Acute Crit Care.
2023 Nov;38(4):460-468. 10.4266/acc.2022.01501.
Effect of fourth hourly oropharyngeal suctioning on ventilator-associated events in patients requiring mechanical ventilation in intensive care units of a tertiary care center in South India: a randomized controlled trial
- Affiliations
-
- 1College of Nursing, Jawaharlal Institute of Postgraduate Medical Education and Research, Pondicherry, India
- 2Department of Anaesthesiology and Critical Care, Jawaharlal Institute of Postgraduate Medical Education and Research, Pondicherry, India
- 3Department of Biostatistics, Jawaharlal Institute of Postgraduate Medical Education and Research, Pondicherry, India
- KMID: 2550902
- DOI: http://doi.org/10.4266/acc.2022.01501
Abstract
- Background
Mechanical ventilation (MV) is a necessary life-saving measure for critically ill patients. Ventilator-associated events (VAEs) are potentially avoidable complications associated with MV that can double the rate of death. Oral care and oropharyngeal suctioning, although neglected procedures, play a vital role in the prevention of VAE.
Methods
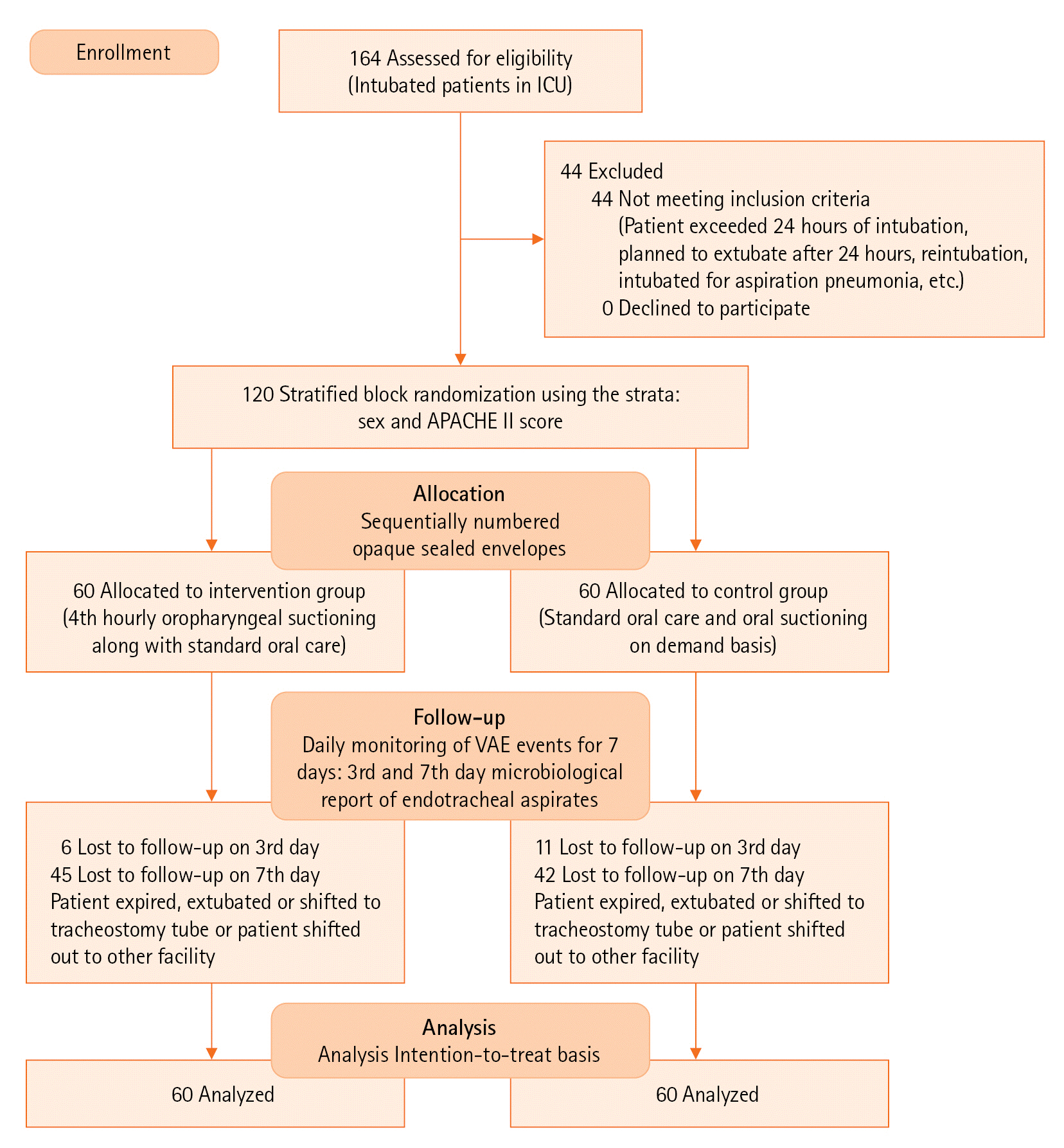
A randomized controlled trial was conducted in the intensive care units to compare the effect of fourth hourly oropharyngeal suctioning with the standard oral care protocol on VAE among patients on MV. One hundred twenty mechanically ventilated patients who were freshly intubated and expected to be on ventilator support for the next 72 hours were randomly allocated to the control or intervention groups. The intervention was fourth hourly oropharyngeal suctioning along with the standard oral care procedure. The control group received standard oral care (i.e., thrice a day) and on-demand oral suctioning. On the 3rd and 7th days following the intervention, endotracheal aspirates were sent to rule out ventilator-associated pneumonia.
Results
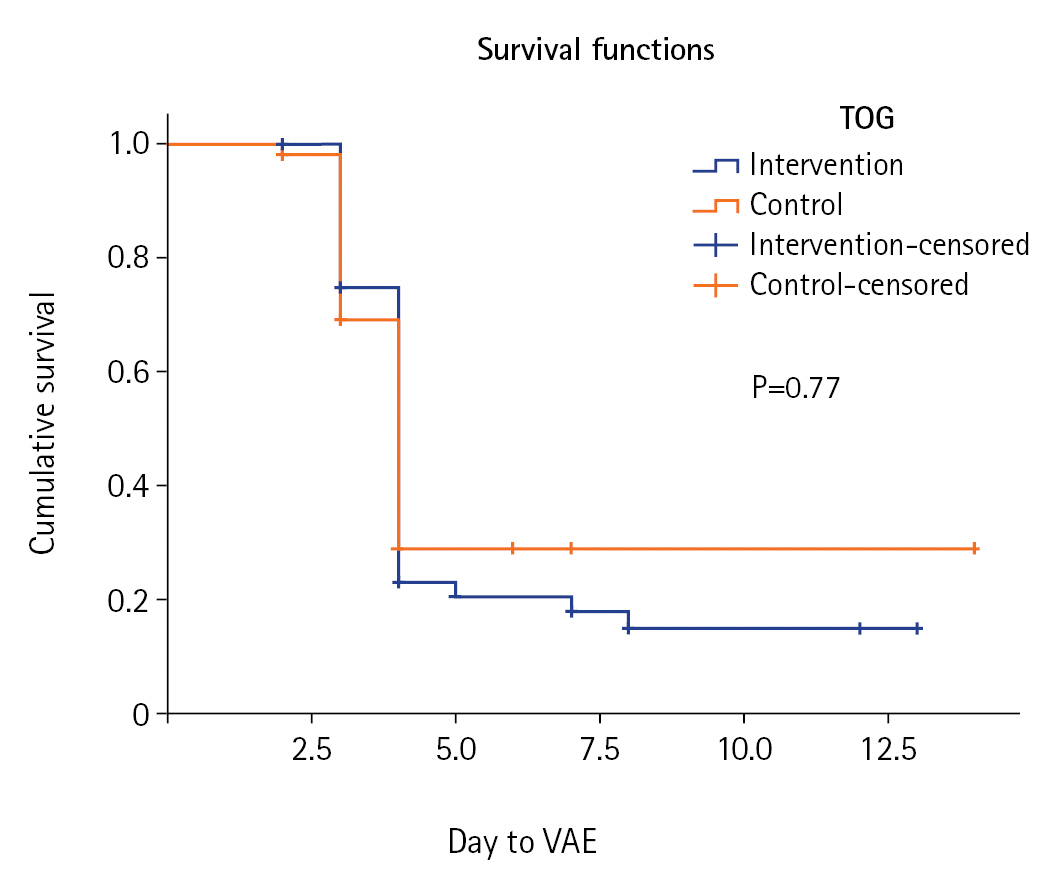
Both groups were homogenous at baseline with respect to their clinical characteristics. The intervention group had fewer VAEs (56.7%) than the control group (78.3%) which was significant at P<0.01. A significant reduction in the status of “positive culture” on ET aspirate also been observed following the 3rd day of the intervention (P<0.001).
Conclusions
One of the most basic preventive strategies is providing oral care. Oropharyngeal suctioning is also an important component of oral care that prevents microaspiration. Hence, fourth-hourly oropharyngeal suctioning with standard oral care significantly reduces the incidence of VAE.
Keyword
Figure
Reference
-
1. Sole ML, Penoyer DA, Bennett M, Bertrand J, Talbert S. Oropharyngeal secretion volume in intubated patients: the importance of oral suctioning. Am J Crit Care. 2011; 20:e141–5.
Article2. Burja S, Belec T, Bizjak N, Mori J, Markota A, Sinkovič A. Efficacy of a bundle approach in preventing the incidence of ventilator associated pneumonia (VAP). Bosn J Basic Med Sci. 2018; 18:105–9.
Article3. United States Department of Health and Human Services, Centers for Disease Control and Prevention. Ventilator-associated event (VAE). Centers for Disease Control and Prevention;2019. [cited 2023 Aug 1]. Available from: https://www.cdc.gov/nhsn/pdfs/pscmanual/10-vae_final.pdf.4. Klompas M, Kleinman K, Murphy MV. Descriptive epidemiology and attributable morbidity of ventilator-associated events. Infect Control Hosp Epidemiol. 2014; 35:502–10.
Article5. Peña-López Y, Ramírez-Estrada S, Rello J. Ventilator-associated events: definitions and uses. Encyclopedia of Respiratory Medicine. 2022; 523–9.
Article6. Garcia R, Jendresky L, Colbert L, Bailey A, Zaman M, Majumder M. Reducing ventilator-associated pneumonia through advanced oral-dental care: a 48-month study. Am J Crit Care. 2009; 18:523–32.
Article7. Bergmans DC, Bonten MJ, Gaillard CA, Paling JC, van der Geest S, van Tiel FH, et al. Prevention of ventilator-associated pneumonia by oral decontamination: a prospective, randomized, double-blind, placebo-controlled study. Am J Respir Crit Care Med. 2001; 164:382–8.
Article8. Boyer AF, Schoenberg N, Babcock H, McMullen KM, Micek ST, Kollef MH. A prospective evaluation of ventilator-associated conditions and infection-related ventilator-associated conditions. Chest. 2015; 147:68–81.
Article9. Muscedere J, Sinuff T, Heyland DK, Dodek PM, Keenan SP, Wood G, et al. The clinical impact and preventability of ventilator-associated conditions in critically ill patients who are mechanically ventilated. Chest. 2013; 144:1453–60.
Article10. Bo H, He L, Qu J. Influence of the subglottic secretion drainage on the morbidity of ventilator associated pneumonia in mechanically ventilated patients. Zhonghua Jie He He Hu Xi Za Zhi. 2000; 23:472–4.11. Paju S, Scannapieco FA. Oral biofilms, periodontitis, and pulmonary infections. Oral Dis. 2007; 13:508–12.
Article12. Fields LB. Oral care intervention to reduce incidence of ventilator-associated pneumonia in the neurologic intensive care unit. J Neurosci Nurs. 2008; 40:291–8.
Article13. Sole ML, Talbert S, Yan X, Penoyer D, Mehta D, Bennett M, et al. Impact of deep oropharyngeal suctioning on microaspiration, ventilator events, and clinical outcomes: a randomized clinical trial. J Adv Nurs. 2019; 75:3045–57.
Article14. Atashi V, Yousefi H, Mahjobipoor H, Bekhradi R, Yazdannik A. Effect of oral care program on prevention of ventilator-associated pneumonia in intensive care unit patients: a randomized controlled trial. Iran J Nurs Midwifery Res. 2018; 23:486–90.
Article15. Sutiono AB, Arifin MZ, Adhipratama H, Hermanto Y. The utilization of APACHE II score to predict the incidence of ventilator-associated pneumonia in patients with severe traumatic brain injury: a single-center study. Interdiscip Neurosurg. 2022; 28:101457.16. Nakahashi S, Imai H, Imanaka H, Ohshimo S, Satou T, Shima M, et al. Ventilator-associated events: prevalence and mortality in Japan. J Thorac Dis. 2018; 10:6942–9.
Article17. Alipour N, Toulabi T, Manouchehrian N, Anbari K, Rahimi Bashar F. A comparison of the effect of open and close endotracheal suctioning on the hemodynamic status of patient with head trauma hospitalized in the intensive care unit. Evid Based Care. 2014; 3:65–74.18. Ebrahimi Fakhar H, Rezaei K, Kohestani HR. Effect of closed endotracheal suction on incidence of ventilator-associated pneumonia. Sci J Kurdistan Univ Med Sci. 2010; 15:79–87.19. Hamishekar H, Shadvar K, Taghizadeh M, Golzari SE, Mojtahedzadeh M, Soleimanpour H, et al. Ventilator-associated pneumonia in patients admitted to intensive care units, using open or closed endotracheal suctioning. Anesth Pain Med. 2014; 4:e21649.
Article20. Qi L, Guo X, Nie C, Lv X, Zhang M. Research on effects of oropharyngeal aspiration on incidence of ventilator-associated pneumonia in patients with cerebral hemorrhage in ICU. J Healthc Eng. 2022; 2022:6433666.
Article21. Klompas M. Potential strategies to prevent ventilator-associated events. Am J Respir Crit Care Med. 2015; 192:1420–30.
Article22. Gershonovitch R, Yarom N, Findler M. Preventing ventilator-associated pneumonia in intensive care unit by improved oral care: a review of randomized control trials. SN Compr Clin Med. 2020; 2:727–33.
Article23. Klein Klouwenberg PM, van Mourik MS, Ong DS, Horn J, Schultz MJ, Cremer OL, et al. Electronic implementation of a novel surveillance paradigm for ventilator-associated events: feasibility and validation. Am J Respir Crit Care Med. 2014; 189:947–55.
Article24. Bouadma L, Sonneville R, Garrouste-Orgeas M, Darmon M, Souweine B, Voiriot G, et al. Ventilator-associated events: prevalence, outcome, and relationship with ventilator-associated pneumonia. Crit Care Med. 2015; 43:1798–806.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Monitoring and Interpretation of Mechanical Ventilator Waveform in the Neuro-Intensive Care Unit
- Multicenter Prospective Observational Study about the Usage Patterns of Sedatives, Analgesics and Neuromuscular Blocking Agents in the Patients Requiring More Than 72 Hours Mechanical Ventilation in Intensive Care Units of Korea
- Patient-Ventilator Dyssynchrony
- Home Mechanical Ventilation of Pediatric Patients
- Prevention and Management of Ventilator-Associated Pneumonia