Clin Endosc.
2024 Mar;57(2):226-236. 10.5946/ce.2023.128.
Double-guidewire technique for selective biliary cannulation does not increase the rate of post-endoscopic retrograde cholangiopancreatography pancreatitis in patients with naïve papilla
- Affiliations
-
- 1Department of Internal Medicine, Daegu Catholic University School of Medicine, Daegu, Korea
- KMID: 2553760
- DOI: http://doi.org/10.5946/ce.2023.128
Abstract
- Background/Aims
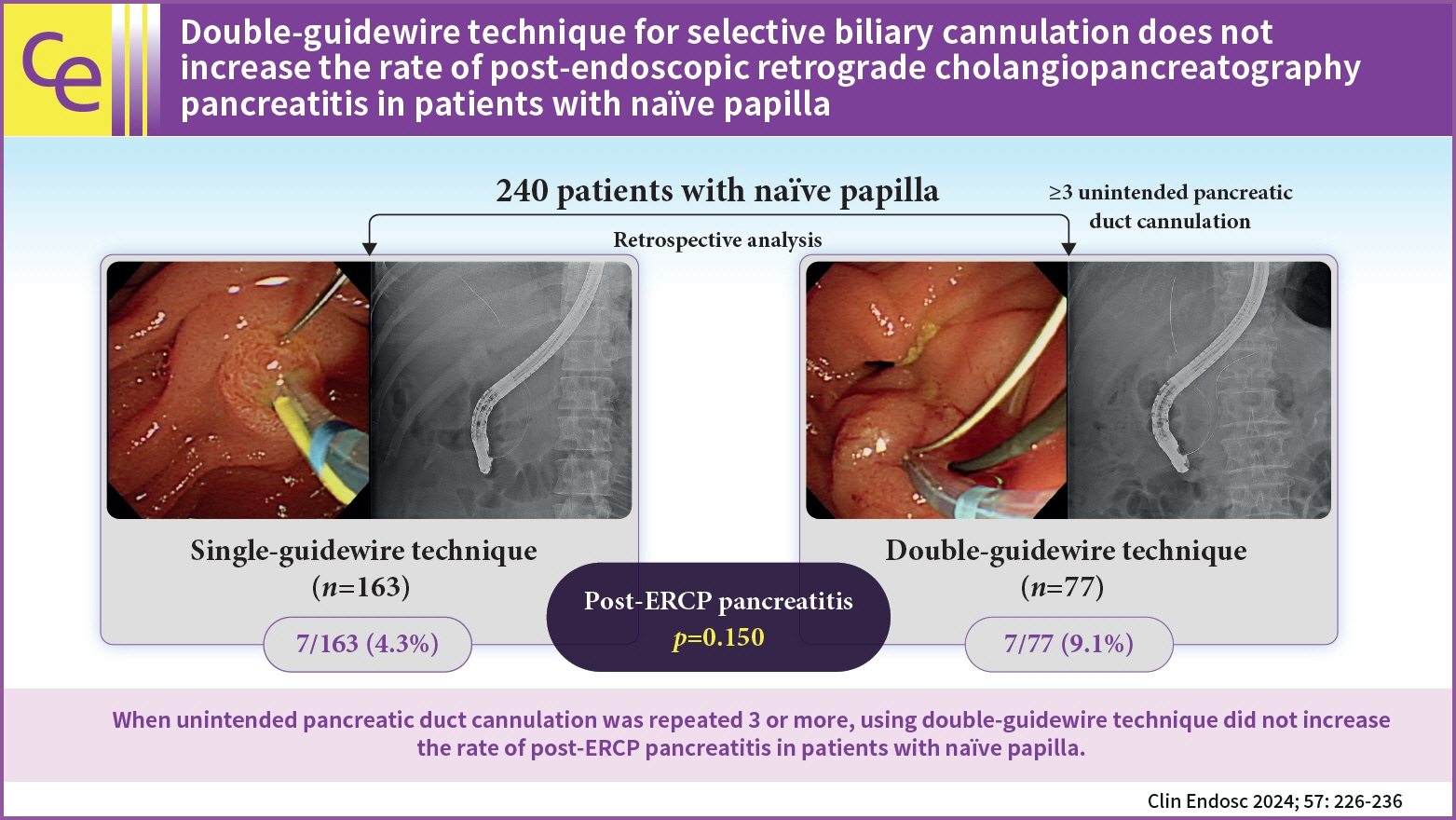
This study aimed to compare the safety of the double-guidewire technique (DGT) with that of the conventional single-guidewire technique (SGT) in real-world situations.
Methods
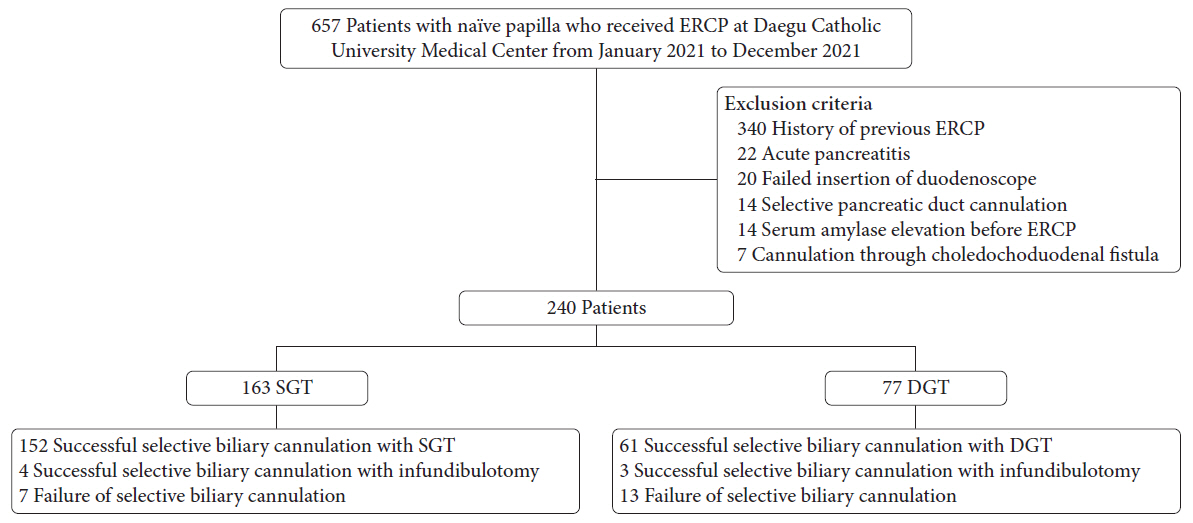
A total of 240 patients with naïve papilla who underwent endoscopic retrograde cholangiopancreatography (ERCP) at Daegu Catholic University Medical Center between January 2021 and December 2021 were included. The primary outcome was the rate of post-ERCP pancreatitis (PEP) in the SGT and DGT groups.
Results
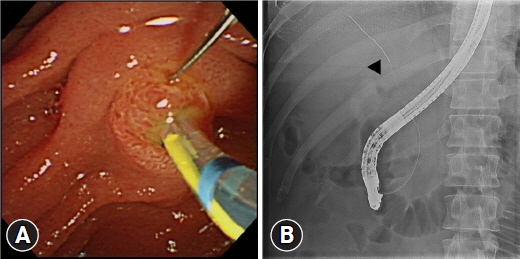
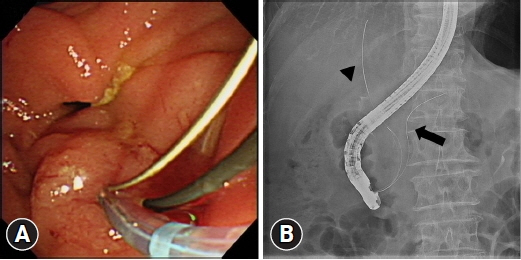
A total of 163 patients (67.9%) belonged to the SGT group, and 77 (32.1%) belonged to the DGT group. The rates of successful biliary cannulation were 95.7% and 83.1% in the SGT and DGT groups, respectively (p=0.002). In the study group, PEP occurred in 14 patients (5.8%). The PEP rates were not significantly different between the SGT and DGT groups (4.3% vs. 9.1%, p=0.150). In the multivariate analysis, the age of <50 years (odds ratio [OR], 9.305; 95% confidence interval [CI], 1.367–63.358; p=0.023) and hyperlipidemia (OR, 7.384; 95% CI, 1.103–49.424; p=0.039) were significant risk factors for PEP in the DGT group.
Conclusions
DGT did not increase the PEP rate in patients with naïve papilla. In addition, the age of <50 years and hyperlipidemia were significant risk factors for PEP in the DGT group.
Keyword
Figure
Reference
-
1. Testoni PA, Mariani A, Aabakken L, et al. Papillary cannulation and sphincterotomy techniques at ERCP: European Society of Gastrointestinal Endoscopy (ESGE) Clinical Guideline. Endoscopy. 2016; 48:657–683.2. Tse F, Yuan Y, Moayyedi P, et al. Guidewire-assisted cannulation of the common bile duct for the prevention of post-endoscopic retrograde cholangiopancreatography (ERCP) pancreatitis. Cochrane Database Syst Rev. 2012; 12:CD009662.3. Williams EJ, Taylor S, Fairclough P, et al. Are we meeting the standards set for endoscopy?: results of a large-scale prospective survey of endoscopic retrograde cholangio-pancreatograph practice. Gut. 2007; 56:821–829.4. Dumonceau JM, Devière J, Cremer M. A new method of achieving deep cannulation of the common bile duct during endoscopic retrograde cholangiopancreatography. Endoscopy. 1998; 30:S80.5. Maeda S, Hayashi H, Hosokawa O, et al. Prospective randomized pilot trial of selective biliary cannulation using pancreatic guide-wire placement. Endoscopy. 2003; 35:721–724.6. Tse F, Yuan Y, Moayyedi P, et al. Double-guidewire technique in difficult biliary cannulation for the prevention of post-ERCP pancreatitis: a systematic review and meta-analysis. Endoscopy. 2017; 49:15–26.7. Takenaka M, Kudo M. Usefulness of the double-guidewire technique for endoscopic procedures in the field of biliary and pancreatic diseases. Clin Endosc. 2022; 55:605–614.8. Laquière A, Privat J, Jacques J, et al. Early double-guidewire versus repeated single-guidewire technique to facilitate selective bile duct cannulation: a randomized controlled trial. Endoscopy. 2022; 54:120–127.9. Facciorusso A, Ramai D, Gkolfakis P, et al. Comparative efficacy of different methods for difficult biliary cannulation in ERCP: systematic review and network meta-analysis. Gastrointest Endosc. 2022; 95:60–71.10. Cotton PB, Lehman G, Vennes J, et al. Endoscopic sphincterotomy complications and their management: an attempt at consensus. Gastrointest Endosc. 1991; 37:383–393.11. Fugazza A, Troncone E, Amato A, et al. Difficult biliary cannulation in patients with distal malignant biliary obstruction: an underestimated problem? Dig Liver Dis. 2022; 54:529–536.12. Lee ES, Kim H. The prevention and management of post-ERCP pancreatitis. Korean J Pancreas Biliary Tract. 2016; 21:68–75.13. Wu CC, Lim SJ, Khor CJ. Endoscopic retrograde cholangiopancreatography-related complications: risk stratification, prevention, and management. Clin Endosc. 2023; 56:433–445.14. Sadeghi A, Jafari-Moghaddam R, Ataei S, et al. Role of vitamin C and rectal indomethacin in preventing and alleviating post-endoscopic retrograde cholangiopancreatography pancreatitis: a clinical study. Clin Endosc. 2023; 56:214–220.15. Arata S, Takada T, Hirata K, et al. Post-ERCP pancreatitis. J Hepatobiliary Pancreat Sci. 2010; 17:70–78.16. Dumonceau JM, Andriulli A, Deviere J, et al. European Society of Gastrointestinal Endoscopy (ESGE) guideline: prophylaxis of post-ERCP pancreatitis. Endoscopy. 2010; 42:503–515.17. Tryliskyy Y, Bryce GJ. Post-ERCP pancreatitis: pathophysiology, early identification and risk stratification. Adv Clin Exp Med. 2018; 27:149–154.18. Herreros de Tejada A, Calleja JL, Díaz G, et al. Double-guidewire technique for difficult bile duct cannulation: a multicenter randomized, controlled trial. Gastrointest Endosc. 2009; 70:700–709.19. Yang MJ, Hwang JC, Yoo BM, et al. Wire-guided cannulation over a pancreatic stent versus double guidewire technique in patients with difficult biliary cannulation. BMC Gastroenterol. 2015; 15:150.20. Dumonceau JM, Andriulli A, Elmunzer BJ, et al. Prophylaxis of post-ERCP pancreatitis: European Society of Gastrointestinal Endoscopy (ESGE) guideline: updated June 2014. Endoscopy. 2014; 46:799–815.21. Karr S. Epidemiology and management of hyperlipidemia. Am J Manag Care. 2017; 23(9 Suppl):S139–S148.22. Deng LH, Xue P, Xia Q, et al. Effect of admission hypertriglyceridemia on the episodes of severe acute pancreatitis. World J Gastroenterol. 2008; 14:4558–4561.23. Sbeit W, Khoury T. Fatty pancreas represents a risk factor for acute pancreatitis: a pilot study. Pancreas. 2021; 50:990–993.24. Hong W, Zimmer V, Basharat Z, et al. Association of total cholesterol with severe acute pancreatitis: a U-shaped relationship. Clin Nutr. 2020; 39:250–257.25. Socea B, Bolocan A, Bratu OG, et al. Hypercholesterolemia, as a predictor factor of severe acute pancreatitis. Mod Med. 2018; 25:219–222.26. Hong W, Zimmer V, Stock S, et al. Relationship between low-density lipoprotein cholesterol and severe acute pancreatitis (“the lipid paradox”). Ther Clin Risk Manag. 2018; 14:981–989.27. Vihervaara H, Salminen P, Hurme S, et al. Female gender and post-ERCP pancreatitis: is the association caused by difficult cannulation? Scand J Gastroenterol. 2011; 46:1498–1502.28. Freeman ML, DiSario JA, Nelson DB, et al. Risk factors for post-ERCP pancreatitis: a prospective, multicenter study. Gastrointest Endosc. 2001; 54:425–434.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Usefulness of the double-guidewire technique for endoscopic procedures in the field of biliary and pancreatic diseases
- Prevention of Post-endoscopic Retrograde Cholangiopancreatography Pancreatitis: An Endoscopic Perspective
- Optimal Use of Wire-Assisted Techniques and Precut Sphincterotomy
- Papillary Cannulation Facilitated by Submucosal Saline Injection into an Intradiverticular Papilla
- Endoclip-Assisted Cannulation for a Hidden Duodenal Papilla: Three Cases