J Korean Assoc Oral Maxillofac Surg.
2024 Feb;50(1):41-48. 10.5125/jkaoms.2024.50.1.41.
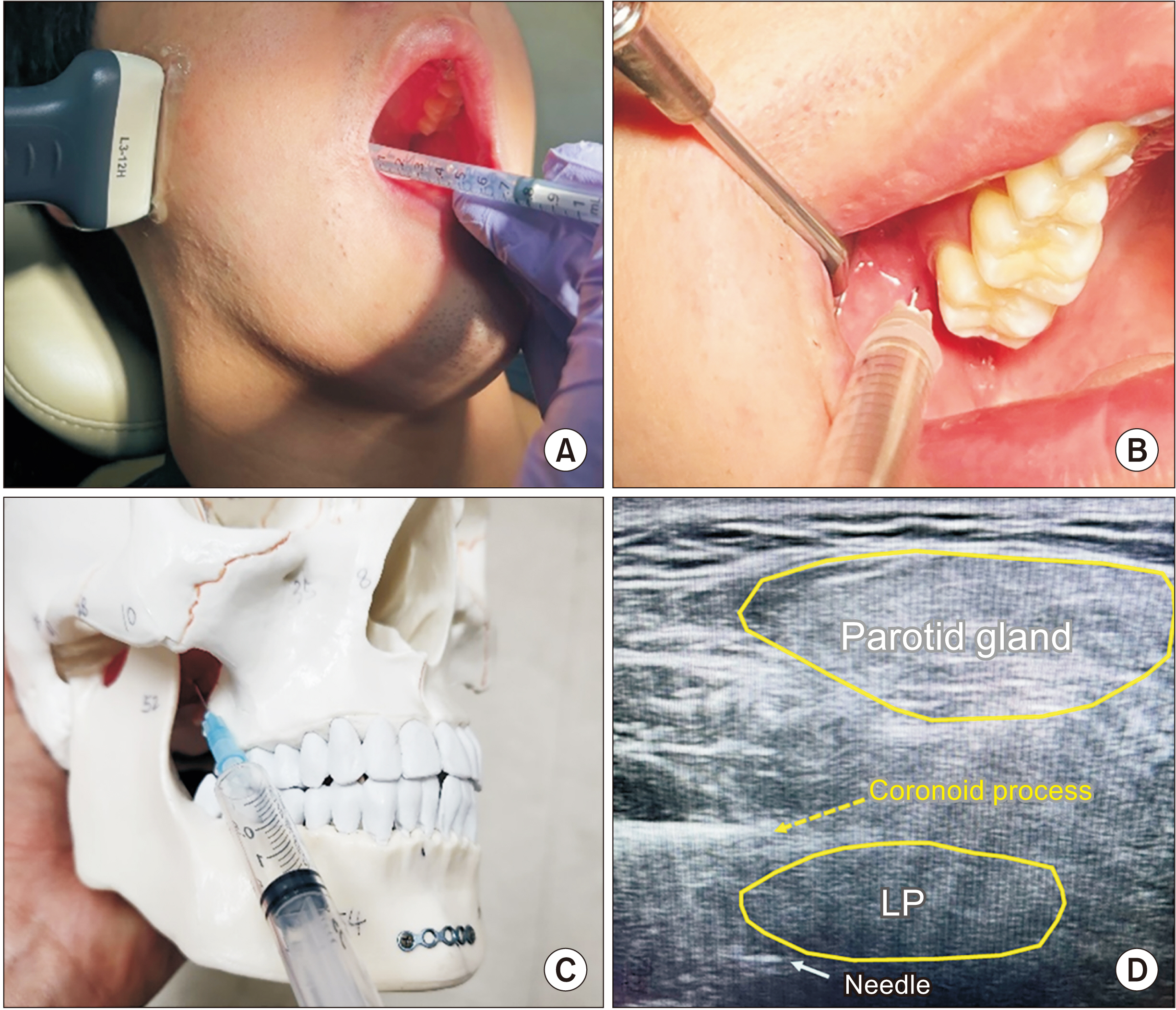
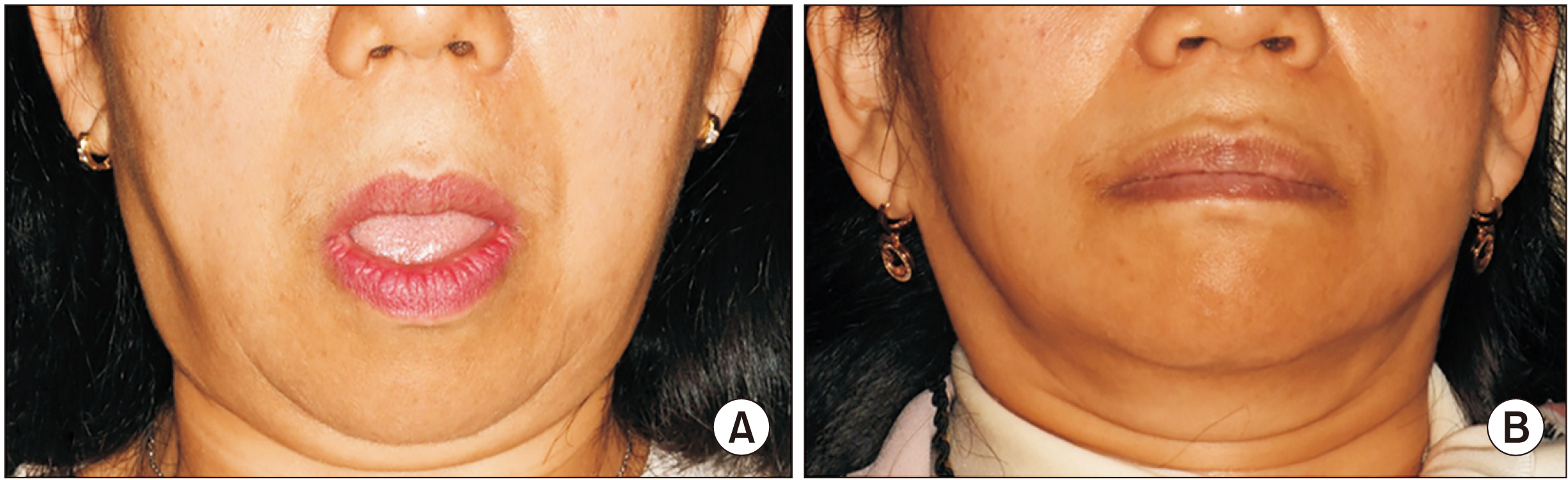
Ultrasound-guided intraoral botulinum toxin injection into the lateral pterygoid muscle for chronic temporomandibular joint dislocation
- Affiliations
-
- 1Department of Oral and Maxillofacial Surgery, School of Dentistry, Kyungpook National University, Daegu, Korea
- KMID: 2553661
- DOI: http://doi.org/10.5125/jkaoms.2024.50.1.41
Abstract
Objectives
Botulinum toxin type A (BTX), a powerful neurotoxin, can be an effective treatment choice for diverse muscular disorders and can reduce abnormal muscle activities. Abnormal movements of the mandible can be caused by involuntary and uncontrolled contractions of the lateral pterygoid muscle (LP) in various pathological situations. Previous reports have shown that BTX can reduce abnormal contractions of the LP. However, needle placement into the LP for BTX injection requires skill, experience, and sufficient anatomical knowledge. To place the needle precisely into the LP, ultrasonography (USG) can be used as an effective needle-guidance modality. USG is a non-invasive imaging modality able to create real-time images without any potential risks, including radiation exposure. Patients and Methods: The patients who had been performed USG-guided BTX injection into the LP using an intraoral approach were included in this study with a literature review and case presentations. Using the USG, four patients received BTX injections to treat recurrent temporomandibular dislocation and oromandibular dystonia resulting from involuntary LP activity. Result: Involuntary movements of the mandible were improved successfully in all patients, and showed satisfactory results without significant complication.
Conclusion
The intraoral approach could prevent potential complications during needle placement. USG-guided BTX injection is an effective, con-venient, and safe method that provides real-time imaging without unnecessary pain to the patient.
Keyword
Figure
Reference
-
References
1. Chen S. 2012; Clinical uses of botulinum neurotoxins: current indications, limitations and future developments. Toxins (Basel). 4:913–39. https://doi.org/10.3390/toxins4100913. DOI: 10.3390/toxins4100913. PMID: 23162705. PMCID: PMC3496996.
Article2. Altaweel AA, Elsayed SA, Baiomy AABA, Abdelsadek SE, Hyder AA. 2019; Extraoral versus intraoral botulinum toxin type A injection for management of temporomandibular joint disc displacement with reduction. J Craniofac Surg. 30:2149–53. https://doi.org/10.1097/scs.0000000000005658. DOI: 10.1097/SCS.0000000000005658. PMID: 31232992.
Article3. Reyes FI, Shoval HA, Tenaglia A, Kim H. 2022; Ultrasound-guided onabotulinumtoxinA injections to treat oromandibular dystonia in cerebral palsy. Toxins (Basel). 14:158. https://doi.org/10.3390/toxins14030158. DOI: 10.3390/toxins14030158. PMID: 35324655. PMCID: PMC8952419.
Article4. Hu Y, Zhang X, Liu S, Xu F. 2023; Ultrasound-guided vs conventional arthrocentesis for management of temporomandibular joint disorders: a systematic review and meta-analysis. Cranio. 41:264–73. https://doi.org/10.1080/08869634.2020.1829870. DOI: 10.1080/08869634.2020.1829870. PMID: 33044909.
Article5. Chen YJ, Chang PH, Chang KV, Wu WT, Özçakar L. 2018; Ultrasound guided injection for medial and lateral pterygoid muscles: a novel treatment for orofacial pain. Med Ultrason. 1:115–6. https://doi.org/10.11152/mu-1362. DOI: 10.11152/mu-1362. PMID: 29400381.
Article6. Fu KY, Chen HM, Sun ZP, Zhang ZK, Ma XC. 2010; Long-term efficacy of botulinum toxin type A for the treatment of habitual dislocation of the temporomandibular joint. Br J Oral Maxillofac Surg. 48:281–4. https://doi.org/10.1016/j.bjoms.2009.07.014. DOI: 10.1016/j.bjoms.2009.07.014. PMID: 19665263.
Article7. Guo HJ, Wu CC, Li TC. 2023; Ultrasound-guided lateral pterygoid muscle botulinum toxin: an injection for recurrent temporomandibular joint dislocation in a brain injury patient. Oral Maxillofac Surg. 27:365–71. https://doi.org/10.1007/s10006-022-01067-w. DOI: 10.1007/s10006-022-01067-w. PMID: 35486190.
Article8. Hallett M, Albanese A, Dressler D, Segal KR, Simpson DM, Truong D, et al. 2013; Evidence-based review and assessment of botulinum neurotoxin for the treatment of movement disorders. Toxicon. 67:94–114. https://doi.org/10.1016/j.toxicon.2012.12.004. DOI: 10.1016/j.toxicon.2012.12.004. PMID: 23380701.
Article9. Ünal S, Tugra Karaarslan-Turk F, Akbostanci MC, Peker E, Yilmaz R. 2022; Botulinum toxin injections in jaw-opening dystonia. The lateral pterygoid - maxillary artery problem. J Clin Neurosci. 101:217–20. https://doi.org/10.1016/j.jocn.2022.05.017. DOI: 10.1016/j.jocn.2022.05.017. PMID: 35636057.
Article10. Ottone NE, Sandoval C, Cid-Gutierrez P, Vásquez-Balboa ML, Tubbs RS, Fuentes R. 2021; Systematic review and meta-analysis of the anatomy of the maxillary artery using the Anatomical Quality Assurance (AQUA) checklist. Surg Radiol Anat. 43:1875–86. https://doi.org/10.1007/s00276-021-02825-3. DOI: 10.1007/s00276-021-02825-3. PMID: 34480213.
Article11. Yoshida K. 2018; Botulinum neurotoxin injection for the treatment of recurrent temporomandibular joint dislocation with and without neurogenic muscular hyperactivity. Toxins (Basel). 10:174. https://doi.org/10.3390/toxins10050174. DOI: 10.3390/toxins10050174. PMID: 29693593. PMCID: PMC5983230.
Article12. Moscovich M, Chen ZP, Rodriguez R. 2015; Successful treatment of open jaw and jaw deviation dystonia with botulinum toxin using a simple intraoral approach. J Clin Neurosci. 22:594–6. https://doi.org/10.1016/j.jocn.2014.08.027. DOI: 10.1016/j.jocn.2014.08.027. PMID: 25541097.
Article13. Casatuto T, Gosselin M, Lerhe B, Vandersteen C, Ehrmann E, Savoldelli C. 2021; In-house tooth-supported guide for the injection of botulinum toxin into the lateral pterygoid muscle using Blue Sky Plan software: a technical note. J Stomatol Oral Maxillofac Surg. 122:e77–80. https://doi.org/10.1016/j.jormas.2021.05.015. DOI: 10.1016/j.jormas.2021.05.015. PMID: 34157446.
Article14. Taema M, Nabi NA, Ibrahim S, Kamal HA, Emara A. 2021; Assessment of anterior positioning splint in conjunction with lateral pterygoid BTX injection to treat TMJ disc displacement with reduction - a preliminary report. Maxillofac Plast Reconstr Surg. 43:33. https://doi.org/10.1186/s40902-021-00317-3. DOI: 10.1186/s40902-021-00317-3. PMID: 34495418. PMCID: PMC8426453.
Article15. Oliveira AT, Camilo AA, Bahia PR, Carvalho AC, DosSantos MF, da Silva JV, et al. 2014; A novel method for intraoral access to the superior head of the human lateral pterygoid muscle. Biomed Res Int. 2014:432635. https://doi.org/10.1155/2014/432635. DOI: 10.1155/2014/432635. PMID: 24963484. PMCID: PMC4052112.
Article16. Yoshida K. 2018; Computer-aided design/computer-assisted manufacture-derived needle guide for injection of botulinum toxin into the lateral pterygoid muscle in patients with oromandibular dystonia. J Oral Facial Pain Headache. 32:e13–21. https://doi.org/10.11607/ofph.1955. DOI: 10.11607/ofph.1955. PMID: 29694466.
Article17. Ziegler CM, Haag C, Mühling J. 2003; Treatment of recurrent temporomandibular joint dislocation with intramuscular botulinum toxin injection. Clin Oral Investig. 7:52–5. https://doi.org/10.1007/s00784-002-0187-y. DOI: 10.1007/s00784-002-0187-y. PMID: 12673439.
Article18. Pons M, Meyer C, Euvrard E, Weber E, Sigaux N, Louvrier A. 2019; MR-guided navigation for botulinum toxin injection in the lateral pterygoid muscle. First results in the treatment of temporomandibular joint disorders. J Stomatol Oral Maxillofac Surg. 120:188–95. https://doi.org/10.1016/j.jormas.2018.11.002. DOI: 10.1016/j.jormas.2018.11.002. PMID: 30453102.
Article19. Maranini B, Ciancio G, Mandrioli S, Galiè M, Govoni M. 2022; The role of ultrasound in temporomandibular joint disorders: an update and future perspectives. Front Med (Lausanne). 9:926573. https://doi.org/10.3389/fmed.2022.926573. DOI: 10.3389/fmed.2022.926573. PMID: 35795636. PMCID: PMC9251198.
Article20. Daelen B, Thorwirth V, Koch A. 1997; [Neurogenic temporomandibular joint dislocation. Definition and therapy with botulinum toxin]. Nervenarzt. 68:346–50. German. https://doi.org/10.1007/s001150050135. DOI: 10.1007/s001150050135. PMID: 9273466.
Article21. Okeson JP. 2019. Management of temporomandibular disorders and occlusion. 8th ed. Elsevier.22. Liddell A, Perez DE. 2015; Temporomandibular joint dislocation. Oral Maxillofac Surg Clin North Am. 27:125–36. https://doi.org/10.1016/j.coms.2014.09.009. DOI: 10.1016/j.coms.2014.09.009. PMID: 25483448.
Article23. Balal M, Demirkiran M. 2023; Oromandibular dystonia: clinical and demographic data from eight-two patients. Tremor Other Hyperkinet Mov (N Y). 13:3. https://doi.org/10.5334/tohm.730. DOI: 10.5334/tohm.730. PMID: 36789171. PMCID: PMC9896995.
Article24. Jinnah HA. 2020; Medical and surgical treatments for dystonia. Neurol Clin. 38:325–48. https://doi.org/10.1016/j.ncl.2020.01.003. DOI: 10.1016/j.ncl.2020.01.003. PMID: 32279713. PMCID: PMC7156436.
Article25. Bhidayasiri R, Cardoso F, Truong DD. 2006; Botulinum toxin in blepharospasm and oromandibular dystonia: comparing different botulinum toxin preparations. Eur J Neurol. 13 Suppl 1:21–9. https://doi.org/10.1111/j.1468-1331.2006.01441.x. DOI: 10.1111/j.1468-1331.2006.01441.x. PMID: 16417594.
Article26. Tan EK, Jankovic J. 1999; Botulinum toxin A in patients with oromandibular dystonia: long-term follow-up. Neurology. 53:2102–7. https://doi.org/10.1212/wnl.53.9.2102. DOI: 10.1212/WNL.53.9.2102. PMID: 10599789.
Article27. Nastasi L, Mostile G, Nicoletti A, Zappia M, Reggio E, Catania S. 2016; Effect of botulinum toxin treatment on quality of life in patients with isolated lingual dystonia and oromandibular dystonia affecting the tongue. J Neurol. 263:1702–8. https://doi.org/10.1007/s00415-016-8185-1. DOI: 10.1007/s00415-016-8185-1. PMID: 27278063.
Article28. Jahngir MU, Ameer MA, Patel BC. Aboubakr S, Abu-Ghosh A, Adibi Sedeh P, Aeby TC, Aeddula NR, Agadi S, editors. 2023. Meige syndrome. StatPearls. StatPearls Publishing.29. Pandey S, Sharma S. 2017; Meigeʼs syndrome: history, epidemiology, clinical features, pathogenesis and treatment. J Neurol Sci. 372:162–70. https://doi.org/10.1016/j.jns.2016.11.053. DOI: 10.1016/j.jns.2016.11.053. PMID: 28017205.
Article30. Rosales RL, Ng AR, Santos MM, Fernandez HH. 2011; The broadening application of chemodenervation in X-linked dystonia-parkinsonism (part II): an open-label experience with botulinum toxin-A (Dysport®) injections for oromandibular, lingual, and truncal-axial dystonias. Int J Neurosci. 121 Suppl 1:44–56. https://doi.org/10.3109/00207454.2011.558260. DOI: 10.3109/00207454.2011.558260. PMID: 21348790.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Application of botulinum toxin in maxillofacial field: Part II. Wrinkle, intraoral ulcer, and cranio-maxillofacial pain
- A Child of Palatal Myoclonus Tinnitus Treated with Intraoral Injection of Botulinum Toxin
- Effect of bisphosphonate on temporomandibular joint in osteopenia-induced rats by botulinum toxin A injection on masticatory muscle: a preliminary study
- The Complications Developed after Repeated Botulinum Toxin Injection
- Accuracy of Ultrasound-Guided and Non-guided Botulinum Toxin Injection Into Neck Muscles Involved in Cervical Dystonia: A Cadaveric Study