Ann Lab Med.
2023 Mar;43(2):196-199. 10.3343/alm.2023.43.2.196.
Emergence of NDM-1–producing Pseudomonas aeruginosa Sequence Type 773 Clone: Shift of Carbapenemase Molecular Epidemiology and Spread of 16S rRNA Methylase Genes in Korea
- Affiliations
-
- 1Department of Laboratory Medicine, Yonsei University College of Medicine, Seoul, Korea
- 2Department of Laboratory Medicine, National Health Insurance Service Ilsan Hospital, Goyang, Korea
- 3Research Institute of Bacterial Resistance, Seoul, Korea
- 4Department of Laboratory Medicine, Chonnam National University Medical School, Gwangju, Korea
- 5Department of Laboratory Medicine, Chungbuk National University College of Medicine, Cheongju, Korea
- 6Department of Laboratory Medicine and Paik Institute for Clinical Research, Inje University College of Medicine, Busan, Korea
- 7Department of Laboratory Medicine, Jeju National University, College of Medicine, Jeju, Korea
- 8Department of Laboratory Medicine, Hallym University Dongtan Sacred Heart Hospital, Hallym University College of Medicine, Hwaseong, Korea
- 9Department of Laboratory Medicine, Yonsei University Wonju College of Medicine, Wonju, Korea
- 10Department of Laboratory Medicine, Keimyung University School of Medicine, Daegu, Korea
- KMID: 2551697
- DOI: http://doi.org/10.3343/alm.2023.43.2.196
Abstract
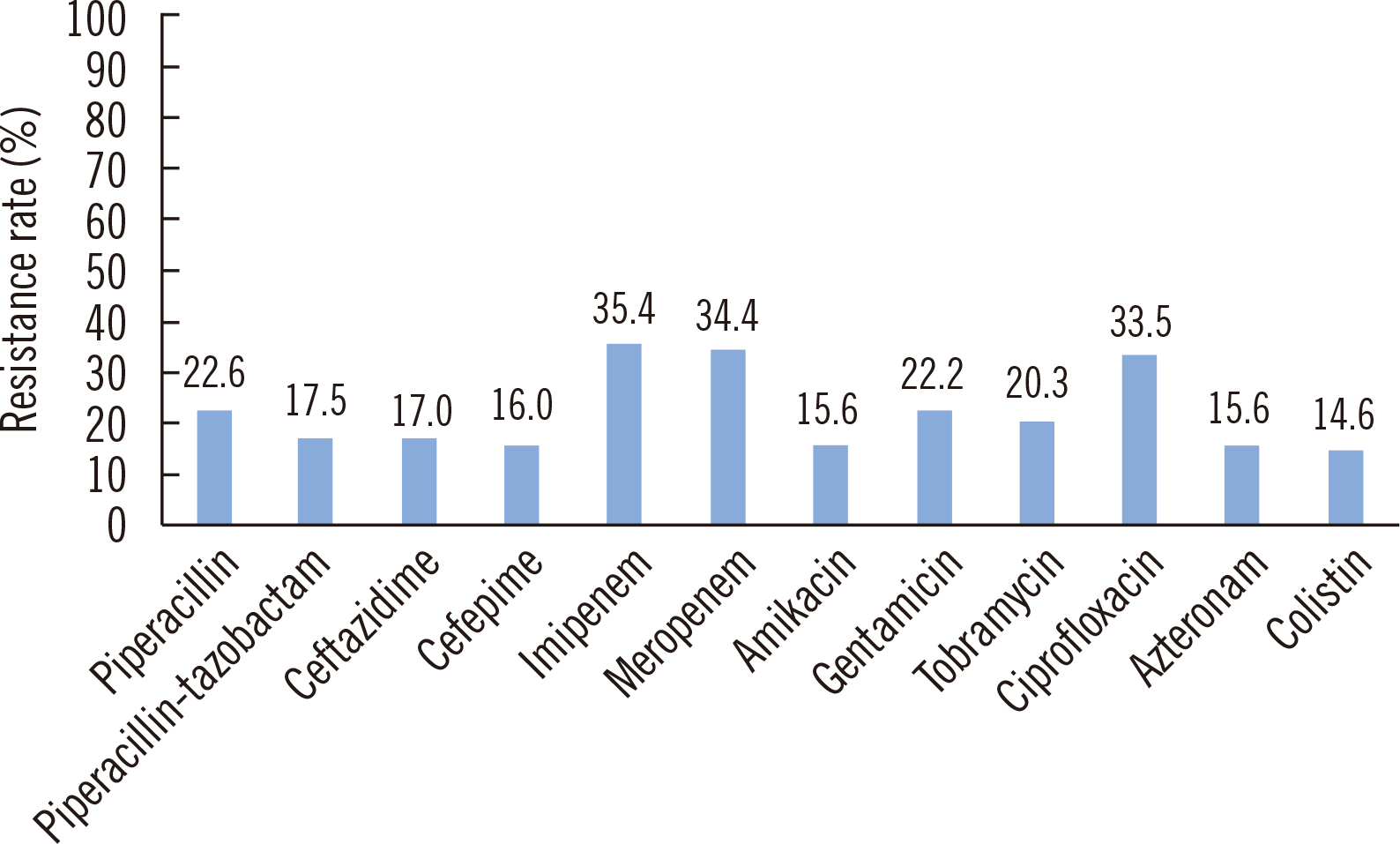
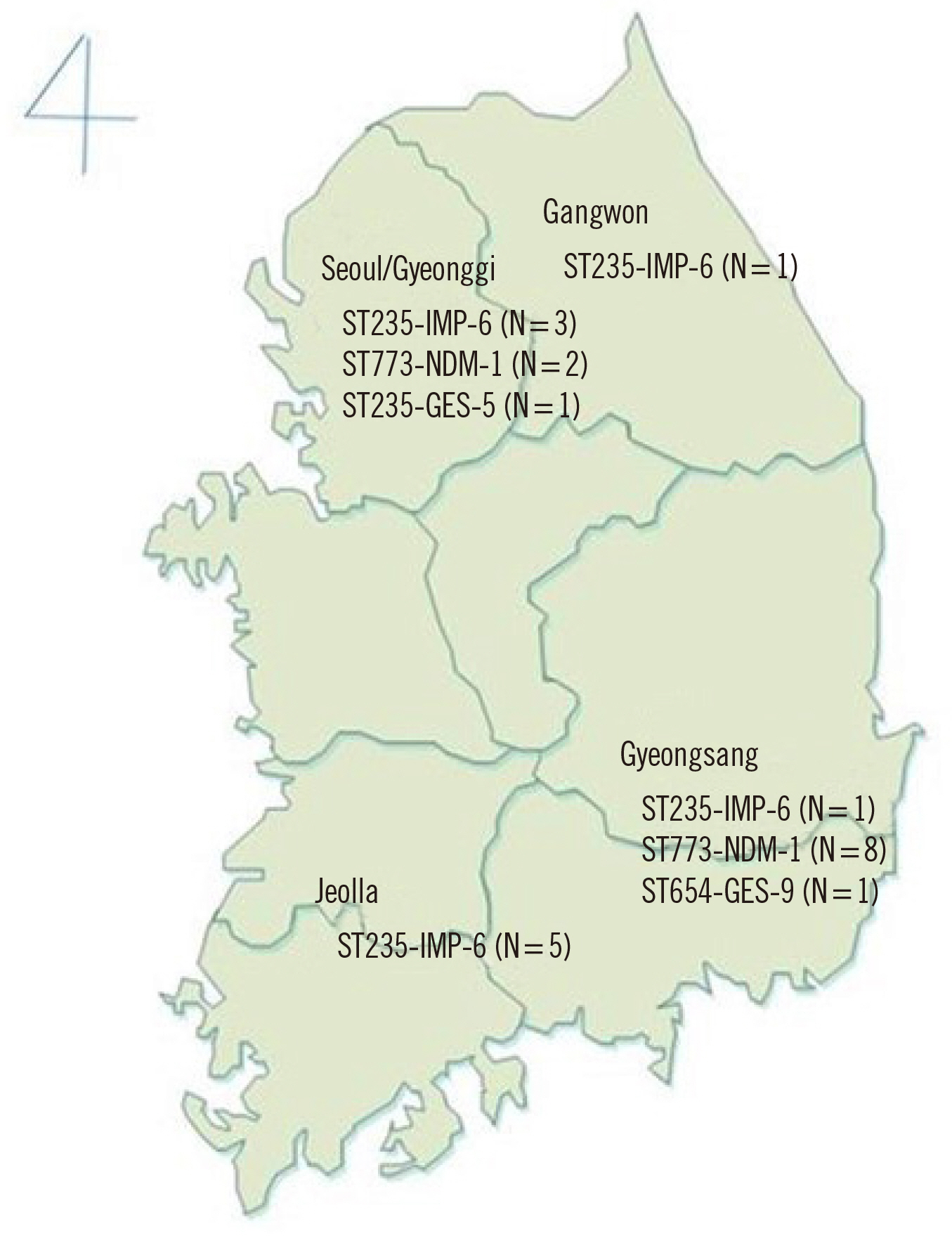
- Imipenemase (IMP)-6–producing Pseudomonas aeruginosa sequence type (ST) 235 is a dominant clone of carbapenemase-producing P. aeruginosa (CPPAE) in Korea. As part of the Antimicrobial Resistance Surveillance System in Korea, we found an increase in the carbapenem resistance rate of P. aeruginosa isolates from blood cultures and a shift in the molecular epidemiology of CPPAE. A total of 212 non-duplicated P. aeruginosa blood isolates were obtained from nine general hospitals and two nursing homes. Twenty-four isolates were identified as CPPAE. We observed the emergence of the NDM-1 P. aeruginosa ST 773 clone (N=10), mostly from Gyeongsang Province. The IMP-6 ST 235 clone (N=11) was detected in all provinces. CPPAE isolates showed very high resistance rates to amikacin, and all NDM-1 P. aeruginosa strains carried rmtB. This is the first nationwide surveillance of the recently emerged NDM-1–producing P. aeruginosa ST773 clone in Korea. Continuous surveillance is necessary to prevent the infection and transmission of carbapenem- and amikacin-resistant P. aeruginosa in Korea.
Keyword
Figure
Cited by 3 articles
-
Challenges of Carbapenem-resistant
Pseudomonas aeruginosa in Infection Control and Antibiotic Management
Young Jin Kim, Hee Jae Huh, Heungsup Sung
Ann Lab Med. 2024;44(1):1-2. doi: 10.3343/alm.2024.44.1.1.Importance of the Molecular Epidemiological Monitoring of Carbapenem-Resistant
Pseudomonas aeruginosa
Young Ah Kim
Ann Lab Med. 2024;44(5):381-382. doi: 10.3343/alm.2024.0184.Clonal Distribution and Its Association With the Carbapenem Resistance Mechanisms of Carbapenem-Non-Susceptible
Pseudomonas aeruginosa Isolates From Korean Hospitals
Nayeong Kim, Seo Yeon Ko, Seong Yong Park, Seong Yeob Kim, Da Eun Lee, Ki Tae Kwon, Yu Kyung Kim, Je Chul Lee
Ann Lab Med. 2024;44(5):410-417. doi: 10.3343/alm.2023.0369.
Reference
-
1. Yu SM, Jeon SS, Kang IS, An HG. 2006; Status of nosocomial urinary tract infections in the ICU: molecular epidemiology of imipenem resistant P. aeruginosa. Taehan Kanho Hakhoe Chi. 36:1204–14. DOI: 10.4040/jkan.2006.36.7.1204. PMID: 17211123.
Article2. Lee JY, Ko KS. 2012; OprD mutations and inactivation, expression of efflux pumps and AmpC, and metallo-β-lactamases in carbapenem-resistant Pseudomonas aeruginosa isolates from South Korea. Int J Antimicrob Agents. 40:168–72. DOI: 10.1016/j.ijantimicag.2012.04.004. PMID: 22633564.3. Yoon EJ, Jeong SH. 2021; Mobile carbapenemase genes in Pseudomonas aeruginosa. Front Microbiol. 12:614058. DOI: 10.3389/fmicb.2021.614058. PMID: 33679638. PMCID: PMC7930500.4. Yoo JS, Yang JW, Kim HM, Byeon J, Kim HS, Yoo JI, et al. 2012; Dissemination of genetically related IMP-6-producing multidrug-resistant Pseudomonas aeruginosa ST235 in South Korea. Int J Antimicrob Agents. 39:300–4. DOI: 10.1016/j.ijantimicag.2011.11.018. PMID: 22325122.5. Seok Y, Bae IK, Jeong SH, Kim SH, Lee H, Lee K. 2011; Dissemination of IMP-6 metallo-β-lactamase-producing Pseudomonas aeruginosa sequence type 235 in Korea. J Antimicrob Chemother. 66:2791–6. DOI: 10.1093/jac/dkr381. PMID: 21933788.6. Cho HH, Kwon KC, Sung JY, Koo SH. 2013; Prevalence and genetic analysis of multidrug-resistant Pseudomonas aeruginosa ST235 isolated from a hospital in Korea, 2008-2012. Ann Clin Lab Sci. 43:414–9.7. Kim MJ, Bae IK, Jeong SH, Kim SH, Song JH, Choi JY, et al. 2013; Dissemination of metallo-β-lactamase-producing Pseudomonas aeruginosa of sequence type 235 in Asian countries. J Antimicrob Chemother. 68:2820–4. DOI: 10.1093/jac/dkt269. PMID: 23843299.8. Lee H, Yoon EJ, Kim D, Jeong SH, Shin JH, Shin JH, et al. 2018; Establishment of the South Korean national antimicrobial resistance surveillance system, Kor-GLASS, in 2016. Euro Surveill. 23:1700734. DOI: 10.2807/1560-7917.ES.2018.23.42.1700734. PMID: 30352643. PMCID: PMC6199867.
Article9. CLSI. 2020. Performance standards for antimicrobial susceptibility testing. 28th ed. CLSI M100. Clinical and Laboratory Standards Institute;Wayne, PA:10. Center for Genomic Epidemiology. www.genomicepidemiology.org. Updated on Feb 2022.11. Hong JS, Choi N, Kim SJ, Choi KH, Roh KH, Lee S. 2020; Molecular characteristics of GES-type carbapenemase-producing Pseudomonas aeruginosa clinical isolates from long-term care facilities and general hospitals in South Korea. Microb Drug Resist. 26:605–10. DOI: 10.1089/mdr.2019.0302. PMID: 31800356.12. Hong JS, Song W, Park MJ, Jeong S, Lee N, Jeong SH. 2021; Molecular characterization of the first emerged NDM-1-producing Pseudomonas aeruginosa isolates in South Korea. Microb Drug Resist. 27:1063–70. DOI: 10.1089/mdr.2020.0374. PMID: 33332204.13. Farhan SM, Raafat M, Abourehab MAS, Abd El-Baky RM, Abdalla S, El-Gendy AO, et al. 2021; Effect of imipenem and amikacin combination against multi-drug resistant Pseudomonas aeruginosa. Antibiotics. 10:1429. DOI: 10.3390/antibiotics10111429. PMID: 34827367. PMCID: PMC8615098.
Article14. Junaid K. Molecular diversity of NDM-1, NDM-5, NDM-6, and NDM-7 variants of New Delhi metallo-β-lactamases and their impact on drug resistance. Clin Lab. 2021; 67:DOI: 10.7754/Clin.Lab.2021.201214. PMID: 34383423.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Erratum: Emergence of NDM-1–producing Pseudomonas aeruginosa Sequence Type 773 Clone: Shift of Carbapenemase Molecular Epidemiology and Spread of 16S rRNA Methylase Genes in Korea
- Antimicrobial Susceptibility and Clonal Distribution of the Blood Isolates of Pseudomonas aeruginosa from Two Korean Hospitals
- Molecular and Phenotypic Characteristics of 16S rRNA Methylase-producing Gram-negative Bacilli
- Importance of the Molecular Epidemiological Monitoring of Carbapenem-Resistant Pseudomonas aeruginosa
- Clonal Distribution and Its Association With the Carbapenem Resistance Mechanisms of Carbapenem-Non-Susceptible Pseudomonas aeruginosa Isolates From Korean Hospitals