the most common finding in late PE. Patients with late PE had a higher rate of reintubation within 14 days (31.8% vs. 4.1%, P=0.004) and longer hospital stays than those without late PE (67.0 [43.0–104.0] vs. 36.0 [28.0–48.0], P<0.001). Subgroup analysis indicated that female sex, low body mass index, cardiac resynchronization therapy, and hypoalbuminemia were associated with late PE. Conclusions: Compared to patients not undergoing TD, those undergoing TD had a longer hospital stay but not a higher 90-day mortality. Patients with late PE had poor clinical outcomes. Therefore, the correction of risk factors, like hypoalbuminemia, may be required.
Figure
Cited by 1 articles
-
Nuances of pleural effusion after left ventricular assist devices implantation: insights from therapeutic drainage and preoperative predictors
Huijin Lee, Jeehoon Kang
Acute Crit Care. 2024;39(1):192-193. doi: 10.4266/acc.2024.00157.
Reference
-
1. Correction to: 2022 AHA/ACC/HFSA Guideline for the Management of Heart Failure: a report of the American College of Cardiology/American Heart Association Joint Committee on Clinical Practice Guidelines. Circulation. 2022; 146:e185.2. Ulubay G, Küpeli E, Er DedeARKgınoğlu B, Savaş Bozbaş Ş, Alekberov M, Salman Sever Ö, et al. Postoperative pleural effusions after orthotopic heart transplant: cause, clinical manifestations, and course. Exp Clin Transplant. 2016; 14(Suppl 3):125–9.3. Jain A, Devarajan A, Assallum H, Malekan R, Lanier GM, Epelbaum O. Characteristics of early pleural effusions after orthotopic heart transplantation: comparison with coronary artery bypass graft surgery. Pleura Peritoneum. 2021; 6:161–5.
Article4. Labidi M, Baillot R, Dionne B, Lacasse Y, Maltais F, Boulet LP. Pleural effusions following cardiac surgery: prevalence, risk factors, and clinical features. Chest. 2009; 136:1604–11.5. Peng MJ, Vargas FS, Cukier A, Terra-Filho M, Teixeira LR, Light RW. Postoperative pleural changes after coronary revascularization: comparison between saphenous vein and internal mammary artery grafting. Chest. 1992; 101:327–30.
Article6. Vargas FS, Cukier A, Terra-Filho M, Hueb W, Teixeira LR, Light RW. Relationship between pleural changes after myocardial revascularization and pulmonary mechanics. Chest. 1992; 102:1333–6.
Article7. Schiefenhövel F, Poncette AS, Boyle EM, von Heymann C, Menk M, Vorderwülbecke G, et al. Pleural effusions are associated with adverse outcomes after cardiac surgery: a propensity-matched analysis. J Cardiothorac Surg. 2022; 17:298.
Article8. Bateman M, Alkhatib A, John T, Parikh M, Kheir F. Pleural effusion outcomes in intensive care: analysis of a large clinical database. J Intensive Care Med. 2020; 35:48–54.
Article9. Brims FJ, Davies MG, Elia A, Griffiths MJ. The effects of pleural fluid drainage on respiratory function in mechanically ventilated patients after cardiac surgery. BMJ Open Respir Res. 2015; 2:e000080.
Article10. Guha A, Munjampalli S, Bandi V, Loebe M, Noon G, Lunn W. Pleural effusion after ventricular assist device placement: prevalence and pleural fluid characteristics. Chest. 2008; 134:382–6.
Article11. Light RW, Rogers JT, Cheng D, Rodriguez RM. Large pleural effusions occurring after coronary artery bypass grafting: Cardiovascular Surgery Associates, PC. Ann Intern Med. 1999; 130:891–6.
Article12. Vargas FS, Uezumi KK, Janete FB, Terra-Filho M, Hueb W, Cukier A, et al. Acute pleuropulmonary complications detected by computed tomography following myocardial revascularization. Rev Hosp Clin Fac Med Sao Paulo. 2002; 57:135–42.
Article13. Imazio M. The post-pericardiotomy syndrome. Curr Opin Pulm Med. 2012; 18:366–74.
Article14. Lehto J, Kiviniemi T, Gunn J, Airaksinen J, Rautava P, Kytö V. Occurrence of postpericardiotomy syndrome: association with operation type and postoperative mortality after open-heart operations. J Am Heart Assoc. 2018; 7:e010269.
Article15. Light RW, Rogers JT, Moyers JP, Lee YC, Rodriguez RM, Alford WC Jr, et al. Prevalence and clinical course of pleural effusions at 30 days after coronary artery and cardiac surgery. Am J Respir Crit Care Med. 2002; 166(12 Pt 1):1567–71.
Article16. Callan PD, Santhanakrishnan K, Shaw S, Mehta V, Al-Aloul M, Kore S, et al. Increased risk of pleural effusion requiring therapeutic drainage following 3rd generation vs 2nd generation left ventricular assist device implantation: a single centre analysis. J Heart Lung Transplant. 2021; 40(4 Supplement):S397.
Article17. Jani SM, Ahmed S, Sheikh FH, Molina EJ, Najjar SS, Majure DT. Pleural effusions requiring drainage following LVAD implantation: potential contributor to prolonged length of stay. J Card Fail. 2016; 22(8 Supplement):S53.
Article18. Light RW, Macgregor MI, Luchsinger PC, Ball WC Jr. Pleural effusions: the diagnostic separation of transudates and exudates. Ann Intern Med. 1972; 77:507–13.
Article19. Hansen LS, Hjortdal VE, Jakobsen CJ, Heiberg J, Maagaard M, Sloth E. Early, dedicated follow-up and treatment of pleural effusions enhance the recovery rate after open cardiac surgery: results from a randomized, clinical trial. Eur J Cardiothorac Surg. 2017; 51:58–66.
Article20. Gupta A, Daggett C, Behera S, Ferraro M, Wells W, Starnes V. Risk factors for persistent pleural effusions after the extracardiac Fontan procedure. J Thorac Cardiovasc Surg. 2004; 127:1664–9.
Article21. Gupta M, Johann-Liang R, Sison CP, Quaegebeur J, Friedman DM. Relation of early pleural effusion after pediatric open heart surgery to cardiopulmonary bypass time and systemic inflammation as measured by serum interleukin-6. Am J Cardiol. 2001; 87:1220–3.
Article22. Chae G, Jun JB, Jung HS, Park CY, Kim JH, Kang BJ, et al. Histiocytic pleural effusion: the strong clue to malignancy. World J Surg Oncol. 2021; 19:180.
Article23. Prais D, Kuzmenko E, Amir J, Harel L. Association of hypoalbuminemia with the presence and size of pleural effusion in children with pneumonia. Pediatrics. 2008; 121:e533–8.
Article24. Joseph J, Strange C, Sahn SA. Pleural effusions in hospitalized patients with AIDS. Ann Intern Med. 1993; 118:856–9.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Temporary Right Ventricular Assist Device Insertion via Left Thoracotomy after Left Ventricular Assist Device Implantation
- Nuances of pleural effusion after left ventricular assist devices implantation: insights from therapeutic drainage and preoperative predictors
- Left Ventricular Assist Device Implantation via Dual Left Thoracotomy in an Adult Patient with Congenitally Corrected Transposition of the Great Arteries
- Successful open chest intraoperative epicardial ventricular tachycardia mapping and ablation during the HeartMate-3 left ventricular assist device implantation in Taiwan
- The Successful Implantation of Continuous-Flow Left Ventricular Assist Device as a Destination Therapy in Korea: Echocardiographic Assessment