Int J Stem Cells.
2024 Feb;17(1):38-50. 10.15283/ijsc23146.
Unleashing the Power of Undifferentiated Induced Pluripotent Stem Cell Bioprinting: Current Progress and Future Prospects
- Affiliations
-
- 1Department of Biopharmaceutical Convergence, Sungkyunkwan University, Suwon, Korea
- 2School of Pharmacy, Sungkyunkwan University, Suwon, Korea
- KMID: 2552016
- DOI: http://doi.org/10.15283/ijsc23146
Abstract
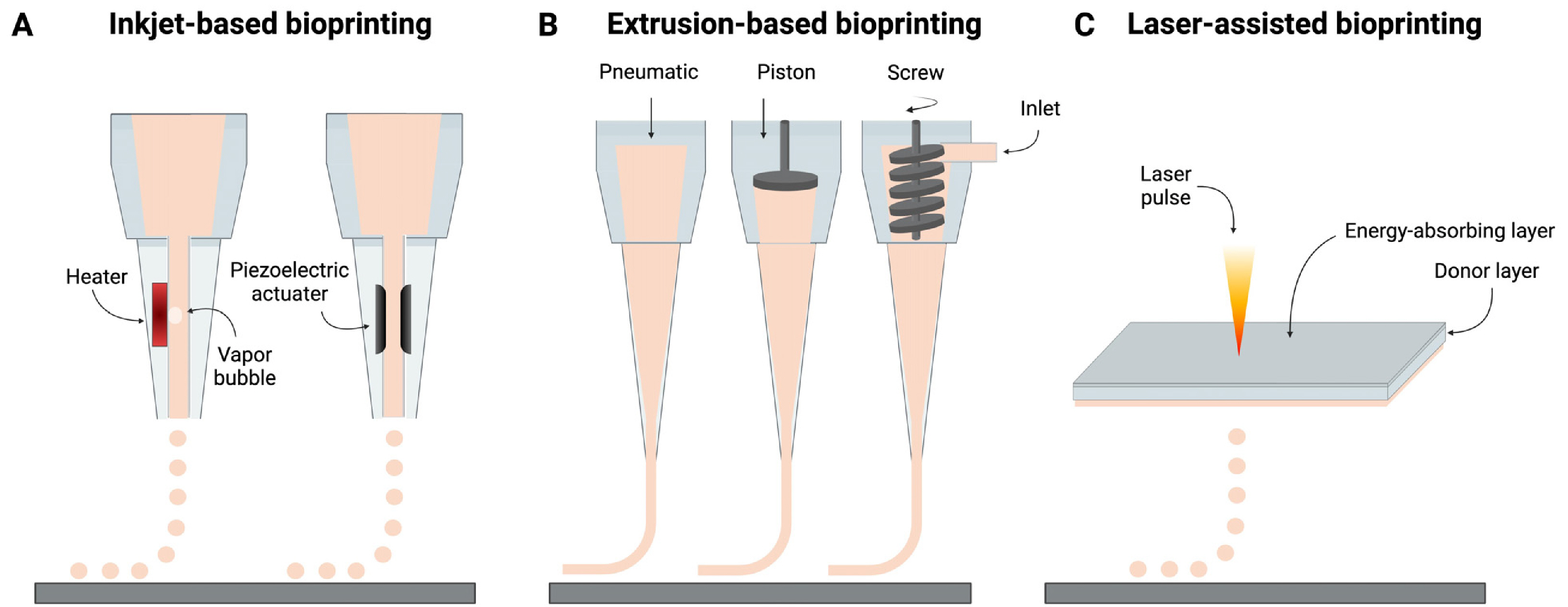
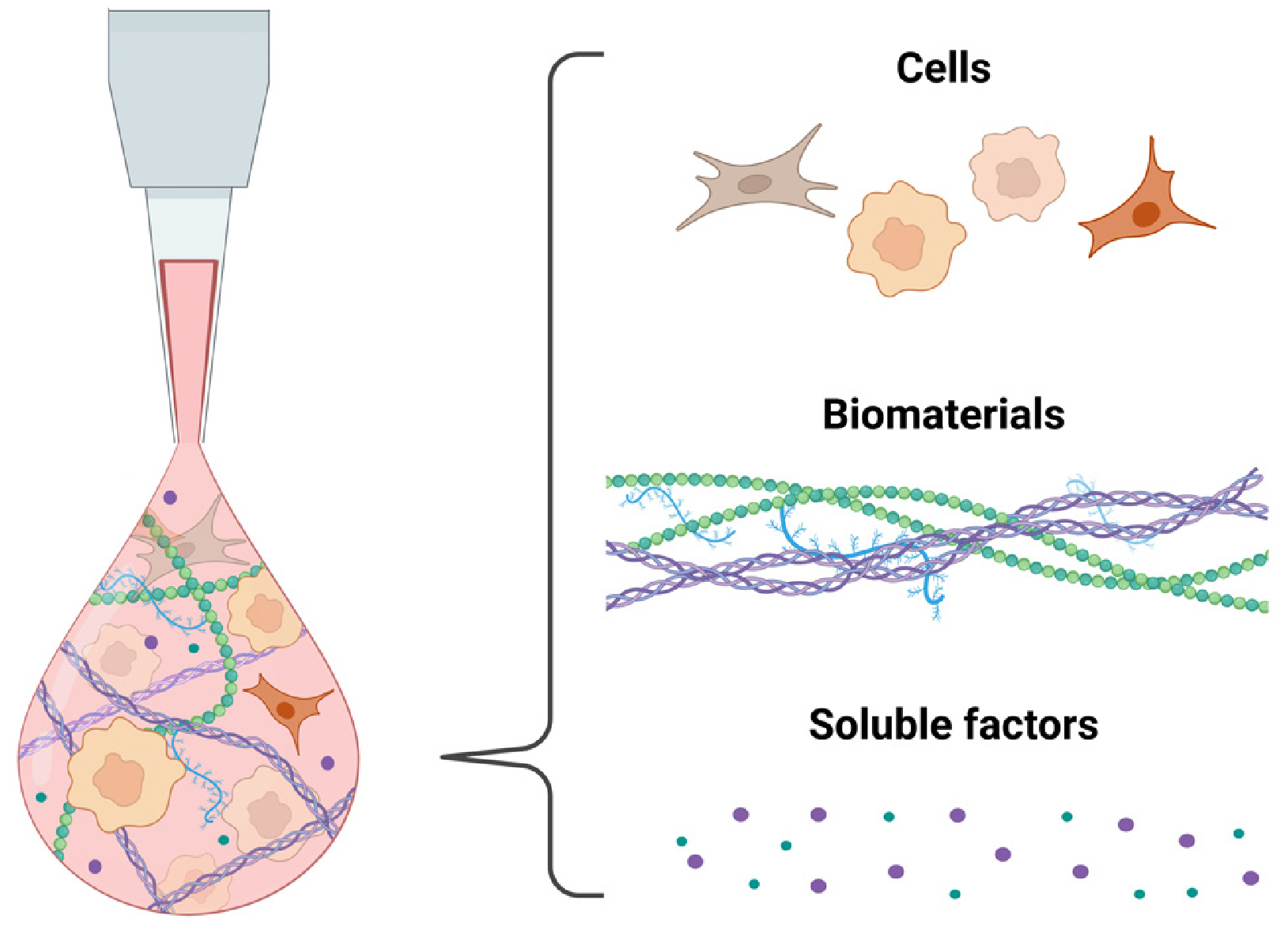
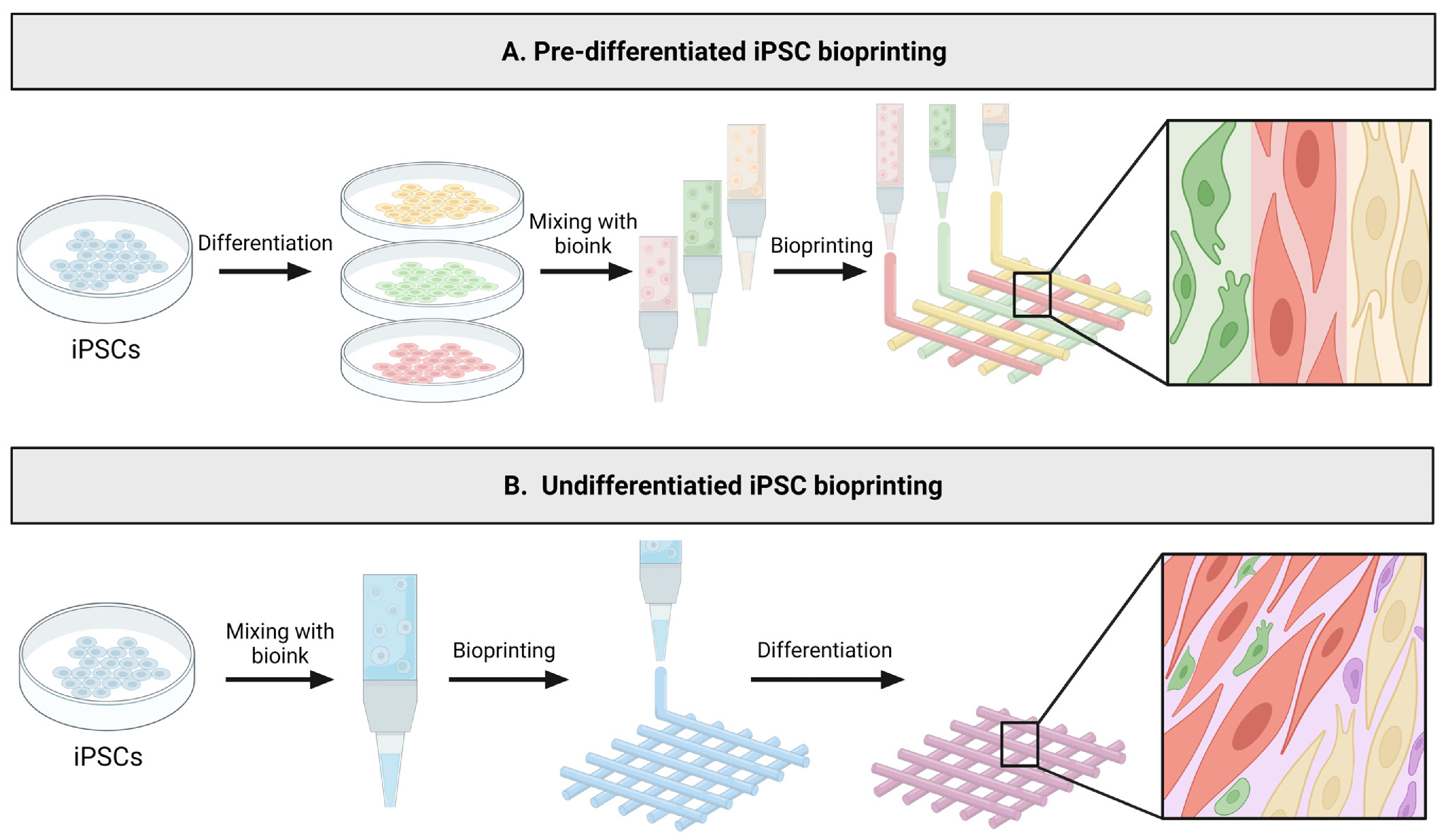
- Induced pluripotent stem cell (iPSC) technology has revolutionized various fields, including stem cell research, disease modeling, and regenerative medicine. The evolution of iPSC-based models has transitioned from conventional two-dimensional systems to more physiologically relevant three-dimensional (3D) models such as spheroids and organoids. Nonetheless, there still remain challenges including limitations in creating complex 3D tissue geometry and structures, the emergence of necrotic core in existing 3D models, and limited scalability and reproducibility. 3D bioprinting has emerged as a revolutionary technology that can facilitate the development of complex 3D tissues and organs with high scalability and reproducibility. This innovative approach has the potential to effectively bridge the gap between conventional iPSC models and complex 3D tissues in vivo. This review focuses on current trends and advancements in the bioprinting of iPSCs. Specifically, it covers the fundamental concepts and techniques of bioprinting and bioink design, reviews recent progress in iPSC bioprinting research with a specific focus on bioprinting undifferentiated iPSCs, and concludes by discussing existing limitations and future prospects.
Figure
Reference
-
References
1. Takahashi K, Tanabe K, Ohnuki M, et al. 2007; Induction of pluripotent stem cells from adult human fibroblasts by defined factors. Cell. 131:861–872. DOI: 10.1016/j.cell.2007.11.019. PMID: 18035408.
Article2. Takahashi K, Yamanaka S. 2006; Induction of pluripotent stem cells from mouse embryonic and adult fibroblast cultures by defined factors. Cell. 126:663–676. DOI: 10.1016/j.cell.2006.07.024. PMID: 16904174.
Article3. Jensen C, Teng Y. 2020; Is it time to start transitioning from 2D to 3D cell culture? Front Mol Biosci. 7:33. DOI: 10.3389/fmolb.2020.00033. PMID: 32211418. PMCID: PMC7067892. PMID: aec5f4cb51bf4807879336b5d3e21622.
Article4. Duval K, Grover H, Han LH, et al. 2017; Modeling physiological events in 2D vs. 3D cell culture. Physiology (Bethesda). 32:266–277. DOI: 10.1152/physiol.00036.2016. PMID: 28615311. PMCID: PMC5545611.
Article5. Kim J, Koo BK, Knoblich JA. 2020; Human organoids: model systems for human biology and medicine. Nat Rev Mol Cell Biol. 21:571–584. DOI: 10.1038/s41580-020-0259-3. PMID: 32636524. PMCID: PMC7339799.
Article6. Hofer M, Lutolf MP. 2021; Engineering organoids. Nat Rev Mater. 6:402–420. DOI: 10.1038/s41578-021-00279-y. PMID: 33623712. PMCID: PMC7893133.
Article7. Kačarević ŽP, Rider PM, Alkildani S, et al. 2018; An introduction to 3D bioprinting: possibilities, challenges and future aspects. Materials (Basel). 11:2199. DOI: 10.3390/ma11112199. PMID: 30404222. PMCID: PMC6266989. PMID: 9abefcf0bfc34ce1b67400bc2ae32199.
Article8. Thomson JA, Itskovitz-Eldor J, Shapiro SS, et al. 1998; Embryonic stem cell lines derived from human blastocysts. Science. 282:1145–1147. DOI: 10.1126/science.282.5391.1145. PMID: 9804556.
Article9. Hoffman LM, Carpenter MK. 2005; Characterization and culture of human embryonic stem cells. Nat Biotechnol. 23:699–708. DOI: 10.1038/nbt1102. PMID: 15940242.
Article10. Yu J, Hu K, Smuga-Otto K, et al. 2009; Human induced pluripotent stem cells free of vector and transgene sequences. Science. 324:797–801. DOI: 10.1126/science.1172482. PMID: 19325077. PMCID: PMC2758053.
Article11. Ludwig TE, Levenstein ME, Jones JM, et al. 2006; Derivation of human embryonic stem cells in defined conditions. Nat Biotechnol. 24:185–187. DOI: 10.1038/nbt1177. PMID: 16388305.
Article12. Richards M, Fong CY, Chan WK, Wong PC, Bongso A. 2002; Human feeders support prolonged undifferentiated growth of human inner cell masses and embryonic stem cells. Nat Biotechnol. 20:933–936. DOI: 10.1038/nbt726. PMID: 12161760.
Article13. Richards M, Tan S, Fong CY, Biswas A, Chan WK, Bongso A. 2003; Comparative evaluation of various human feeders for prolonged undifferentiated growth of human embryonic stem cells. Stem Cells. 21:546–556. DOI: 10.1634/stemcells.21-5-546. PMID: 12968109.
Article14. Amit M, Carpenter MK, Inokuma MS, et al. 2000; Clonally derived human embryonic stem cell lines maintain pluripotency and proliferative potential for prolonged periods of culture. Dev Biol. 227:271–278. DOI: 10.1006/dbio.2000.9912. PMID: 11071754.
Article15. Xu RH, Peck RM, Li DS, Feng X, Ludwig T, Thomson JA. 2005; Basic FGF and suppression of BMP signaling sustain undifferentiated proliferation of human ES cells. Nat Methods. 2:185–190. DOI: 10.1038/nmeth744. PMID: 15782187.
Article16. Watanabe K, Ueno M, Kamiya D, et al. 2007; A ROCK inhibitor permits survival of dissociated human embryonic stem cells. Nat Biotechnol. 25:681–686. DOI: 10.1038/nbt1310. PMID: 17529971.
Article17. Braam SR, Zeinstra L, Litjens S, et al. 2008; Recombinant vitronectin is a functionally defined substrate that supports human embryonic stem cell self-renewal via alphavbeta5 integrin. Stem Cells. 26:2257–2265. DOI: 10.1634/stemcells.2008-0291. PMID: 18599809.
Article18. Miyazaki T, Futaki S, Suemori H, et al. 2012; Laminin E8 fragments support efficient adhesion and expansion of dissociated human pluripotent stem cells. Nat Commun. 3:1236. DOI: 10.1038/ncomms2231. PMID: 23212365. PMCID: PMC3535336.
Article19. Rodin S, Domogatskaya A, Ström S, et al. 2010; Long-term self-renewal of human pluripotent stem cells on human recombinant laminin-511. Nat Biotechnol. 28:611–615. DOI: 10.1038/nbt.1620. PMID: 20512123.
Article20. Rodin S, Antonsson L, Hovatta O, Tryggvason K. 2014; Monolayer culturing and cloning of human pluripotent stem cells on laminin-521-based matrices under xeno-free and chemically defined conditions. Nat Protoc. 9:2354–2368. DOI: 10.1038/nprot.2014.159. PMID: 25211513.
Article21. Rodin S, Antonsson L, Niaudet C, et al. 2014; Clonal culturing of human embryonic stem cells on laminin-521/E-cadherin matrix in defined and xeno-free environment. Nat Commun. 5:3195. DOI: 10.1038/ncomms4195. PMID: 24463987.
Article22. Olmer R, Haase A, Merkert S, et al. 2010; Long term expansion of undifferentiated human iPS and ES cells in suspension culture using a defined medium. Stem Cell Res. 5:51–64. DOI: 10.1016/j.scr.2010.03.005. PMID: 20478754.
Article23. Steiner D, Khaner H, Cohen M, et al. 2010; Derivation, propagation and controlled differentiation of human embryonic stem cells in suspension. Nat Biotechnol. 28:361–364. DOI: 10.1038/nbt.1616. PMID: 20351691.
Article24. Lancaster MA, Renner M, Martin CA, et al. 2013; Cerebral organoids model human brain development and microcephaly. Nature. 501:373–379. DOI: 10.1038/nature12517. PMID: 23995685. PMCID: PMC3817409.
Article25. Qian X, Nguyen HN, Song MM, et al. 2016; Brain-region-specific organoids using mini-bioreactors for modeling ZIKV exposure. Cell. 165:1238–1254. DOI: 10.1016/j.cell.2016.04.032. PMID: 27118425. PMCID: PMC4900885.
Article26. Hofbauer P, Jahnel SM, Papai N, et al. 2021; Cardioids reveal self-organizing principles of human cardiogenesis. Cell. 184:3299–3317.e22. DOI: 10.1016/j.cell.2021.04.034. PMID: 34019794.
Article27. Lewis-Israeli YR, Wasserman AH, Gabalski MA, et al. 2021; Self-assembling human heart organoids for the modeling of cardiac development and congenital heart disease. Nat Commun. 12:5142. DOI: 10.1038/s41467-021-25329-5. PMID: 34446706. PMCID: PMC8390749. PMID: 253ca09085994e7ca7cf500eaaf085e0.
Article28. Murphy SV, Atala A. 2014; 3D bioprinting of tissues and organs. Nat Biotechnol. 32:773–785. DOI: 10.1038/nbt.2958. PMID: 25093879.
Article29. Arslan-Yildiz A, El Assal R, Chen P, Guven S, Inci F, Demirci U. 2016; Towards artificial tissue models: past, present, and future of 3D bioprinting. Biofabrication. 8:014103. DOI: 10.1088/1758-5090/8/1/014103. PMID: 26930133.
Article30. Hölzl K, Lin S, Tytgat L, Van Vlierberghe S, Gu L, Ovsianikov A. 2016; Bioink properties before, during and after 3D bioprinting. Biofabrication. 8:032002. DOI: 10.1088/1758-5090/8/3/032002. PMID: 27658612.
Article31. Khoeini R, Nosrati H, Akbarzadeh A, et al. 2021; Natural and synthetic bioinks for 3D bioprinting. Adv NanoBiomed Res. 1:2000097. DOI: 10.1002/anbr.202000097. PMID: 0a3e1a791efb48ecbfe1ba5c2f18e7dc.
Article32. Vijayavenkataraman S, Yan WC, Lu WF, Wang CH, Fuh JYH. 2018; 3D bioprinting of tissues and organs for regenerative medicine. Adv Drug Deliv Rev. 132:296–332. DOI: 10.1016/j.addr.2018.07.004. PMID: 29990578.
Article33. Guillemot F, Souquet A, Catros S, et al. 2010; High-throughput laser printing of cells and biomaterials for tissue engi-neering. Acta Biomater. 6:2494–2500. DOI: 10.1016/j.actbio.2009.09.029. PMID: 19819356.
Article34. Kim JD, Choi JS, Kim BS, Chan Choi Y, Cho YW. 2010; Piezoelectric inkjet printing of polymers: stem cell patterning on polymer substrates. Polymer. 51:2147–2154. DOI: 10.1016/j.polymer.2010.03.038.
Article35. Chang CC, Boland ED, Williams SK, Hoying JB. 2011; Direct-write bioprinting three-dimensional biohybrid systems for future regenerative therapies. J Biomed Mater Res B Appl Biomater. 98:160–170. DOI: 10.1002/jbm.b.31831. PMID: 21504055. PMCID: PMC3772543.
Article36. Koch L, Kuhn S, Sorg H, et al. 2010; Laser printing of skin cells and human stem cells. Tissue Eng Part C Methods. 16:847–854. DOI: 10.1089/ten.tec.2009.0397. PMID: 19883209.
Article37. Michael S, Sorg H, Peck CT, et al. 2013; Tissue engineered skin substitutes created by laser-assisted bioprinting form skin-like structures in the dorsal skin fold chamber in mice. PLoS One. 8:e57741. DOI: 10.1371/journal.pone.0057741. PMID: 23469227. PMCID: PMC3587634. PMID: c7098c3a3b03470abd3e7dbeea61849f.
Article38. Norotte C, Marga FS, Niklason LE, Forgacs G. 2009; Scaffold-free vascular tissue engineering using bioprinting. Biomaterials. 30:5910–5917. DOI: 10.1016/j.biomaterials.2009.06.034. PMID: 19664819. PMCID: PMC2748110.
Article39. Smith CM, Stone AL, Parkhill RL, et al. 2004; Three-dimensio-nal bioassembly tool for generating viable tissue-engineered constructs. Tissue Eng. 10:1566–1576. DOI: 10.1089/ten.2004.10.1566. PMID: 15588416.
Article40. Marga F, Jakab K, Khatiwala C, et al. 2012; Toward engineering functional organ modules by additive manufacturing. Bio-fabrication. 4:022001. DOI: 10.1088/1758-5082/4/2/022001. PMID: 22406433.
Article41. Li X, Liu B, Pei B, et al. 2020; Inkjet Bioprinting of Bio-materials. Chem Rev. 120:10793–10833. DOI: 10.1021/acs.chemrev.0c00008. PMID: 32902959.
Article42. Xu T, Jin J, Gregory C, Hickman JJ, Boland T. 2005; Inkjet prin-ting of viable mammalian cells. Biomaterials. 26:93–99. DOI: 10.1016/j.biomaterials.2004.04.011. PMID: 15193884.
Article43. Mirdamadi E, Tashman JW, Shiwarski DJ, Palchesko RN, Feinberg AW. 2020; FRESH 3D bioprinting a full-size model of the human heart. ACS Biomater Sci Eng. 6:6453–6459. DOI: 10.1021/acsbiomaterials.0c01133. PMID: 33449644.
Article44. Kim E, Choi S, Kang B, et al. 2020; Creation of bladder assembloids mimicking tissue regeneration and cancer. Nature. 588:664–669. DOI: 10.1038/s41586-020-3034-x. PMID: 33328632.
Article45. Guillotin B, Souquet A, Catros S, et al. 2010; Laser assisted bioprinting of engineered tissue with high cell density and microscale organization. Biomaterials. 31:7250–7256. DOI: 10.1016/j.biomaterials.2010.05.055. PMID: 20580082.
Article46. Zhu W, Ma X, Gou M, Mei D, Zhang K, Chen S. 2016; 3D printing of functional biomaterials for tissue engineering. Curr Opin Biotechnol. 40:103–112. DOI: 10.1016/j.copbio.2016.03.014. PMID: 27043763.
Article47. Yu C, Ma X, Zhu W, et al. 2019; Scanningless and continuous 3D bioprinting of human tissues with decellularized extracellular matrix. Biomaterials. 194:1–13. DOI: 10.1016/j.biomaterials.2018.12.009. PMID: 30562651. PMCID: PMC6339581.
Article48. Coffin BD, Hudson AR, Lee A, Feinberg AW. 2022; FRESH 3D bioprinting a ventricle-like cardiac construct using human stem cell-derived cardiomyocytes. Methods Mol Biol. 2485:71–85. DOI: 10.1007/978-1-0716-2261-2_5. PMID: 35618899.49. Maiullari F, Costantini M, Milan M, et al. 2018; A multi-cellular 3D bioprinting approach for vascularized heart tissue engineering based on HUVECs and iPSC-derived cardiomyo-cytes. Sci Rep. 8:13532. DOI: 10.1038/s41598-018-31848-x. PMID: 30201959. PMCID: PMC6131510.
Article50. Noor N, Shapira A, Edri R, Gal I, Wertheim L, Dvir T. 2019; 3D printing of personalized thick and perfusable cardiac patches and hearts. Adv Sci (Weinh). 6:1900344. DOI: 10.1002/advs.201900344. PMID: 31179230. PMCID: PMC6548966. PMID: 44cc3ac1883a478fb4d5120112eb3975.
Article51. Lawlor KT, Vanslambrouck JM, Higgins JW, et al. 2021; Cellular extrusion bioprinting improves kidney organoid reproducibility and conformation. Nat Mater. 20:260–271. DOI: 10.1038/s41563-020-00853-9. PMID: 33230326. PMCID: PMC7855371.
Article52. Choi K, Park CY, Choi JS, et al. 2023; The effect of the mechanical properties of the 3D printed gelatin/hyaluronic acid scaffolds on hMSCs differentiation towards chondrogenesis. Tissue Eng Regen Med. 20:593–605. DOI: 10.1007/s13770-023-00545-w. PMID: 37195569.
Article53. Narayanan LK, Huebner P, Fisher MB, Spang JT, Starly B, Shirwaiker RA. 2016; 3D-bioprinting of polylactic acid (PLA) nanofiber-alginate hydrogel bioink containing human adipose-derived stem cells. ACS Biomater Sci Eng. 2:1732–1742. DOI: 10.1021/acsbiomaterials.6b00196. PMID: 33440471.
Article54. Osidak EO, Karalkin PA, Osidak MS, et al. 2019; Viscoll collagen solution as a novel bioink for direct 3D bioprinting. J Mater Sci Mater Med. 30:31. DOI: 10.1007/s10856-019-6233-y. PMID: 30830351.
Article55. Duarte Campos DF, Rohde M, Ross M, et al. 2019; Corneal bioprinting utilizing collagen-based bioinks and primary human keratocytes. J Biomed Mater Res A. 107:1945–1953. DOI: 10.1002/jbm.a.36702. PMID: 31012205.
Article56. Park JA, Lee HR, Park SY, Jung S. 2020; Self-organization of fibroblast-laden 3D collagen microstructures from inkjet-printed cell patterns. Adv Biosyst. 4:e1900280. DOI: 10.1002/adbi.201900280. PMID: 32402122.
Article57. Säljö K, Orrhult LS, Apelgren P, Markstedt K, Kölby L, Gatenholm P. 2020; Successful engraftment, vascularization, and In vivo survival of 3D-bioprinted human lipoaspirate-derived adipose tissue. Bioprinting. 17:e00065. DOI: 10.1016/j.bprint.2019.e00065.58. Kim MH, Lee YW, Jung WK, Oh J, Nam SY. 2019; Enhanced rheological behaviors of alginate hydrogels with carrageenan for extrusion-based bioprinting. J Mech Behav Bio-med Mater. 98:187–194. DOI: 10.1016/j.jmbbm.2019.06.014. PMID: 31252328.
Article59. Faulkner-Jones A, Fyfe C, Cornelissen DJ, et al. 2015; Bioprin-ting of human pluripotent stem cells and their directed differentiation into hepatocyte-like cells for the generation of mini-livers in 3D. Biofabrication. 7:044102. DOI: 10.1088/1758-5090/7/4/044102. PMID: 26486521.
Article60. Poldervaart MT, Gremmels H, van Deventer K, et al. 2014; Pro-longed presence of VEGF promotes vascularization in 3D bioprinted scaffolds with defined architecture. J Control Release. 184:58–66. DOI: 10.1016/j.jconrel.2014.04.007. PMID: 24727077.
Article61. Snyder JE, Hamid Q, Wang C, et al. 2011; Bioprinting cell-laden matrigel for radioprotection study of liver by pro-drug conversion in a dual-tissue microfluidic chip. Biofabrication. 3:034112. DOI: 10.1088/1758-5082/3/3/034112. PMID: 21881168.
Article62. Berg J, Hiller T, Kissner MS, et al. 2018; Optimization of cell-laden bioinks for 3D bioprinting and efficient infection with influenza A virus. Sci Rep. 8:13877. DOI: 10.1038/s41598-018-31880-x. PMID: 30224659. PMCID: PMC6141611.
Article63. Xin S, Chimene D, Garza JE, Gaharwar AK, Alge DL. 2019; Clickable PEG hydrogel microspheres as building blocks for 3D bioprinting. Biomater Sci. 7:1179–1187. DOI: 10.1039/C8BM01286E. PMID: 30656307. PMCID: PMC9179007.
Article64. Skardal A, Zhang J, Prestwich GD. 2010; Bioprinting vessel-like constructs using hyaluronan hydrogels crosslinked with tetrahedral polyethylene glycol tetracrylates. Biomaterials. 31:6173–6181. DOI: 10.1016/j.biomaterials.2010.04.045. PMID: 20546891.
Article65. Dubbin K, Tabet A, Heilshorn SC. 2017; Quantitative criteria to benchmark new and existing bio-inks for cell compatibility. Biofabrication. 9:044102. DOI: 10.1088/1758-5090/aa869f. PMID: 28812982. PMCID: PMC5811195.
Article66. Borkar T, Goenka V, Jaiswal AK. 2021; Application of poly-ε-caprolactone in extrusion-based bioprinting. Bioprinting. 21:e00111. DOI: 10.1016/j.bprint.2020.e00111.
Article67. Merceron TK, Burt M, Seol YJ, et al. 2015; A 3D bioprinted complex structure for engineering the muscle-tendon unit. Biofabrication. 7:035003. DOI: 10.1088/1758-5090/7/3/035003. PMID: 26081669.
Article68. Duan B, Hockaday LA, Kang KH, Butcher JT. 2013; 3D bioprinting of heterogeneous aortic valve conduits with alginate/gelatin hydrogels. J Biomed Mater Res A. 101:1255–1264. DOI: 10.1002/jbm.a.34420. PMID: 23015540. PMCID: PMC3694360.
Article69. Pataky K, Braschler T, Negro A, Renaud P, Lutolf MP, Brugger J. 2012; Microdrop printing of hydrogel bioinks into 3D tissue-like geometries. Adv Mater. 24:391–396. DOI: 10.1002/adma.201102800. PMID: 22161949.
Article70. Huang J, Fu H, Wang Z, et al. 2016; BMSCs-laden gelatin/so-dium alginate/carboxymethyl chitosan hydrogel for 3D bio-printing. RSC Adv. 6:108423–108430. DOI: 10.1039/C6RA24231F.
Article71. Rajabi M, McConnell M, Cabral J, Ali MA. 2021; Chitosan hydrogels in 3D printing for biomedical applications. Carbohydr Polym. 260:117768. DOI: 10.1016/j.carbpol.2021.117768. PMID: 33712126.
Article72. Li Y, Jiang X, Li L, et al. 2018; 3D printing human induced pluripotent stem cells with novel hydroxypropyl chitin bioink: scalable expansion and uniform aggregation. Biofabrication. 10:044101. DOI: 10.1088/1758-5090/aacfc3. PMID: 29952313.
Article73. Engler AJ, Sen S, Sweeney HL, Discher DE. 2006; Matrix elasticity directs stem cell lineage specification. Cell. 126:677–689. DOI: 10.1016/j.cell.2006.06.044. PMID: 16923388.
Article74. Engler AJ, Carag-Krieger C, Johnson CP, et al. 2008; Embryonic cardiomyocytes beat best on a matrix with heart-like elasticity: scar-like rigidity inhibits beating. J Cell Sci. 121(Pt 22):3794–3802. DOI: 10.1242/jcs.029678. PMID: 18957515. PMCID: PMC2740334.
Article75. Lee S, Stanton AE, Tong X, Yang F. 2019; Hydrogels with enhanced protein conjugation efficiency reveal stiffness-in-duced YAP localization in stem cells depends on biochemical cues. Biomaterials. 202:26–34. DOI: 10.1016/j.biomaterials.2019.02.021. PMID: 30826537. PMCID: PMC6447317.
Article76. Chaudhuri O, Cooper-White J, Janmey PA, Mooney DJ, Shenoy VB. 2020; Effects of extracellular matrix viscoelasticity on cellular behaviour. Nature. 584:535–546. DOI: 10.1038/s41586-020-2612-2. PMID: 32848221. PMCID: PMC7676152.
Article77. Ong CS, Yesantharao P, Huang CY, et al. 2018; 3D bioprinting using stem cells. Pediatr Res. 83:223–231. DOI: 10.1038/pr.2017.252. PMID: 28985202.
Article78. Zhang YS, Arneri A, Bersini S, et al. 2016; Bioprinting 3D microfibrous scaffolds for engineering endothelialized myocardium and heart-on-a-chip. Biomaterials. 110:45–59. DOI: 10.1016/j.biomaterials.2016.09.003. PMID: 27710832. PMCID: PMC5198581.
Article79. Billiet T, Gevaert E, De Schryver T, Cornelissen M, Dubruel P. 2014; The 3D printing of gelatin methacrylamide cell-laden tissue-engineered constructs with high cell viability. Biomaterials. 35:49–62. DOI: 10.1016/j.biomaterials.2013.09.078. PMID: 24112804.
Article80. Rutz AL, Hyland KE, Jakus AE, Burghardt WR, Shah RN. 2015; A multimaterial bioink method for 3D printing tunable, cell-compatible hydrogels. Adv Mater. 27:1607–1614. DOI: 10.1002/adma.201405076. PMID: 25641220. PMCID: PMC4476973.
Article81. Kupfer ME, Lin WH, Ravikumar V, et al. 2020; In situ expan-sion, differentiation, and electromechanical coupling of human cardiac muscle in a 3D bioprinted, chambered orga-noid. Circ Res. 127:207–224. DOI: 10.1161/CIRCRESAHA.119.316155. PMID: 32228120. PMCID: PMC8210857.
Article82. Reid JA, Mollica PA, Johnson GD, Ogle RC, Bruno RD, Sachs PC. 2016; Accessible bioprinting: adaptation of a low-cost 3D-printer for precise cell placement and stem cell differen-tiation. Biofabrication. 8:025017. DOI: 10.1088/1758-5090/8/2/025017. PMID: 27271208.
Article83. Gu Q, Tomaskovic-Crook E, Wallace GG, Crook JM. 2017; 3D bioprinting human induced pluripotent stem cell constructs for in situ cell proliferation and successive multili-neage differentiation. Adv Healthc Mater. 6:1700175. DOI: 10.1002/adhm.201700175. PMID: 28544655.
Article84. Nguyen D, Hägg DA, Forsman A, et al. 2017; Cartilage tissue engineering by the 3D bioprinting of iPS cells in a nanocellulose/alginate bioink. Sci Rep. 7:658. DOI: 10.1038/s41598-017-00690-y. PMID: 28386058. PMCID: PMC5428803. PMID: 3c064b477afd4f1db31a5385f9ae7dfe.
Article85. Koch L, Deiwick A, Franke A, et al. 2018; Laser bioprinting of human induced pluripotent stem cells-the effect of printing and biomaterials on cell survival, pluripotency, and differen-tiation. Biofabrication. 10:035005. DOI: 10.1088/1758-5090/aab981. PMID: 29578448.
Article86. Axpe E, Oyen ML. 2016; Applications of alginate-based bioinks in 3D bioprinting. Int J Mol Sci. 17:1976. DOI: 10.3390/ijms17121976. PMID: 27898010. PMCID: PMC5187776. PMID: aa22e29657f04041873565c91cfa3e84.
Article87. Huang G, Li F, Zhao X, et al. 2017; Functional and biomimetic materials for engineering of the three-dimensional cell micro-environment. Chem Rev. 117:12764–12850. DOI: 10.1021/acs.chemrev.7b00094. PMID: 28991456. PMCID: PMC6494624.
Article88. Handorf AM, Zhou Y, Halanski MA, Li WJ. 2015; Tissue stiffness dictates development, homeostasis, and disease progre-ssion. Organogenesis. 11:1–15. DOI: 10.1080/15476278.2015.1019687. PMID: 25915734. PMCID: PMC4594591.
Article89. Guimarães CF, Gasperini L, Marques AP, Reis RL. 2020; The stiffness of living tissues and its implications for tissue engineering. Nat Rev Mater. 5:351–370. DOI: 10.1038/s41578-019-0169-1.
Article90. Pettikiriarachchi JTS, Parish CL, Shoichet MS, Forsythe JS, Nisbet DR. 2010; Biomaterials for brain tissue engineering. Aust J Chem. 63:1143–1154. DOI: 10.1071/CH10159.
Article91. Rauti R, Renous N, Maoz BM. 2020; Mimicking the brain extracellular matrix in vitro: a review of current methodologies and challenges. Israel J Chem. 60:1141–1151. DOI: 10.1002/ijch.201900052.
Article92. Novak U, Kaye AH. 2000; Extracellular matrix and the brain: components and function. J Clin Neurosci. 7:280–290. DOI: 10.1054/jocn.1999.0212. PMID: 10938601.
Article93. Bedossa P, Paradis V. 2003; Liver extracellular matrix in health and disease. J Pathol. 200:504–515. DOI: 10.1002/path.1397. PMID: 12845618.
Article94. Jain E, Damania A, Kumar A. 2014; Biomaterials for liver tissue engineering. Hepatol Int. 8:185–197. DOI: 10.1007/s12072-013-9503-7. PMID: 26202501.
Article95. Balestrini JL, Niklason LE. 2015; Extracellular matrix as a driver for lung regeneration. Ann Biomed Eng. 43:568–576. DOI: 10.1007/s10439-014-1167-5. PMID: 25344351. PMCID: PMC4380778.
Article96. Tebyanian H, Karami A, Nourani MR, et al. 2019; Lung tissue engineering: an update. J Cell Physiol. 234:19256–19270. DOI: 10.1002/jcp.28558. PMID: 30972749.
Article97. Lockhart M, Wirrig E, Phelps A, Wessels A. 2011; Extracellular matrix and heart development. Birth Defects Res A Clin Mol Teratol. 91:535–550. DOI: 10.1002/bdra.20810. PMID: 21618406. PMCID: PMC3144859.
Article98. Chen Q-Z, Harding SE, Ali NN, Lyon AR, Boccaccini AR. 2008; Biomaterials in cardiac tissue engineering: ten years of research survey. Mater Sci Eng R Rep. 59:1–37. DOI: 10.1016/j.mser.2007.08.001.
Article99. Hussain SH, Limthongkul B, Humphreys TR. 2013; The biomechanical properties of the skin. Dermatol Surg. 39:193–203. DOI: 10.1111/dsu.12095. PMID: 23350638.
Article100. Norouzi M, Boroujeni SM, Omidvarkordshouli N, Soleimani M. 2015; Advances in skin regeneration: application of electrospun scaffolds. Adv Healthc Mater. 4:1114–1133. DOI: 10.1002/adhm.201500001. PMID: 25721694.
Article101. Stevens MM. 2008; Biomaterials for bone tissue engineering. Mater Today. 11:18–25. DOI: 10.1016/S1369-7021(08)70086-5.
Article102. Ho DLL, Lee S, Du J, et al. 2022; Large-scale production of wholly cellular bioinks via the optimization of human induced pluripotent stem cell aggregate culture in automated bioreactors. Adv Healthc Mater. 11:e2201138. DOI: 10.1002/adhm.202270149. PMID: 36314397. PMCID: PMC10234214.
Article103. Skylar-Scott MA, Uzel SGM, Nam LL, et al. 2019; Biomanufacturing of organ-specific tissues with high cellular density and embedded vascular channels. Sci Adv. 5:eaaw2459. DOI: 10.1126/sciadv.aaw2459. PMID: 31523707. PMCID: PMC6731072.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Induced pluripotent stem cells and personalized medicine: current progress and future perspectives
- Advances in laser and stem cell treatment: current technologies, limitations, and future prospects
- Regenerative Medicine of the Bile Duct: Beyond the Myth
- Current and Future Perspectives of Stem Cell Therapy in Dermatology
- Stem cells: general information and perspectives