Lab Med Online.
2023 Jan;13(1):36-41. 10.47429/lmo.2023.13.1.36.
Therapeutic Leukapheresis for Plasma Cell Leukemia Presenting with Hyperleukocytosis: The First Case in Korea
- Affiliations
-
- 1Department of Laboratory Medicine, Seoul National University Hospital, Seoul, Korea
- 2Department of Laboratory Medicine, Seoul National University College of Medicine, Seoul, Korea
- 3Department of Laboratory Medicine, Kangdong Sacred Heart Hospital, Seoul, Korea
- 4Department of Laboratory Medicine , Asan Medical Center, University of Ulsan College of Medicine, Seoul, Korea
- KMID: 2552723
- DOI: http://doi.org/10.47429/lmo.2023.13.1.36
Abstract
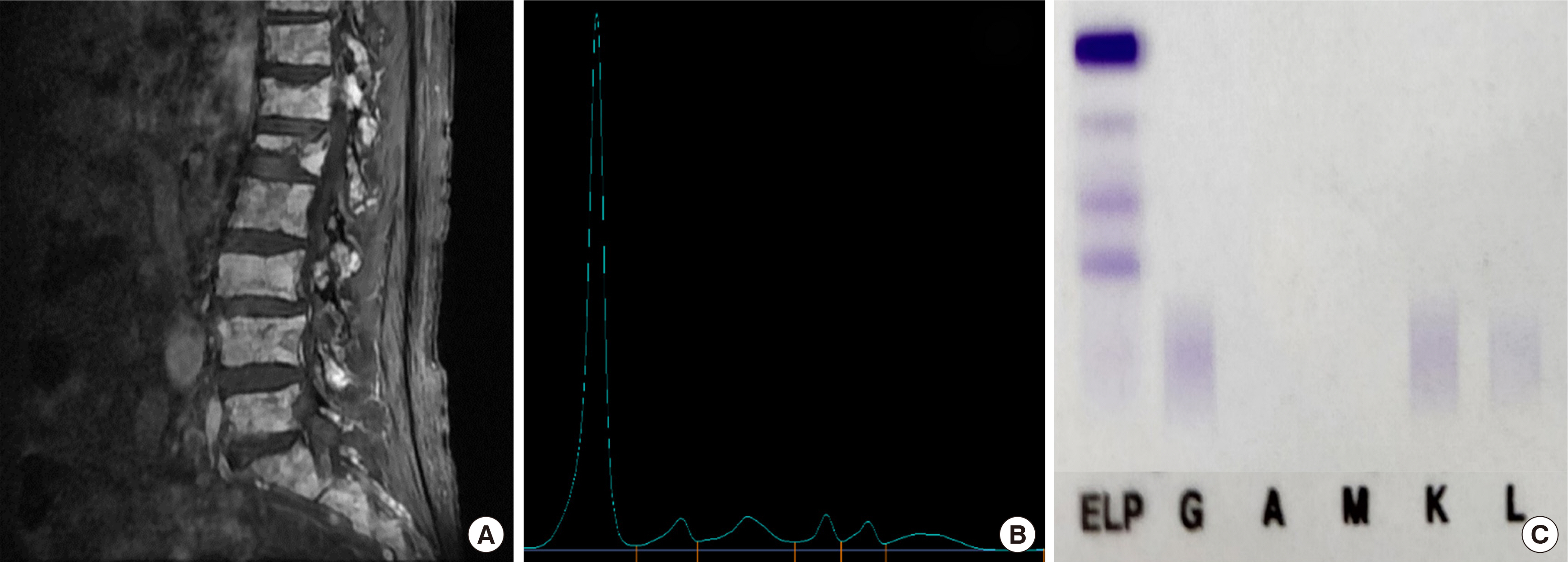
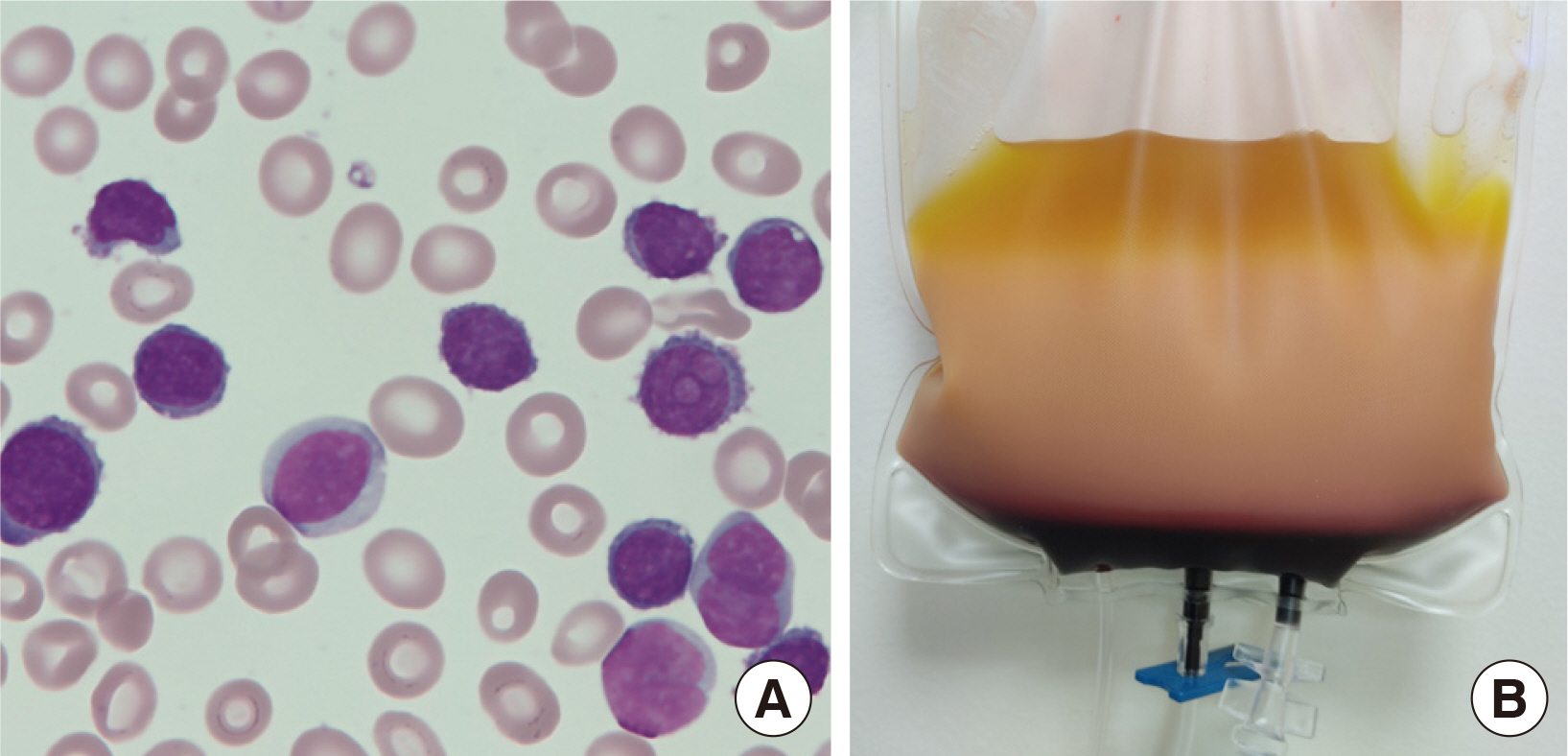
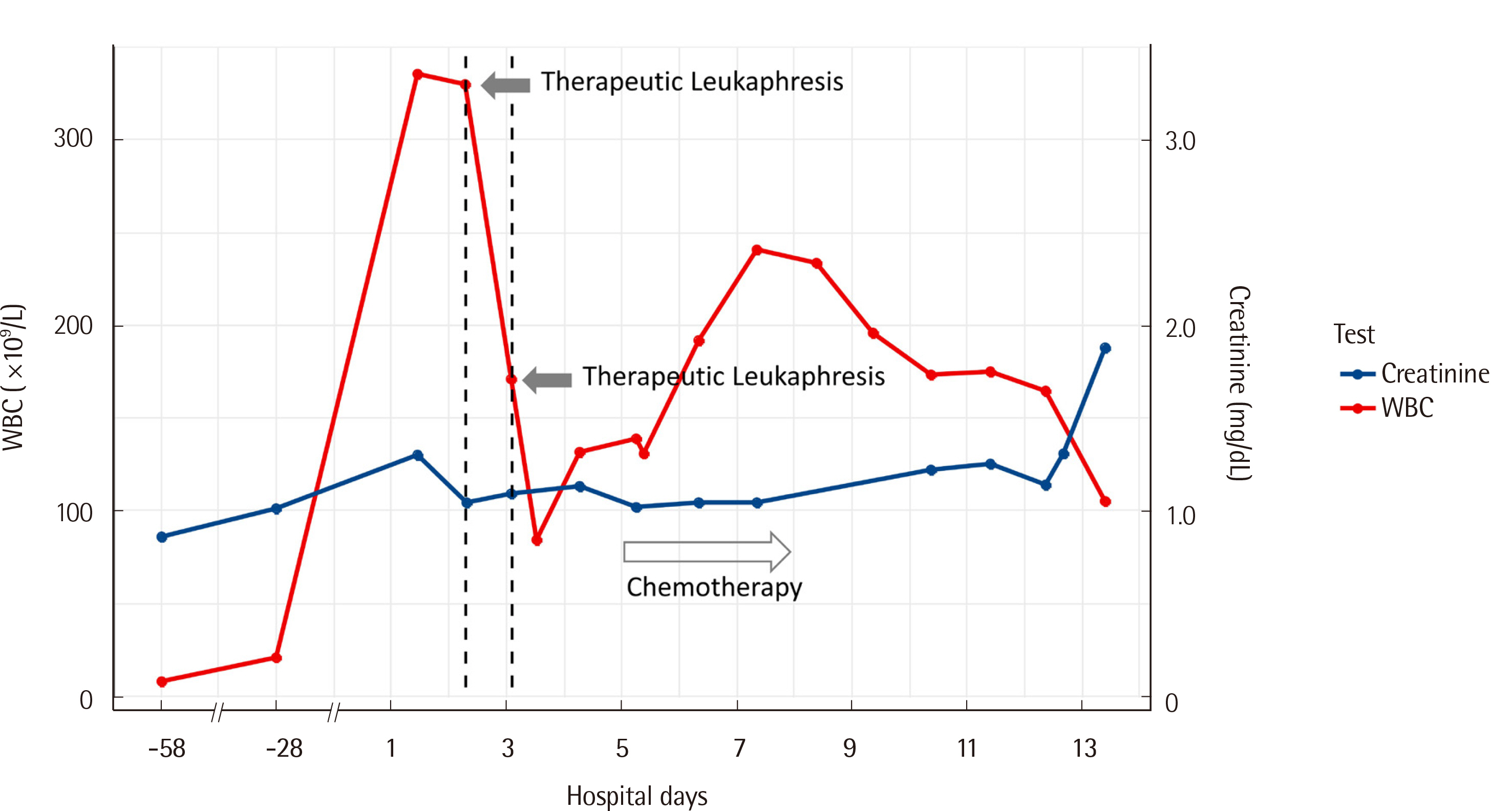
- Plasma cell leukemia (PCL) is a rare plasma cell disorder. Although therapeutic plasma exchange has reportedly been performed for hypergammaglobulinemia in PCL, there are no reports of therapeutic leukapheresis (TL) having been performed for hyperleukocytosis in Korea. Here, we report a rare case of TL performed for hyperleukocytosis in PCL with a literature review. A 78-year-old female patient was diagnosed and treated for nonsecretory myeloma 5 years ago before the present visit. She was diagnosed with secondary PCL 6 months ago after which her chemotherapy regimen was changed. The patient developed worsening dyspnea and memory loss one week before admission. She was hospitalized and two sessions of TL were performed to alleviate the symptoms caused by hyperleukocytosis (leukocyte count 335.60×10 9 /L, plasma cell 88%) and leukostasis. Although the leukocytes in peripheral blood were effectively removed (leukocyte count 171.29×10 9 /L, 48% reduction after first TL; leukocyte count 84.53×10 9 /L, 74% reduction after second TL), it was difficult to accurately assess whether the symptoms improved, owing to communication difficulties due to delirium. Although chemotherapy was administered, the patient died of multiple organ failure on the 13th day after admission. This case presented the highest leukocyte count among reports in the existing literature on rare cases of PCL with hyperleukocytosis. Although the patient eventually died, this is the first case of TL performed to successfully decrease leukocytes in PCL in Korea, presenting the potential for delaying the exacerbation of disease progression.
Figure
Reference
-
1. Fernández de Larrea C, Kyle RA, Durie BG, Ludwig H, Usmani S, Vesole DH, et al. 2013; Plasma cell leukemia: consensus statement on diagnostic requirements, response criteria and treatment recommendations by the International Myeloma Working Group. Leukemia. 27:780–91. DOI: 10.1038/leu.2012.336. PMID: 23288300. PMCID: PMC4112539.2. Sant M, Allemani C, Tereanu C, De Angelis R, Capocaccia R, Visser O, et al. 2010; Incidence of hematologic malignancies in Europe by morphologic subtype: results of the HAEMACARE project. Blood. 116:3724–34. DOI: 10.1182/blood-2010-05-282632. PMID: 20664057.3. Godbey EA, Dalton JB, Lai G, Sanford KW, Roseff SD. 2020; First reported case of leukocytapheresis in plasma cell leukemia. Transfusion. 60:11–2. DOI: 10.1111/trf.15564. PMID: 31682280.4. Noel P, Kyle RA. 1987; Plasma cell leukemia: An evaluation of response to therapy. Am J Med. 83:1062–8. DOI: 10.1016/0002-9343(87)90942-9. PMID: 3503574.5. Tuazon SA, Holmberg LA, Nadeem O, Richardson PG. 2021; A clinical perspective on plasma cell leukemia; current status and future directions. Blood Cancer J. 11:23. DOI: 10.1038/s41408-021-00414-6. PMID: 33563906. PMCID: PMC7873074.6. Granell M, Calvo X, Garcia-Guiñón A, Escoda L, Abella E, Martínez CM, et al. 2017; Prognostic impact of circulating plasma cells in patients with multiple myeloma: implications for plasma cell leukemia definition. Haematologica. 102:1099–104. DOI: 10.3324/haematol.2016.158303. PMID: 28255016. PMCID: PMC5451342.7. Ravi P, Kumar SK, Roeker L, Gonsalves W, Buadi F, Lacy MQ, et al. 2018; Revised diagnostic criteria for plasma cell leukemia: results of a Mayo Clinic study with comparison of outcomes to multiple myeloma. Blood Cancer J. 8:116. DOI: 10.1038/s41408-018-0140-1. PMID: 30442928. PMCID: PMC6238010.8. Ramsingh G, Mehan P, Luo J, Vij R, Morgensztern D. 2009; Primary plasma cell leukemia: a Surveillance, Epidemiology, and End Results database analysis between 1973 and 2004. Cancer. 115:5734–9. DOI: 10.1002/cncr.24700. PMID: 19877113.9. Okafor C, Ward DM, Mokrzycki MH, Weinstein R, Clark P, Balogun RA. 2010; Introduction and overview of therapeutic apheresis. J Clin Apher. 25:240–9. DOI: 10.1002/jca.20247. PMID: 20806281.10. Padmanabhan A, Connelly-Smith L, Aqui N, Balogun RA, Klingel R, Meyer E, et al. 2019; Guidelines on the Use of Therapeutic Apheresis in Clinical Practice - Evidence-Based Approach from the Writing Committee of the American Society for Apheresis: The Eighth Special Issue. J Clin Apher. 34:171–354. DOI: 10.1002/jca.21705. PMID: 31180581.11. Kwaan HC. 2013; Hyperviscosity in plasma cell dyscrasias. Clin Hemorheol Microcirc. 55:75–83. DOI: 10.3233/CH-131691. PMID: 23455837.12. Mehta J, Singhal S. 2003; Hyperviscosity syndrome in plasma cell dyscrasias. Semin Thromb Hemost. 29:467–71. DOI: 10.1055/s-2003-44554. PMID: 14631546.13. Kosmo MA, Gale RP. 1988; Plasma cell leukemia with IgA paraproteinemia and hyperviscosity. Am J Hematol. 28:113–5. DOI: 10.1002/ajh.2830280210. PMID: 3394712.14. Geraci JM, Hansen RM, Kueck BD. 1990; Plasma cell leukemia and hyperviscosity syndrome. South Med J. 83:800–5. DOI: 10.1097/00007611-199007000-00020. PMID: 2196691.15. Giammarco S, Chiusolo P, Piccirillo N, Di Giovanni A, Metafuni E, Laurenti L, et al. 2017; Hyperleukocytosis and leukostasis: management of a medical emergency. Expert Rev Hematol. 10:147–54. DOI: 10.1080/17474086.2017.1270754. PMID: 27967252.16. Pagano L, Valentini CG, De Stefano V, Venditti A, Visani G, Petrucci MT, et al. 2011; Primary plasma cell leukemia: a retrospective multicenter study of 73 patients. Ann Oncol. 22:1628–35. DOI: 10.1093/annonc/mdq646. PMID: 21252060.17. Jurczyszyn A, Radocha J, Davila J, Fiala MA, Gozzetti A, Grząśko N, et al. 2018; Prognostic indicators in primary plasma cell leukaemia: a multicentre retrospective study of 117 patients. Br J Haematol. 180:831–9. DOI: 10.1111/bjh.15092. PMID: 29315478.18. Jurczyszyn A, Castillo JJ, Avivi I, Czepiel J, Davila J, Vij R, et al. 2019; Secondary plasma cell leukemia: a multicenter retrospective study of 101 patients. Leuk Lymphoma. 60:118–23. DOI: 10.1080/10428194.2018.1473574. PMID: 29965787.19. Moiz B, Ali SS. 2012; Plasma cell leukemia in pregnancy. Blood. 120:3633. DOI: 10.1182/blood-2012-04-425074. PMID: 23281530.20. Rastogi P, Ahluwalia J, Parathan KK, Malhotra P. 2017; Plasma cell leukemia presenting with hyperleukocytosis and anaplasia. Indian J Hematol Blood Transfus. 33:128–9. DOI: 10.1007/s12288-016-0740-5. PMID: 28194071. PMCID: PMC5280869.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Therapeutic Leukapheresis for Acute Lymphoblastic Leukemia with Severe Hyperleukocytosis in a Six-Week-Old Infant (4.7 kg)
- Therapeutic Leukapheresis for the Management of Hyperleukocytosis: Ten-year Experience in a Tertiary Care Hospital
- Leukapheresis with high dose hydroxyurea in the management of lower leg artery obstruction in Chronic Myelogenous Leukemia
- Evaluation of therapeutic leukapheresis in hyperleukocytic leukemias
- Clinical Effects and Safety of Therapeutic Leukapheresis in Hyperleukocytosis