Diabetes Metab J.
2024 Jan;48(1):122-133. 10.4093/dmj.2022.0431.
Psychotic Disorders and the Risk of Type 2 Diabetes Mellitus, Atherosclerotic Cardiovascular Diseases, and All-Cause Mortality: A Population-Based Matched Cohort Study
- Affiliations
-
- 1Division of Endocrinology and Metabolism, Department of Internal Medicine, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea
- 2Department of Psychiatry, Hanyang University Hospital, Seoul, Korea
- 3Data Science Team, Hanmi Pharm. Co., Ltd., Seoul, Korea
- 4Department of Psychiatry, Depression Center, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea
- KMID: 2551268
- DOI: http://doi.org/10.4093/dmj.2022.0431
Abstract
- Background
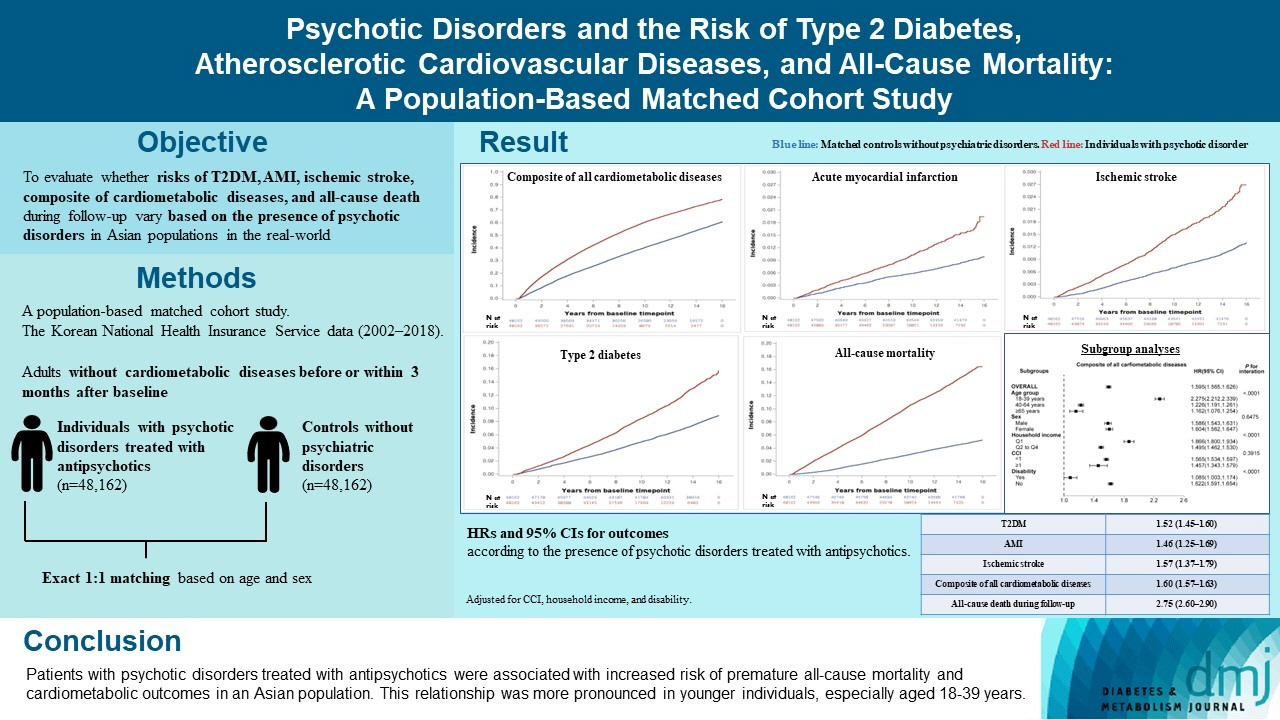
The effects of psychotic disorders on cardiometabolic diseases and premature death need to be determined in Asian populations.
Methods
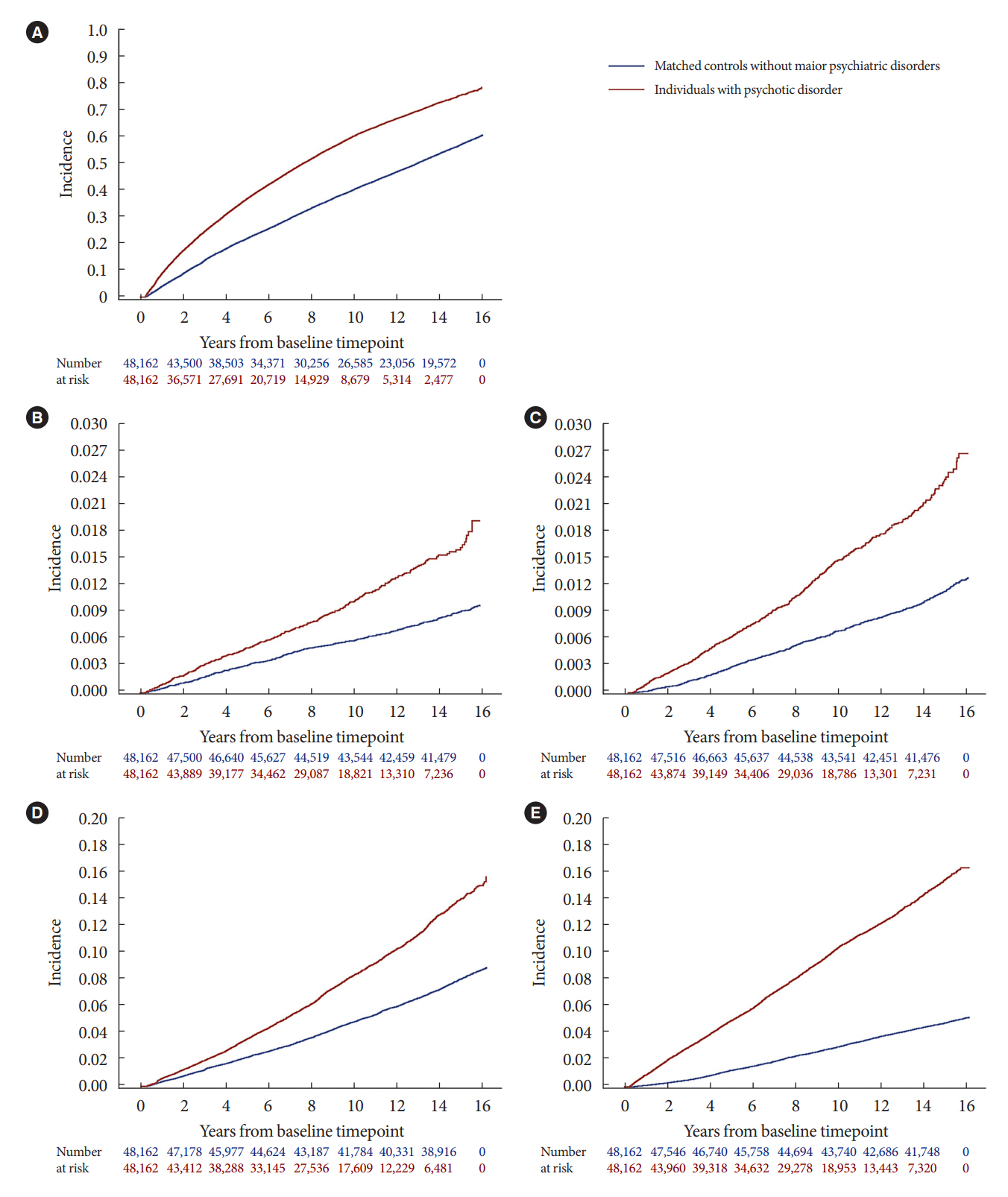
In this population-based matched cohort study, the Korean National Health Insurance Service database (2002 to 2018) was used. The risk of type 2 diabetes mellitus (T2DM), acute myocardial infarction (AMI), ischemic stroke, composite of all cardiometabolic diseases, and all-cause death during follow-up was compared between individuals with psychotic disorders treated with antipsychotics (n=48,162) and 1:1 matched controls without psychiatric disorders among adults without cardiometabolic diseases before or within 3 months after baseline.
Results
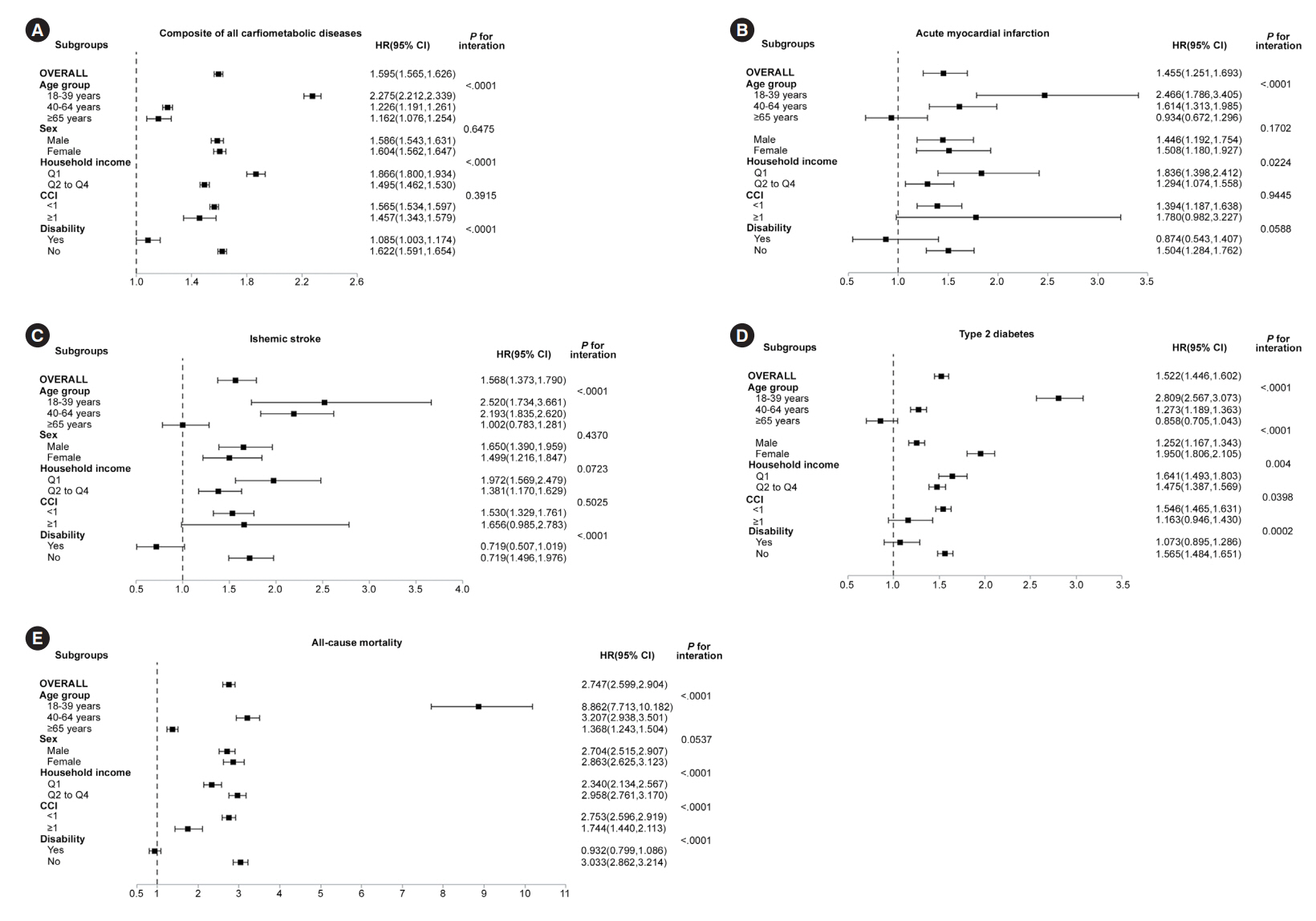
In this cohort, 53,683 composite cases of all cardiometabolic diseases (during median 7.38 years), 899 AMI, and 1,216 ischemic stroke cases (during median 14.14 years), 7,686 T2DM cases (during median 13.26 years), and 7,092 deaths (during median 14.23 years) occurred. The risk of all outcomes was higher in subjects with psychotic disorders than matched controls (adjusted hazard ratios [95% confidence intervals]: 1.522 [1.446 to 1.602] for T2DM; 1.455 [1.251 to 1.693] for AMI; 1.568 [1.373 to 1.790] for ischemic stroke; 1.595 [1.565 to 1.626] for composite of all cardiometabolic diseases; and 2.747 [2.599 to 2.904] for all-cause mortality) during follow-up. Similar patterns of associations were maintained in subgroup analyses but more prominent in younger individuals (P for interaction <0.0001) when categorized as those aged 18–39, 40–64, or ≥65 years.
Conclusion
Patients with psychotic disorders treated with antipsychotics were associated with increased risk of premature allcause mortality and cardiometabolic outcomes in an Asian population. This relationship was more pronounced in younger individuals, especially aged 18 to 39 years.
Keyword
Figure
Reference
-
1. Newcomer JW, Hennekens CH. Severe mental illness and risk of cardiovascular disease. JAMA. 2007; 298:1794–6.2. Goldstein BI, Carnethon MR, Matthews KA, McIntyre RS, Miller GE, Raghuveer G, et al. Major depressive disorder and bipolar disorder predispose youth to accelerated atherosclerosis and early cardiovascular disease: a scientific statement from the American Heart Association. Circulation. 2015; 132:965–86.3. Nielsen RE, Banner J, Jensen SE. Cardiovascular disease in patients with severe mental illness. Nat Rev Cardiol. 2021; 18:136–45.4. Kugathasan P, Stubbs B, Aagaard J, Jensen SE, Munk Laursen T, Nielsen RE. Increased mortality from somatic multimorbidity in patients with schizophrenia: a Danish nationwide cohort study. Acta Psychiatr Scand. 2019; 140:340–8.5. Ringen PA, Engh JA, Birkenaes AB, Dieset I, Andreassen OA. Increased mortality in schizophrenia due to cardiovascular disease: a non-systematic review of epidemiology, possible causes, and interventions. Front Psychiatry. 2014; 5:137.6. Ward M, Druss B. The epidemiology of diabetes in psychotic disorders. Lancet Psychiatry. 2015; 2:431–51.7. Curkendall SM, Mo J, Glasser DB, Rose Stang M, Jones JK. Cardiovascular disease in patients with schizophrenia in Saskatchewan, Canada. J Clin Psychiatry. 2004; 65:715–20.8. Seong SC, Kim YY, Khang YH, Park JH, Kang HJ, Lee H, et al. Data resource profile: the National Health Information Database of the National Health Insurance Service in South Korea. Int J Epidemiol. 2017; 46:799–800.9. Lee YH, Han K, Ko SH, Ko KS, Lee KU; Taskforce Team of Diabetes Fact Sheet of the Korean Diabetes Association. Data analytic process of a nationwide population-based study using National Health Information Database established by National Health Insurance Service. Diabetes Metab J. 2016; 40:79–82.10. De Hert M, Correll CU, Bobes J, Cetkovich-Bakmas M, Cohen D, Asai I, et al. Physical illness in patients with severe mental disorders. I. Prevalence, impact of medications and disparities in health care. World Psychiatry. 2011; 10:52–77.11. Noh J, Han KD, Ko SH, Ko KS, Park CY. Trends in the pervasiveness of type 2 diabetes, impaired fasting glucose and comorbidities during an 8-year-follow-up of nationwide Korean population. Sci Rep. 2017; 7:46656.12. Lee YB, Kim DH, Kim SM, Kim NH, Choi KM, Baik SH, et al. Risk of type 2 diabetes according to the cumulative exposure to metabolic syndrome or obesity: a nationwide populationbased study. J Diabetes Investig. 2020; 11:1583–93.13. Lee YB, Han K, Kim B, Lee SE, Jun JE, Ahn J, et al. Risk of early mortality and cardiovascular disease in type 1 diabetes: a comparison with type 2 diabetes, a nationwide study. Cardiovasc Diabetol. 2019; 18:157.14. Kim MK, Han K, Kim HS, Park YM, Kwon HS, Yoon KH, et al. Cholesterol variability and the risk of mortality, myocardial infarction, and stroke: a nationwide population-based study. Eur Heart J. 2017; 38:3560–6.15. Kim MK, Han K, Koh ES, Kim ES, Lee MK, Nam GE, et al. Blood pressure and development of cardiovascular disease in Koreans with type 2 diabetes mellitus. Hypertension. 2019; 73:319–26.16. Charlson ME, Pompei P, Ales KL, MacKenzie CR. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis. 1987; 40:373–83.17. Sundararajan V, Henderson T, Perry C, Muggivan A, Quan H, Ghali WA. New ICD-10 version of the Charlson comorbidity index predicted in-hospital mortality. J Clin Epidemiol. 2004; 57:1288–94.18. Jung I, Kwon H, Park SE, Han KD, Park YG, Rhee EJ, et al. The prevalence and risk of type 2 diabetes in adults with disabilities in Korea. Endocrinol Metab (Seoul). 2020; 35:552–61.19. Fine JP, Gray RJ. A proportional hazards model for the subdistribution of a competing risk. J Am Stat Assoc. 1999; 94:496–509.20. Oh J, Nam H, Park S, Chae JH, Kim TS. Decreased cardiovascular death in schizophrenia patients treated with antipsychotics: a Korean national cohort study. Schizophr Res. 2021; 228:417–24.21. De Hert M, Cohen D, Bobes J, Cetkovich-Bakmas M, Leucht S, Ndetei DM, et al. Physical illness in patients with severe mental disorders. II. Barriers to care, monitoring and treatment guidelines, plus recommendations at the system and individual level. World Psychiatry. 2011; 10:138–51.22. So HC, Chau KL, Ao FK, Mo CH, Sham PC. Exploring shared genetic bases and causal relationships of schizophrenia and bipolar disorder with 28 cardiovascular and metabolic traits. Psychol Med. 2019; 49:1286–98.23. Malan-Muller S, Kilian S, van den Heuvel LL, Bardien S, Asmal L, Warnich L, et al. A systematic review of genetic variants associated with metabolic syndrome in patients with schizophrenia. Schizophr Res. 2016; 170:1–17.24. Laursen TM, Nordentoft M, Mortensen PB. Excess early mortality in schizophrenia. Annu Rev Clin Psychol. 2014; 10:425–48.25. Walker ER, McGee RE, Druss BG. Mortality in mental disorders and global disease burden implications: a systematic review and meta-analysis. JAMA Psychiatry. 2015; 72:334–41.26. Nielsen RE, Uggerby AS, Jensen SO, McGrath JJ. Increasing mortality gap for patients diagnosed with schizophrenia over the last three decades: a Danish nationwide study from 1980 to 2010. Schizophr Res. 2013; 146:22–7.27. Piotrowski P, Gondek TM, Krolicka-Deregowska A, Misiak B, Adamowski T, Kiejna A. Causes of mortality in schizophrenia: an updated review of European studies. Psychiatr Danub. 2017; 29:108–20.28. Kirkpatrick B, Kennedy BK. Accelerated aging in schizophrenia and related disorders: future research. Schizophr Res. 2018; 196:4–8.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Type 2 diabetes mellitus and metabolic syndrome
- Hypoglycemia and Dementia Risk in Older Patients with Type 2 Diabetes Mellitus: A Propensity-Score Matched Analysis of a Population-Based Cohort Study (Diabetes Metab J 2020;44:125-33)
- Hypoglycemia and Dementia Risk in Older Patients with Type 2 Diabetes Mellitus: A Propensity-Score Matched Analysis of a Population-Based Cohort Study (Diabetes Metab J 2020;44:125-33)
- Management of Type 2 Diabetes Mellitus in the Elderly
- Paradigm Changes in Diabetes Management Guidelines: American Diabetes Association 2018