Clin Endosc.
2024 Mar;57(2):253-262. 10.5946/ce.2022.216.
Risk factors for recurrent stenosis after balloon dilation for benign hepaticojejunostomy anastomotic stricture
- Affiliations
-
- 1Department of Hepato-Biliary-Pancreatic Medicine, Cancer Institute Hospital of Japanese Foundation for Cancer Research, Tokyo, Japan
- KMID: 2553763
- DOI: http://doi.org/10.5946/ce.2022.216
Abstract
- Background/Aims
Hepaticojejunostomy anastomotic stricture (HJAS) is a feared adverse event associated with hepatopancreatobiliary surgery. Although balloon dilation for benign HJAS during endoscopic retrograde cholangiopancreatography with balloon-assisted enteroscopy has been reported to be useful, the treatment strategy remains controversial. Therefore, we evaluated the outcomes and risk factors of recurrent stenosis after balloon dilation alone for benign HJAS.
Methods
We retrospectively analyzed consecutive patients who underwent balloon-assisted enteroscopy–endoscopic retrograde cholangiopancreatography for benign HJAS at our institution between July 2014 and December 2020.
Results
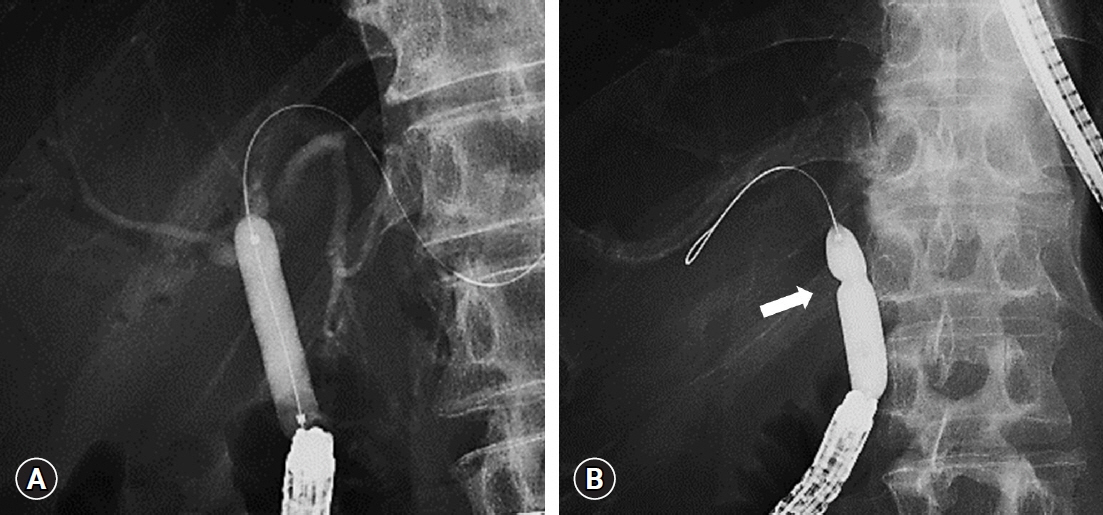
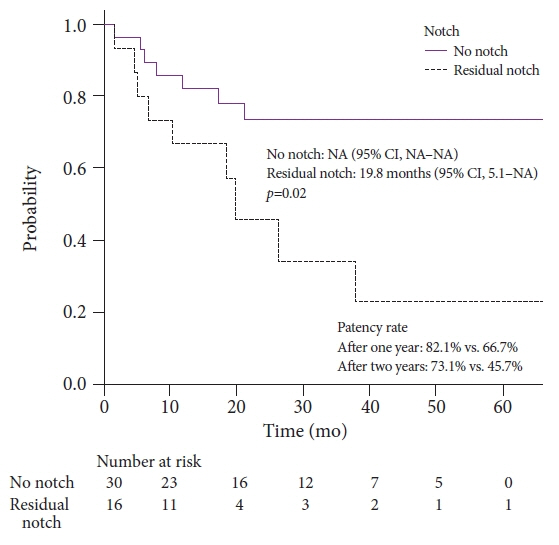
Forty-six patients were included, 16 of whom had recurrent HJAS after balloon dilation. The patency rates at 1 and 2 years after balloon dilation were 76.8% and 64.2%, respectively. Presence of a residual balloon notch during balloon dilation was an independent predictor of recurrence (hazard ratio, 2.80; 95% confidence interval, 1.01–7.78; p=0.048), whereas HJAS within postoperative 1 year tended to be associated with recurrence (hazard ratio, 2.43; 95% confidence interval, 0.85–6.89; p=0.096). The patency rates in patients without a residual balloon notch were 82.1% and 73.1% after 1 and 2 years, respectively.
Conclusions
Balloon dilation alone may be a viable option for patients with benign HJAS without residual balloon notches on fluoroscopy.
Keyword
Figure
Reference
-
1. House MG, Cameron JL, Schulick RD, et al. Incidence and outcome of biliary strictures after pancreaticoduodenectomy. Ann Surg. 2006; 243:571–578.2. Reid-Lombardo KM, Ramos-De la Medina A, Thomsen K, et al. Long-term anastomotic complications after pancreaticoduodenectomy for benign diseases. J Gastrointest Surg. 2007; 11:1704–1711.3. Dimou FM, Adhikari D, Mehta HB, et al. Incidence of hepaticojejunostomy stricture after hepaticojejunostomy. Surgery. 2016; 160:691–698.4. Primrose JN, Fox RP, Palmer DH, et al. Capecitabine compared with observation in resected biliary tract cancer (BILCAP): a randomised, controlled, multicentre, phase 3 study. Lancet Oncol. 2019; 20:663–673.5. Uesaka K, Boku N, Fukutomi A, et al. Adjuvant chemotherapy of S-1 versus gemcitabine for resected pancreatic cancer: a phase 3, open-label, randomised, non-inferiority trial (JASPAC 01). Lancet. 2016; 388:248–257.6. Conroy T, Hammel P, Hebbar M, et al. FOLFIRINOX or gemcitabine as adjuvant therapy for pancreatic cancer. N Engl J Med. 2018; 379:2395–2406.7. Motoi F, Kosuge T, Ueno H, et al. Randomized phase II/III trial of neoadjuvant chemotherapy with gemcitabine and S-1 versus upfront surgery for resectable pancreatic cancer (Prep-02/JSAP05). Jpn J Clin Oncol. 2019; 49:190–194.8. Ikeda M, Nakachi K, Konishi M, et al. Adjuvant S-1 versus observation in curatively resected biliary tract cancer: a phase III trial (JCOG1202: ASCOT). Jpn J Clin Oncol. 2022; 4_suppl:382.9. Inoue Y, Saiura A, Oba A, et al. Neoadjuvant gemcitabine and nab-paclitaxel for borderline resectable pancreatic cancers: intention-to-treat analysis compared with upfront surgery. J Hepatobiliary Pancreat Sci. 2021; 28:143–155.10. Tsutsumi K, Kato H, Yabe S, et al. A comparative evaluation of treatment methods for bile duct stones after hepaticojejunostomy between percutaneous transhepatic cholangioscopy and peroral, short double-balloon enteroscopy. Therap Adv Gastroenterol. 2017; 10:54–67.11. Shimatani M, Hatanaka H, Kogure H, et al. Diagnostic and therapeutic endoscopic retrograde cholangiography using a short-type double-balloon endoscope in patients with altered gastrointestinal anatomy: a multicenter prospective study in Japan. Am J Gastroenterol. 2016; 111:1750–1758.12. Tomoda T, Tsutsumi K, Kato H, et al. Outcomes of management for biliary stricture after living donor liver transplantation with hepaticojejunostomy using short-type double-balloon enteroscopy. Surg Endosc. 2016; 30:5338–5344.13. Itokawa F, Itoi T, Ishii K, et al. Single- and double-balloon enteroscopy-assisted endoscopic retrograde cholangiopancreatography in patients with Roux-en-Y plus hepaticojejunostomy anastomosis and Whipple resection. Dig Endosc. 2014; 26 Suppl 2:136–143.14. Shimatani M, Matsushita M, Takaoka M, et al. Effective “short” double-balloon enteroscope for diagnostic and therapeutic ERCP in patients with altered gastrointestinal anatomy: a large case series. Endoscopy. 2009; 41:849–854.15. Tsujino T, Yamada A, Isayama H, et al. Experiences of biliary interventions using short double-balloon enteroscopy in patients with Roux-en-Y anastomosis or hepaticojejunostomy. Dig Endosc. 2010; 22:211–216.16. Mizukawa S, Tsutsumi K, Kato H, et al. Endoscopic balloon dilatation for benign hepaticojejunostomy anastomotic stricture using short double-balloon enteroscopy in patients with a prior Whipple’s procedure: a retrospective study. BMC Gastroenterol. 2018; 18:14.17. Tomoda T, Kato H, Miyamoto K, et al. Comparison between endoscopic biliary stenting combined with balloon dilation and balloon dilation alone for the treatment of benign hepaticojejunostomy anastomotic stricture. J Gastrointest Surg. 2020; 24:1352–1358.18. Sato T, Kogure H, Nakai Y, et al. Endoscopic treatment of hepaticojejunostomy anastomotic strictures using fully-covered metal stents. Dig Endosc. 2021; 33:451–457.19. Tomoda T, Kato H, Ueki T, et al. Efficacy of double-balloon enteroscopy-assisted endoscopic balloon dilatation combined with stent deployment for hepaticojejunostomy anastomotic stricture. Dig Endosc. 2022; 34:604–611.20. Inoue T, Ibusuki M, Kitano R, et al. Balloon enteroscopy-assisted radial incision and cutting method for refractory hepaticojejunostomy anastomotic strictures. Endoscopy. 2019; 51:566–570.21. Lindström O, Udd M, Rainio M, et al. Benign biliary strictures treated with biodegradable stents in patients with surgically altered anatomy using double balloon enteroscopy. Scand J Gastroenterol. 2020; 55:1225–1233.22. Tsutsumi K, Kato H, Sakakihara I, et al. Dilation of a severe bilioenteric or pancreatoenteric anastomotic stricture using a Soehendra Stent Retriever. World J Gastrointest Endosc. 2013; 5:412–416.23. Sato T, Kogure H, Nakai Y, et al. Double-balloon endoscopy-assisted treatment of hepaticojejunostomy anastomotic strictures and predictive factors for treatment success. Surg Endosc. 2020; 34:1612–1620.24. Cotton PB, Eisen GM, Aabakken L, et al. A lexicon for endoscopic adverse events: report of an ASGE workshop. Gastrointest Endosc. 2010; 71:446–454.25. Kanda Y. Investigation of the freely available easy-to-use software ‘EZR’ for medical statistics. Bone Marrow Transplant. 2013; 48:452–458.26. Sato T, Kogure H, Nakai Y, et al. A prospective study of fully covered metal stents for different types of refractory benign biliary strictures. Endoscopy. 2020; 52:368–376.27. Mukund A, Rajesh S, Agrawal N, et al. Percutaneous management of resistant biliary-enteric anastomotic strictures with the use of a combined cutting and conventional balloon cholangioplasty protocol: a single-center experience. J Vasc Interv Radiol. 2015; 26:560–565.28. Winick AB, Waybill PN, Venbrux AC. Complications of percutaneous transhepatic biliary interventions. Tech Vasc Interv Radiol. 2001; 4:200–206.29. Ogura T, Okuda A, Higuchi K. Endoscopic ultrasound-guided hepaticogastrostomy for hepaticojejunostomy stricture using a one-step stent deployment technique (with video). J Hepatobiliary Pancreat Sci. 2021; 28:e34–e35.30. Pawa R, Jiang D, Gilliam J, et al. EUS-guided hepaticogastrostomy for management of cholangitis, hepatolithiasis, and anastomotic stricture after Roux-en-Y hepaticojejunostomy. VideoGIE. 2021; 6:225–227.31. Katanuma A, Hayashi T, Kin T, et al. Interventional endoscopic ultrasonography in patients with surgically altered anatomy: techniques and literature review. Dig Endosc. 2020; 32:263–274.32. Kühn JP, Busemann A, Lerch MM, et al. Percutaneous biliary drainage in patients with nondilated intrahepatic bile ducts compared with patients with dilated intrahepatic bile ducts. AJR Am J Roentgenol. 2010; 195:851–857.33. Morita S, Kitanosono T, Lee D, et al. Comparison of technical success and complications of percutaneous transhepatic cholangiography and biliary drainage between patients with and without transplanted liver. AJR Am J Roentgenol. 2012; 199:1149–1152.34. Chantarojanasiri T, Ratanachu-Ek T, Pausawasdi N. What you need to know before performing endoscopic ultrasound-guided hepaticogastrostomy. Clin Endosc. 2021; 54:301–308.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Use of a Cutting Balloon Dilation as a Rescue Therapy in Patients with Benign Bilioenteric Anastomotic Strictures Refractory to Conventional Balloon Dilation
- Clinical Outcomes of Dilation Therapy for Anastomotic Esophageal Stricture
- Fluoroscopically Guided Balloon Dilation for Benign Anastomotic Stricture in the Upper Gastrointestinal Tract
- Stricture Following Esophageal Reconstruction
- The Role of Endoscopic Balloon Dilation in the Treatment of Esophageal Strictures