Clin Endosc.
2022 Sep;55(5):605-614. 10.5946/ce.2022.032.
Usefulness of the double-guidewire technique for endoscopic procedures in the field of biliary and pancreatic diseases
- Affiliations
-
- 1Department of Gastroenterology and Hepatology, Kindai University Faculty of Medicine, Osakasayama, Japan
- KMID: 2533298
- DOI: http://doi.org/10.5946/ce.2022.032
Abstract
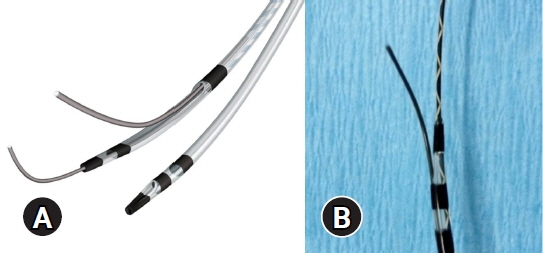
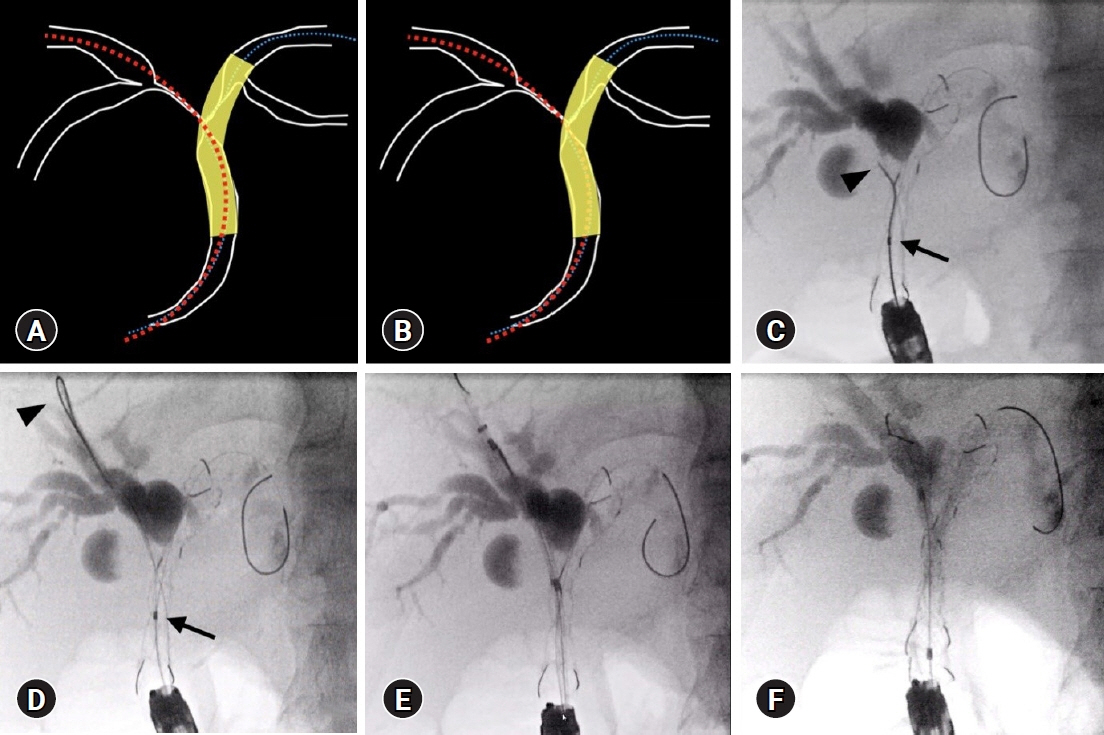
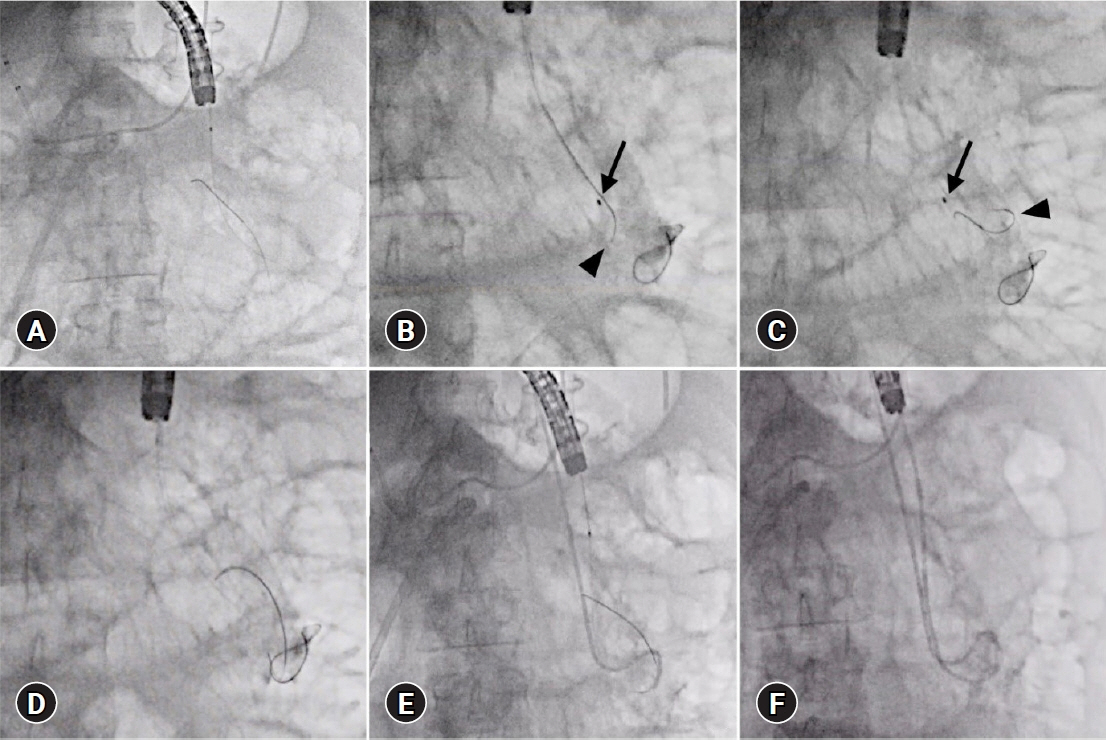
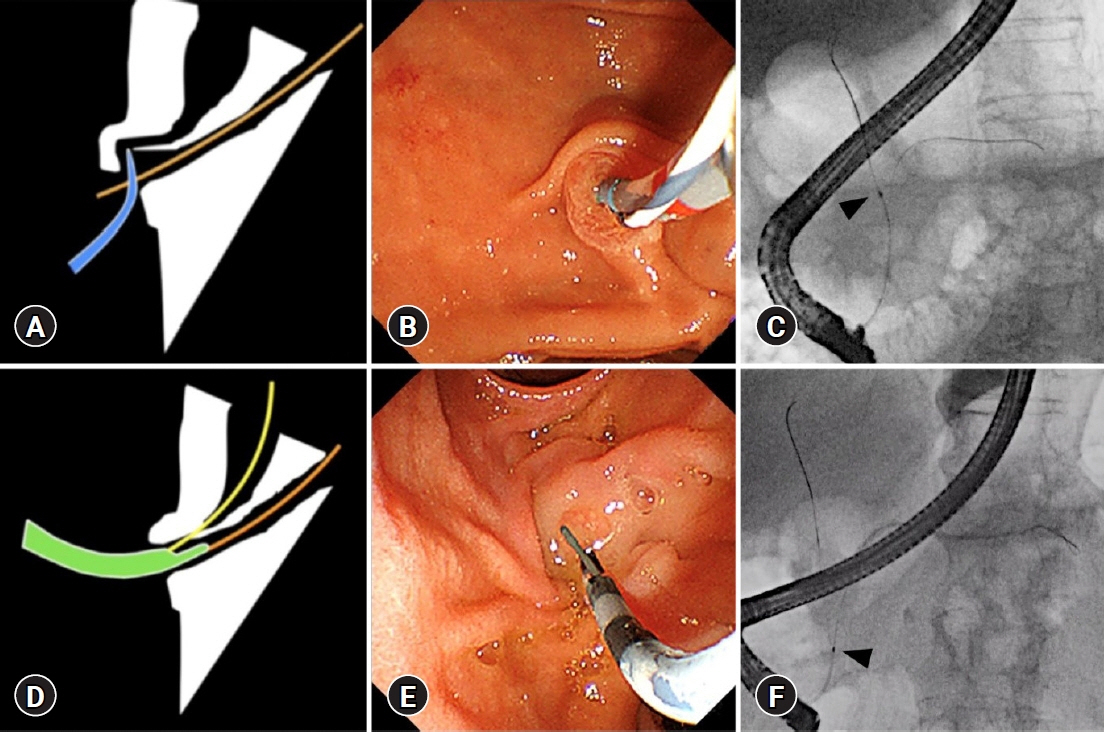
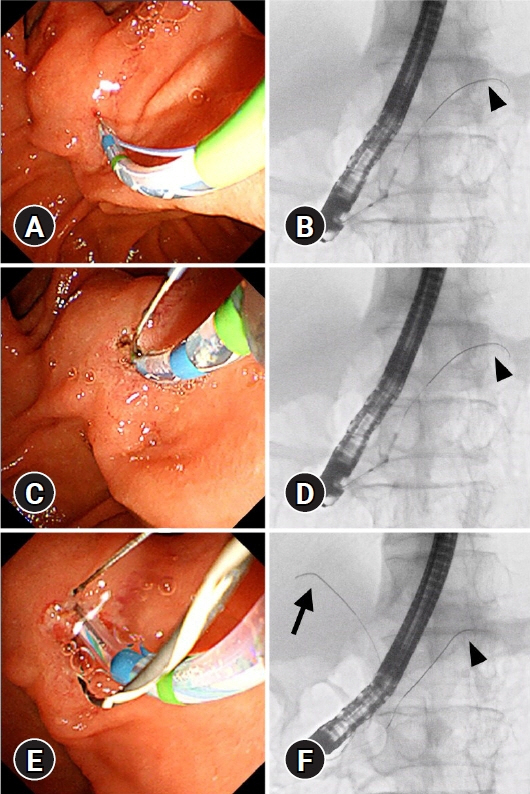
- The double-guidewire method has been increasingly used in endoscopic procedures for biliary and pancreatic diseases in recent years, including endoscopic retrograde cholangiopancreatography and endoscopic ultrasonography-related procedures. In addition, double-lumen catheters with uneven distal and proximal lumen openings have been introduced, making it possible to easily create a double-guidewire situation, and the usefulness of the double-guidewire technique using uneven double-lumen cannulas has been widely reported. Although the advantages of using two guidewires depend on the particular situation and the appropriate use of the two guidewires, deepening the knowledge of the double-guidewire method will contribute greatly to troubleshooting in daily practice. In this review, the usefulness of the double-guidewire technique is discussed with respect to two main areas: selective insertion of guidewires and devices and biliary cannulation.
Figure
Reference
-
1. Ogura T, Ueno S, Okuda A, et al. Experimental study of loop shape using 0.025-inch ERCP guidewires (with videos). Endosc Int Open. 2021; 9:E427–E437.2. Takenaka M, Yamazaki T, Otsuka Y, et al. Successful use of two guidewires with different properties using a double-lumen catheter for postoperative biliary stricture. Endoscopy. 2022; 54:E190–E192.3. Ogura T, Masuda D, Imoto A, et al. Double-guidewire technique using a novel ERCP cannula for hepatic hilar obstruction. Endoscopy. 2014; 46 Suppl 1 UCTN:E56–E57.4. Yasuda I, Takahashi K. Endoscopic management of walled-off pancreatic necrosis. Dig Endosc. 2021; 33:335–341.5. Ang TL, Teoh AY. Endoscopic ultrasonography-guided drainage of pancreatic fluid collections. Dig Endosc. 2017; 29:463–471.6. Bapaye A, Dubale NA, Sheth KA, et al. Endoscopic ultrasonography-guided transmural drainage of walled-off pancreatic necrosis: comparison between a specially designed fully covered bi-flanged metal stent and multiple plastic stents. Dig Endosc. 2017; 29:104–110.7. Consiglieri CF, Gornals JB, Busquets J, et al. Fluoroscopy-assisted vs fluoroless endoscopic ultrasound-guided transmural drainage of pancreatic fluid collections: a comparative study. Gastroenterol Hepatol. 2018; 41:12–21.8. Ge N, Hu J, Sun S, et al. Endoscopic ultrasound-guided pancreatic pseudocyst drainage with lumen-apposing metal stents or plastic double-pigtail stents: a multifactorial analysis. J Transl Int Med. 2017; 5:213–219.9. Siddiqui AA, Kowalski TE, Loren DE, et al. Fully covered self-expanding metal stents versus lumen-apposing fully covered self-expanding metal stent versus plastic stents for endoscopic drainage of pancreatic walled-off necrosis: clinical outcomes and success. Gastrointest Endosc. 2017; 85:758–765.10. Tamura T, Itonaga M, Tanioka K, et al. Radical treatment for walled-off necrosis: transmural nasocyst continuous irrigation. Dig Endosc. 2019; 31:307–315.11. van Santvoort HC, Besselink MG, Bakker OJ, et al. A step-up approach or open necrosectomy for necrotizing pancreatitis. N Engl J Med. 2010; 362:1491–1502.12. Bang JY, Varadarajulu S. Management of walled-off necrosis using the multiple transluminal gateway technique with the Hot AXIOS System. Dig Endosc. 2016; 28:103.13. Iwashita T, Iwasa Y, Shimizu M. Multiple transluminal gateway technique with transplantation of lumen-apposing metal stent for direct endoscopic necrosectomy in a patient with infected walled-off pancreatic necrosis. Dig Endosc. 2021; 33:e123–e124.14. Minaga K, Kitano M, Imai H, et al. Modified single transluminal gateway transcystic multiple drainage technique for a huge infected walled-off pancreatic necrosis: a case report. World J Gastroenterol. 2016; 22:5132–5136.15. Mukai S, Itoi T, Sofuni A, et al. Novel single transluminal gateway transcystic multiple drainages after EUS-guided drainage for complicated multilocular walled-off necrosis (with videos). Gastrointest Endosc. 2014; 79:531–535.16. Varadarajulu S, Phadnis MA, Christein JD, et al. Multiple transluminal gateway technique for EUS-guided drainage of symptomatic walled-off pancreatic necrosis. Gastrointest Endosc. 2011; 74:74–80.17. Itoi T, Itokawa F, Tsuchiya T, et al. EUS-guided pancreatic pseudocyst drainage: simultaneous placement of stents and nasocystic catheter using double-guidewire technique. Dig Endosc. 2009; 21 Suppl 1:S53–S56.18. Seewald S, Thonke F, Ang TL, et al. One-step, simultaneous double-wire technique facilitates pancreatic pseudocyst and abscess drainage (with videos). Gastrointest Endosc. 2006; 64:805–808.19. Ogura T, Higuchi K. Technical review of developments in endoscopic ultrasound-guided hepaticogastrostomy. Clin Endosc. 2021; 54:651–659.20. Ogura T, Higuchi K. Endoscopic ultrasound-guided hepaticogastrostomy: technical review and tips to prevent adverse events. Gut Liver. 2021; 15:196–205.21. Shiomi H, Masuda A, Kodama Y. Novel approach for successful endoscopic ultrasound-guided hepaticogastrostomy using a double-guidewire technique. Dig Endosc. 2019; 31:e50–e51.22. Mandai K, Uno K, Yasuda K. EUS-guided antegrade pancreatic guidewire placement for double-guidewire technique in single-balloon enteroscope-assisted ERCP. J Hepatobiliary Pancreat Sci. 2021; 28:e52–e53.23. Kawakami H, Kubota Y, Makiyama H, et al. Uneven double-lumen cannula for rescue guidewire technique in endoscopic ultrasonography-guided hepaticogastrostomy. Endoscopy. 2017; 49:E264–E265.24. Ishiwatari H, Satoh T, Sato J, et al. Double-guidewire technique facilitates endoscopic ultrasound-guided biliary drainage for hilar biliary obstruction. Endoscopy. 2019; 51:E321–E322.25. Nakai Y, Oyama H, Kanai S, et al. Double guidewire technique using an uneven double lumen catheter for endoscopic ultrasound-guided interventions. Dig Dis Sci. 2021; 66:1540–1547.26. Dumonceau JM, Devière J, Cremer M. A new method of achieving deep cannulation of the common bile duct during endoscopic retrograde cholangiopancreatography. Endoscopy. 1998; 30:S80.27. Angsuwatcharakon P, Rerknimitr R, Ridtitid W, et al. Success rate and cannulation time between precut sphincterotomy and double-guidewire technique in truly difficult biliary cannulation. J Gastroenterol Hepatol. 2012; 27:356–361.28. Cote GA, Mullady DK, Jonnalagadda SS, et al. Use of a pancreatic duct stent or guidewire facilitates bile duct access with low rates of precut sphincterotomy: a randomized clinical trial. Dig Dis Sci. 2012; 57:3271–3278.29. Eminler AT, Parlak E, Koksal AS, et al. Wire-guided cannulation over a pancreatic stent method increases the need for needle-knife precutting ın patients with difficult biliary cannulations. Gastrointest Endosc. 2019; 89:301–308.30. Herreros de Tejada A, Calleja JL, Díaz G, et al. Double-guidewire technique for difficult bile duct cannulation: a multicenter randomized, controlled trial. Gastrointest Endosc. 2009; 70:700–709.31. Kylanpaa L, Koskensalo V, Saarela A, et al. Transpancreatic biliary sphincterotomy versus double guidewire in difficult biliary cannulation: a randomized controlled trial. Endoscopy. 2021; 53:1011–1019.32. Laquiere A, Privat J, Jacques J, et al. Early double-guidewire versus repeated single-guidewire technique to facilitate selective bile duct cannulation: a randomized controlled trial. Endoscopy. 2022; 54:120–127.33. Maeda S, Hayashi H, Hosokawa O, et al. Prospective randomized pilot trial of selective biliary cannulation using pancreatic guide-wire placement. Endoscopy. 2003; 35:721–724.34. Sasahira N, Kawakami H, Isayama H, et al. Early use of double-guidewire technique to facilitate selective bile duct cannulation: the multicenter randomized controlled EDUCATION trial. Endoscopy. 2015; 47:421–429.35. Sugiyama H, Tsuyuguchi T, Sakai Y, et al. Transpancreatic precut papillotomy versus double-guidewire technique in difficult biliary cannulation: prospective randomized study. Endoscopy. 2018; 50:33–39.36. Yoo YW, Cha SW, Lee WC, et al. Double guidewire technique vs transpancreatic precut sphincterotomy in difficult biliary cannulation. World J Gastroenterol. 2013; 19:108–114.37. Takenaka M, Fujita T, Sugiyama D, et al. What is the most adapted indication of prophylactic pancreatic duct stent within the high-risk group of post-endoscopic retrograde cholangiopancreatography pancreatitis? Using the propensity score analysis. J Hepatobiliary Pancreat Sci. 2014; 21:275–280.38. Facciorusso A, Ramai D, Gkolfakis P, et al. Comparative efficacy of different methods for difficult biliary cannulation in ERCP: systematic review and network meta-analysis. Gastrointest Endosc. 2022; 95:60–71.39. Guzman-Calderon E, Martinez-Moreno B, Casellas JA, et al. Transpancreatic precut papillotomy versus double-guidewire technique in difficult biliary cannulation: a systematic review and meta-analysis. Endosc Int Open. 2021; 9:E1758–E1767.40. Tse F, Yuan Y, Moayyedi P, et al. Double-guidewire technique in difficult biliary cannulation for the prevention of post-ERCP pancreatitis: a systematic review and meta-analysis. Endoscopy. 2017; 49:15–26.41. Amer ME, Allam MA, Al-Sisi MH. Double guidewire technique versus transpancreatic sphincterotomy for difficult biliary cannulation. Egypt J Hosp Med. 2019; 74:764–770.42. Dumonceau JM, Kapral C, Aabakken L, et al. ERCP-related adverse events: European Society of Gastrointestinal Endoscopy (ESGE) Guideline. Endoscopy. 2020; 52:127–149.43. Wang X, Luo H, Luo B, et al. Combination prevention of post-endoscopic retrograde cholangiopancreatography pancreatitis in patients undergoing double-guidewire assisted biliary cannulation: a case-control study with propensity score matching. J Gastroenterol Hepatol. 2021; 36:1905–1912.44. Takenaka M, Arisaka Y, Sakai A, et al. A novel biliary cannulation method for difficult cannulation cases using a unique, uneven, double-lumen cannula (Uneven method). Endoscopy. 2018; 50:E229–E230.45. Takenaka M, Kawano K, Kawano R, et al. A novel method of papilla fixation for difficult biliary cannulation without using a pancreatic duct guidewire: non-guidewire fixation method. Endoscopy. 2022; 54:101–102.46. Takenaka M, Yamao K, Kudo M. Novel method of biliary cannulation for patients with Roux-en-Y anastomosis using a unique, uneven, double-lumen cannula (Uneven method). Dig Endosc. 2018; 30:808–809.47. Takenaka M, Minaga K, Kamata K, et al. Efficacy of a modified double-guidewire technique using an uneven double lumen cannula (uneven method) in patients with surgically altered gastrointestinal anatomy (with video). Surg Endosc. 2020; 34:1432–1441.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Optimal Use of Wire-Assisted Techniques and Precut Sphincterotomy
- Endoscopic ultrasound-guided portal vein coiling: troubleshooting interventional endoscopic ultrasonography
- Double-guidewire technique for selective biliary cannulation does not increase the rate of post-endoscopic retrograde cholangiopancreatography pancreatitis in patients with naïve papilla
- Guidewire Impaction in the Main Pancreatic Duct in a Patient with Chronic Pancreatitis: A Case Report
- A Selective Cannulation into the Common Bile Duct by a Guidewire Insertion through the Pancreatic Duct