J Korean Med Sci.
2024 Mar;39(8):e81. 10.3346/jkms.2024.39.e81.
Impact of Lactate Dehydrogenase and Hemoglobin Levels on Clinical Outcomes in Patients With Paroxysmal Nocturnal Hemoglobinuria: Results From the National Korean PNH Registry
- Affiliations
-
- 1Division of Hemato-oncology, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea
- 2Division of Hematology, Department of Internal Medicine, Severance Hospital, Yonsei University College of Medicine, Seoul, Korea
- 3IQVIA Solutions Asia Pte Ltd., Singapore
- 4IQVIA Solutions Hong Kong Ltd., Hong Kong SAR
- 5Alexion, AstraZeneca Rare Disease, Boston, MA, USA
- 6Division of Hematology, Seoul St. Mary’s Hospital, College of Medicine, The Catholic University of Korea, Seoul, Korea
- KMID: 2553330
- DOI: http://doi.org/10.3346/jkms.2024.39.e81
Abstract
- Background
Paroxysmal nocturnal hemoglobinuria (PNH) is a rare hematologic disorder caused by uncontrolled terminal complement activation, which leads to intravascular hemolysis (IVH), thromboembolism (TE), renal failure, and premature mortality.
Methods
We performed a secondary analysis of data collected from patients enrolled in the Korean National PNH Registry to assess the relative importance of risk factors, specifically lactate dehydrogenase (LDH) and hemoglobin (Hb), in predicting the incidence of TE, impaired renal function, and death in complement inhibitor-naïve patients with PNH.
Results
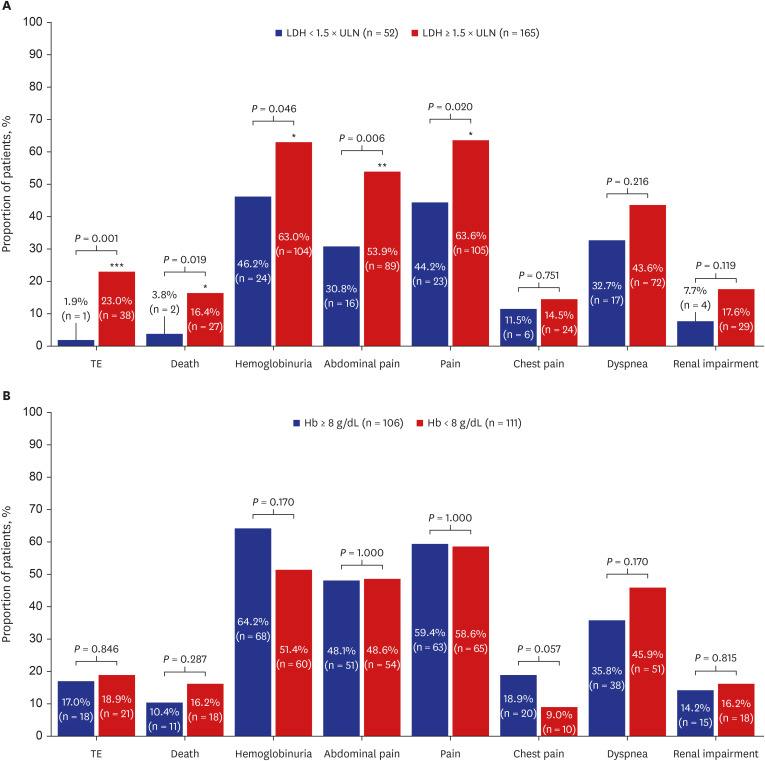
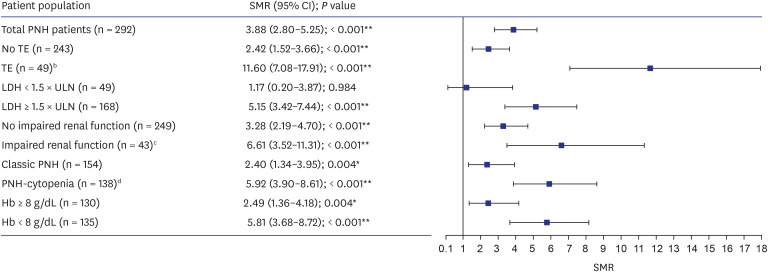
Multivariate regression modeling indicated that LDH ≥ 1.5 × upper limit of normal (ULN), male sex, and pain were associated with increased risk of TE (P = 0.016, 0.045, and 0.033, respectively), hemoglobinuria and pain were associated with an increased risk of impaired renal function (P = 0.034 and 0.022, respectively), and TE was associated with an increased incidence of death (P < 0.001). Hb < 8 g/dL was not a predictor of TE, impaired renal function, or death in multivariate regression analyses. Standardized mortality ratio analysis indicated that LDH ≥ 1.5 × ULN (P < 0.001), Hb < 8 g/dL (P < 0.001), and Hb ≥ 8 g/dL (P = 0.004) were all risk factors for death; in contrast, patients with LDH < 1.5 × ULN had similar mortality to the general population.
Conclusion
In complement inhibitor-naïve patients with PNH, LDH ≥ 1.5 × ULN was a significant predictor of TE, and TE was a significant predictor of death. Hb was not a significant predictor of TE, impaired renal function, or death. Therefore, controlling IVH will improve clinical outcomes for patients with PNH.
Figure
Reference
-
1. Parker C, Omine M, Richards S, Nishimura J, Bessler M, Ware R, et al. Diagnosis and management of paroxysmal nocturnal hemoglobinuria. Blood. 2005; 106(12):3699–3709. PMID: 16051736.2. Hillmen P, Lewis SM, Bessler M, Luzzatto L, Dacie JV. Natural history of paroxysmal nocturnal hemoglobinuria. N Engl J Med. 1995; 333(19):1253–1258. PMID: 7566002.3. Kulasekararaj AG, Brodsky RA, Nishimura JI, Patriquin CJ, Schrezenmeier H. The importance of terminal complement inhibition in paroxysmal nocturnal hemoglobinuria. Ther Adv Hematol. 2022; 13:20406207221091046. PMID: 35663504.4. Choi HJ, Lee SN. A clinical study on paroxysmal nocturnal hemoglobinuria in Korea. Ewha Med J. 1995; 18(3):189–197.5. Choi CW, Jang JH, Kim JS, Jo DY, Lee JH, Kim SH, et al. Efficacy of eculizumab in paroxysmal nocturnal hemoglobinuria patients with or without aplastic anemia: prospective study of a Korean PNH cohort. Blood Res. 2017; 52(3):207–211. PMID: 29043236.6. Kim JS, Jang JH, Jo DY, Ahn SY, Yoon SS, Lee JH, et al. Long-term efficacy and safety of eculizumab in patients with paroxysmal nocturnal hemoglobinuria and high disease burden: real-world data from Korea. J Korean Med Sci. 2023; 38(41):e328. PMID: 37873628.7. Kim YD, Yang JW, Choi JW, Kim BR, Yu JM, Kim YS, et al. Hemolytic crisis and acute kidney injury in patient with paroxysmal nocturnal hemoglobinuria in Korea – case report and review of literature. Korean J Nephrol. 2009; 28:236–242.8. Rother RP, Bell L, Hillmen P, Gladwin MT. The clinical sequelae of intravascular hemolysis and extracellular plasma hemoglobin: a novel mechanism of human disease. JAMA. 2005; 293(13):1653–1662. PMID: 15811985.9. Nishimura JI, Kanakura Y, Ware RE, Shichishima T, Nakakuma H, Ninomiya H, et al. Clinical course and flow cytometric analysis of paroxysmal nocturnal hemoglobinuria in the United States and Japan. Medicine (Baltimore). 2004; 83(3):193–207. PMID: 15118546.10. Schrezenmeier H, Muus P, Socié G, Szer J, Urbano-Ispizua A, Maciejewski JP, et al. Baseline characteristics and disease burden in patients in the International Paroxysmal Nocturnal Hemoglobinuria Registry. Haematologica. 2014; 99(5):922–929. PMID: 24488565.11. Socié G, Mary JY, de Gramont A, Rio B, Leporrier M, Rose C, et al. Paroxysmal nocturnal haemoglobinuria: long-term follow-up and prognostic factors. Lancet. 1996; 348(9027):573–577. PMID: 8774569.12. Kim JS, Lee JW, Kim BK, Lee JH, Chung J. The use of the complement inhibitor eculizumab (Soliris®) for treating Korean patients with paroxysmal nocturnal hemoglobinuria. Korean J Hematol. 2010; 45(4):269–274. PMID: 21253430.13. Hillmen P, Muus P, Dührsen U, Risitano AM, Schubert J, Luzzatto L, et al. Effect of the complement inhibitor eculizumab on thromboembolism in patients with paroxysmal nocturnal hemoglobinuria. Blood. 2007; 110(12):4123–4128. PMID: 17702897.14. Jang JH, Kim JS, Yoon SS, Lee JH, Kim YK, Jo DY, et al. Predictive factors of mortality in population of patients with paroxysmal nocturnal hemoglobinuria (PNH): results from a Korean PNH registry. J Korean Med Sci. 2016; 31(2):214–221. PMID: 26839475.15. Brodsky RA, Lee JW, Nishimura JI, Szer J. Lactate dehydrogenase versus haemoglobin: which one is the better marker in paroxysmal nocturnal haemoglobinuria? Br J Haematol. 2022; 196(2):264–265. PMID: 34923628.16. Brodsky RA. Paroxysmal nocturnal hemoglobinuria. Blood. 2014; 124(18):2804–2811. PMID: 25237200.17. Lee JW, Jang JH, Kim JS, Yoon SS, Lee JH, Kim YK, et al. Clinical signs and symptoms associated with increased risk for thrombosis in patients with paroxysmal nocturnal hemoglobinuria from a Korean Registry. Int J Hematol. 2013; 97(6):749–757. PMID: 23636668.18. Kim JS, Lee JW, Yoon SS, Lee JH, Jo DY, Jang JH, et al. Association between elevated hemolysis at diagnosis and early mortality and risk of thrombosis in paroxysmal nocturnal hemoglobinuria (PNH) patients with cytopenia. Blood. 2010; 116(21):4241.19. Lee JW, Jang JH, Kim JS, Yoon SS, Lee JH, Kim YK, et al. Uncontrolled complement activation and the resulting chronic hemolysis as measured by LDH serum level at diagnosis as predictor of thrombotic complications and mortality in a large cohort of patients with paroxysmal nocturnal hemoglobinuria (PNH). Blood. 2011; 118(21):3166.20. Astor BC, Muntner P, Levin A, Eustace JA, Coresh J. Association of kidney function with anemia: the Third National Health and Nutrition Examination Survey (1988-1994). Arch Intern Med. 2002; 162(12):1401–1408. PMID: 12076240.21. Westenbrink BD, Alings M, Connolly SJ, Eikelboom J, Ezekowitz MD, Oldgren J, et al. Anemia predicts thromboembolic events, bleeding complications and mortality in patients with atrial fibrillation: insights from the RE-LY trial. J Thromb Haemost. 2015; 13(5):699–707. PMID: 25683276.22. Chi G, Gibson CM, Hernandez AF, Hull RD, Kazmi SHA, Younes A, et al. Association of anemia with venous thromboembolism in acutely ill hospitalized patients: an APEX trial substudy. Am J Med. 2018; 131(8):972.e1–972.e7.23. Kim JS, Jang JH, Yoon SS, Lee JH, Kim YK, Jo DY, et al. Distinct subgroups of paroxysmal nocturnal hemoglobinuria (PNH) with cytopenia: results from South Korean National PNH Registry. Ann Hematol. 2016; 95(1):125–133. PMID: 26416513.24. Höchsmann B, de Fontbrune FS, Lee JW, Kulagin AD, Hillmen P, Wilson A, et al. Effect of eculizumab treatment in patients with paroxysmal nocturnal hemoglobinuria with or without high disease activity: real-world findings from the International Paroxysmal Nocturnal Hemoglobinuria Registry. Eur J Haematol. 2022; 109(3):197–204. PMID: 35390189.25. de Latour RH, Hill A, Füreder W, Piatek C, Griffin M, Ogawa M, et al. Ravulizumab reduces the risk of thrombosis in adult patients with paroxysmal nocturnal hemoglobinuria and high disease activity: 2-year data from a phase 3, open-label study. Hemasphere. 2021; 5(Suppl 2):109–110.26. Boehme AK, Pamboukian SV, George JF, Dillon C, Levitan EB, Griffin R, et al. Predictors of thromboembolic events in patients with ventricular assist device. ASAIO J. 2015; 61(6):640–647. PMID: 26418204.27. Gizzi M, Oberic L, Massard C, Poterie A, Le Teuff G, Loriot Y, et al. Predicting and preventing thromboembolic events in patients receiving cisplatin-based chemotherapy for germ cell tumours. Eur J Cancer. 2016; 69:151–157. PMID: 27821318.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Paroxysmal Nocturnal Hemoglobinuria Presenting as Recurrent Jejunitis
- Two Cases of Acute Renal Failure Complicating Paroxysmal Nocturnal Hemoglobinuria in Children
- Progressive Moyamoya Syndrome Associated with Paroxysmal Nocturnal Hemoglobinuria
- Anesthetic and Perioperative Management of Patient with Paroxysmal Nocturnal Hemoglobinuria
- The use of the complement inhibitor eculizumab (Soliris(R)) for treating Korean patients with paroxysmal nocturnal hemoglobinuria