Brain Tumor Res Treat.
2024 Jan;12(1):75-79. 10.14791/btrt.2023.0044.
Awake Surgery for Angiocentric Glioma in the Eloquent Area in an Adolescent: A Case Report
- Affiliations
-
- 1Departments of Neurosurgery , Nara Medical University, Kashihara, Japan
- 2Department of Neurosurgery, Ohnishi Neurologic Center, Akashi, Japan
- 3Departments of Diagnostic Pathology, Nara Medical University, Kashihara, Japan
- KMID: 2552344
- DOI: http://doi.org/10.14791/btrt.2023.0044
Abstract
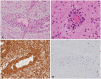
- Angiocentric glioma (AG) is an extremely rare tumor that often develops in adolescents. Awake surgery for AG occurring in the eloquent area has not been reported to date. We report a case involving a righthanded 15-year-old boy with AG. He presented with a first-time generalized tonic-clonic seizure and was rushed to the local hospital. CT of the head indicated a left frontal low-density mass with no calcification. He was subsequently referred to our hospital. Comparison with a CT scan obtained two years prior due to mild head trauma indicated that the lesion showed a trend toward enlargement. The lesion was located in the anterior and lateral portions of the primary motor cortex, and MRI showed homogenous hypointensity on T1-weighted and hyperintensity on T2-weighted images. Contrast-enhanced MRI showed a linear contrast effect. The patient underwent awake surgery with successful intraoperative brain mapping and total resection, and brain function was preserved. Pathological analysis revealed AG. He returned to his normal life and has shown no recurrence without additional treatment for 2 years. Thus, awake surgery for complete tumor resection while preserving brain function is effective and safe even in adolescents with AGs.
Keyword
Figure
Reference
-
1. Han G, Zhang J, Ma Y, Gui Q, Yin S. Clinical characteristics, treatment and prognosis of angiocentric glioma. Oncol Lett. 2020; 20:1641–1648. PMID: 32724405.
Article2. Fernández Coello A, Moritz-Gasser S, Martino J, Martinoni M, Matsuda R, Duffau H. Selection of intraoperative tasks for awake mapping based on relationships between tumor location and functional networks. J Neurosurg. 2013; 119:1380–1394. PMID: 24053503.
Article3. Matsuda R, Moritz-Gasser S, Duvaux S, Fernández Coello A, Martinoni M, Duffau H. The persistent crucial role of the left hemisphere for language in left-handers with a left low grade glioma: a stimulation mapping study. Acta Neurochir (Wien). 2014; 156:661–670. discussion 670. PMID: 24452594.
Article4. Matsuda R, Coello AF, De Benedictis A, Martinoni M, Duffau H. Awake mapping for resection of cavernous angioma and surrounding gliosis in the left dominant hemisphere: surgical technique and functional results: clinical article. J Neurosurg. 2012; 117:1076–1081. PMID: 23039148.
Article5. Matsuda R, Tamura K, Nishimura F, Nakagawa I, Motoyama Y. Subcortical calculation mapping during parietal glioma surgery in the dominant hemisphere: a case report. World Neurosurg. 2019; 121:205–210. PMID: 30326305.
Article6. Wang M, Tihan T, Rojiani AM, Bodhireddy SR, Prayson RA, Iacuone JJ, et al. Monomorphous angiocentric glioma: a distinctive epileptogenic neoplasm with features of infiltrating astrocytoma and ependymoma. J Neuropathol Exp Neurol. 2005; 64:875–881. PMID: 16215459.
Article7. Lellouch-Tubiana A, Boddaert N, Bourgeois M, Fohlen M, Jouvet A, Delalande O, et al. Angiocentric neuroepithelial tumor (ANET): a new epilepsy-related clinicopathological entity with distinctive MRI. Brain Pathol. 2005; 15:281–286. PMID: 16389940.
Article8. Louis DN, Perry A, Reifenberger G, von Deimling A, Figarella-Branger D, Cavenee WK, et al. The 2016 World Health Organization classification of tumors of the central nervous system: a summary. Acta Neuropathol. 2016; 131:803–820. PMID: 27157931.
Article9. Louis DN, Perry A, Wesseling P, Brat DJ, Cree IA, Figarella-Branger D, et al. The 2021 WHO classification of tumors of the central nervous system: a summary. Neuro Oncol. 2021; 23:1231–1251. PMID: 34185076.
Article10. Chaudhari JP, Kothari KS, Pandya TP, Goel NA. Angiocentric glioma: report of a rare case presenting with psychosis. Asian J Neurosurg. 2018; 13:1186–1192. PMID: 30459891.
Article11. Lohkamp LN, Beuriat PA, Desmurget M, Cristofori I, Szathmari A, Huguet L, et al. Awake brain surgery in children-a single-center experience. Childs Nerv Syst. 2020; 36:967–974. PMID: 32055975.
Article12. Collée E, Satoer D, Wegener Sleeswijk B, Klimek M, Smits M, Van Veelen ML, et al. Language improvement after awake craniotomy in a 12-year-old child: illustrative case. J Neurosurg Case Lessons. 2022; 3:CASE2293. PMID: 35733631.
Article13. O’Leary KD, Philippopoulos AJ, Koslofsky A, Ahmed Y. How often do awake craniotomies in children and adolescents lead to panic and worry? Childs Nerv Syst. 2023; 08. 23. DOI: 10.1007/s00381-023-06117-6. [Epub].
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Surgical Experience of An Arteriovenous Malformation in an Eloquent Motor Area
- A Case of Angiocentric Glioma with Unusual Clinical and Radiological Features
- Awake Craniotomy and Intraoperative Musical Performance for Brain Tumor Surgery: Case Report and Literature Review
- Anesthetic considerations for awake craniotomy
- Solitary Primary Leptomeningeal Glioma: Case Report