Acute Crit Care.
2024 Feb;39(1):138-145. 10.4266/acc.2023.01375.
Clinical characteristics and outcomes of obstetric patients transferred directly to intensive care units
- Affiliations
-
- 1Research Associate Program in Emergency Medicine and Critical Care, Department of Emergency Medicine, University of Maryland School of Medicine, Baltimore, MD, USA
- 2Department of Emergency Medicine, University of Maryland School of Medicine, Baltimore, MD, USA
- 3Program in Trauma, University of Maryland School of Medicine, Baltimore, MD, USA
- 4Division of Pulmonary and Critical Care, Department of Internal Medicine, University of Maryland School of Medicine, Baltimore, MD, USA
- 5Department of Obstetrics, Gynecology and Reproductive Sciences, University of Maryland School of Medicine, Baltimore, MD, USA
- KMID: 2555232
- DOI: http://doi.org/10.4266/acc.2023.01375
Abstract
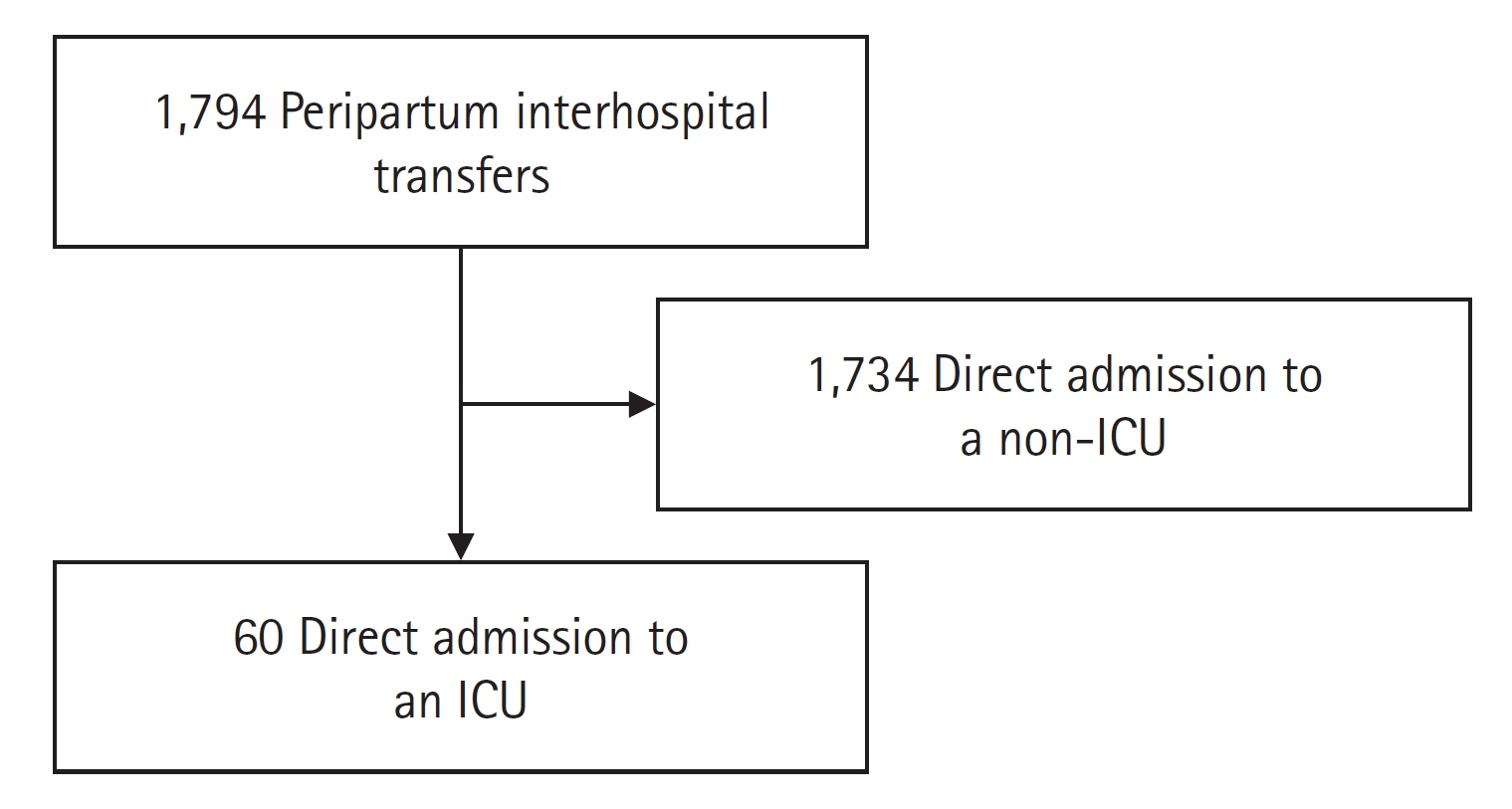
- Background
Medical complications in peripartum patients are uncommon. Often, these patients are transferred to tertiary care centers, but their conditions and outcomes are not well understood. Our study examined peripartum patients transferred to an intensive care unit (ICU) at an academic quaternary center. Methods: We reviewed charts of adult, non-trauma, interhospital transfer (IHT) peripartum patients sent to an academic quaternary ICU between January 2017 and December 2021. We conducted a descriptive analysis and used multivariable ordinal regression to examine associations of demographic and clinical factors with ICU length of stay (LOS) and hospital length of stay (HLOS). Results: Of 1,794 IHT peripartum patients, 60 (3.2%) were directly transferred to an ICU. The average was 32 years, with a median Sequential Organ Failure Assessment (SOFA) score of 3 (1–4.25) and Acute Physiology and Chronic Health Evaluation (APACHE) II score of 8 (7–12). Respiratory failure was most common (32%), followed by postpartum hemorrhage (15%) and sepsis (14%). Intubation was required for 24 (41%), and 4 (7%) needed extracorporeal membrane oxygenation. Only 1 (1.7%) died, while 45 (76.3%) were discharged. Median ICU LOS and HLOS were 5 days (212) and 8 days (5–17). High SOFA score was linked to longer HLOS, as was APACHE II. Conclusions: Transfers of critically ill peripartum patients between hospitals were rare but involved severe medical conditions. Despite this, their outcomes were generally positive. Larger studies are needed to confirm our findings.
Keyword
Figure
Reference
-
1. Tran QK, Hollis G, Beher R, Abdel-Wahab M, Mester G, Tanveer S, et al. Transport of peripartum patients for medical management: predictors of any intervention during transport. Cureus. 2022; 14:e31102.
Article2. NEMSIS Technical Assistance Center. National EMS database: NEMSIS research data set [Internet]. NEMSIS Technical Assistance Center;2017. [cited 2023 Dec 20]. Available from: https://nemsis.org/wp-content/uploads/2018/02/NEMSIS-RDS-221-2016-User-Manual.pdf.3. Nawrocki PS, Levy M, Tang N, Trautman S, Margolis A. Interfacility transport of the pregnant patient: a 5-year retrospective review of a single critical care transport program. Prehosp Emerg Care. 2019; 23:377–84.
Article4. O’Brien DJ, Hooker EA, Hignite J, Maughan E. Long-distance fixed-wing transport of obstetrical patients. South Med J. 2004; 97:816–8.
Article5. Jony L, Baskett TF. Emergency air transport of obstetric patients. J Obstet Gynaecol Can. 2007; 29:406–8.
Article6. Akl N, Coghlan EA, Nathan EA, Langford SA, Newnham JP. Aeromedical transfer of women at risk of preterm delivery in remote and rural Western Australia: why are there no births in flight? Aust N Z J Obstet Gynaecol. 2012; 52:327–33.7. Elsamadicy E, Plotnikova A, Yang J, Gambhir V, Zahid M, Pirzada S, et al. The utility of severity scoring systems to identify obstetric transports at risk for ICU escalation. Am J Obstet Gynecol. 2023; 228:S297–8.
Article8. Powell E, Sahadzic I, Najafali D, Berman E, Andersen K, Afridi LZ, et al. Is the critical care resuscitation unit sustainable: a 5-year experience of a beneficial and novel model. Crit Care Res Pract. 2022; 2022:6171598.
Article9. Heslehurst N, Ells LJ, Simpson H, Batterham A, Wilkinson J, Summerbell CD. Trends in maternal obesity incidence rates, demographic predictors, and health inequalities in 36,821 women over a 15-year period. BJOG. 2007; 114:187–94.
Article10. Farr A, Lenz-Gebhart A, Einig S, Ortner C, Holzer I, Elhenicky M, et al. Outcomes and trends of peripartum maternal admission to the intensive care unit. Wien Klin Wochenschr. 2017; 129:605–11.
Article11. Lapinsky SE, Hallett D, Collop N, Drover J, Lavercombe P, Leeman M, et al. Evaluation of standard and modified severity of illness scores in the obstetric patient. J Crit Care. 2011; 26:535.
Article12. Porreco RP, Barkey R. Peripartum intensive care. J Matern Fetal Neonatal Med. 2010; 23:1136–8.
Article13. Cojocaru L, Turan OM, Levine A, Sollecito L, Williams S, Elsamadicy E, et al. Proning modus operandi in pregnancies complicated by acute respiratory distress syndrome secondary to COVID-19. J Matern Fetal Neonatal Med. 2022; 35:9043–52.
Article14. Beigmohammadi MT, Amoozadeh L, Rezaei Motlagh F, Rahimi M, Maghsoudloo M, Jafarnejad B, et al. Mortality predictive value of APACHE II and SOFA scores in COVID-19 patients in the intensive care unit. Can Respir J. 2022; 2022:5129314.
Article15. Suri J, Khanam Z. Prognosticating fetomaternal ICU outcomes. Indian J Crit Care Med. 2021; 25(Suppl 3):S206–22.
Article16. Khergade M, Suri J, Bharti R, Pandey D, Bachani S, Mittal P. Obstetric early warning score for prognostication of critically ill obstetric patient. Indian J Crit Care Med. 2020; 24:398–403.
Article17. Bellani G, Laffey JG, Pham T, Fan E, Brochard L, Esteban A, et al. Epidemiology, patterns of care, and mortality for patients with acute respiratory distress syndrome in intensive care units in 50 countries. JAMA. 2016; 315:788–800.
Article18. Aldawood A. Clinical characteristics and outcomes of critically ill obstetric patients: a ten-year review. Ann Saudi Med. 2011; 31:518–22.
Article19. Miller T, Emamian N, Glick Z, Chen N, Cao T, Buganu A, et al. Association between resuscitation in the critical care resuscitation unit and in-hospital mortality. Am J Emerg Med. 2022; 60:96–100.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Rehabilitation in Intensive Care Unit
- Transfer anxiety in parents of children transferred from pediatric intensive care units to general wards in South Korea: a hybrid concept analysis
- Analysis of the Nursing Interventions Performed by Hospital Nurses Using NIC
- Current Status and a Prospect of Neonatal Intensive Care Units in Korea
- The Analysis of High Risk Infant Patients Being Transferred to Neonatal Intensive Care Units in Korea