J Neurocrit Care.
2018 Dec;11(2):63-70. 10.18700/jnc.180069.
Monitoring and Interpretation of Mechanical Ventilator Waveform in the Neuro-Intensive Care Unit
- Affiliations
-
- 1Department of Critical Care Medicine, Ewha Womans University Mokdong Hospital, Seoul, Korea. jinegero@hotmail.com
- 2Department of Neurology, Ewha Womans University Mokdong Hospital, Seoul, Korea.
- KMID: 2434831
- DOI: http://doi.org/10.18700/jnc.180069
Abstract
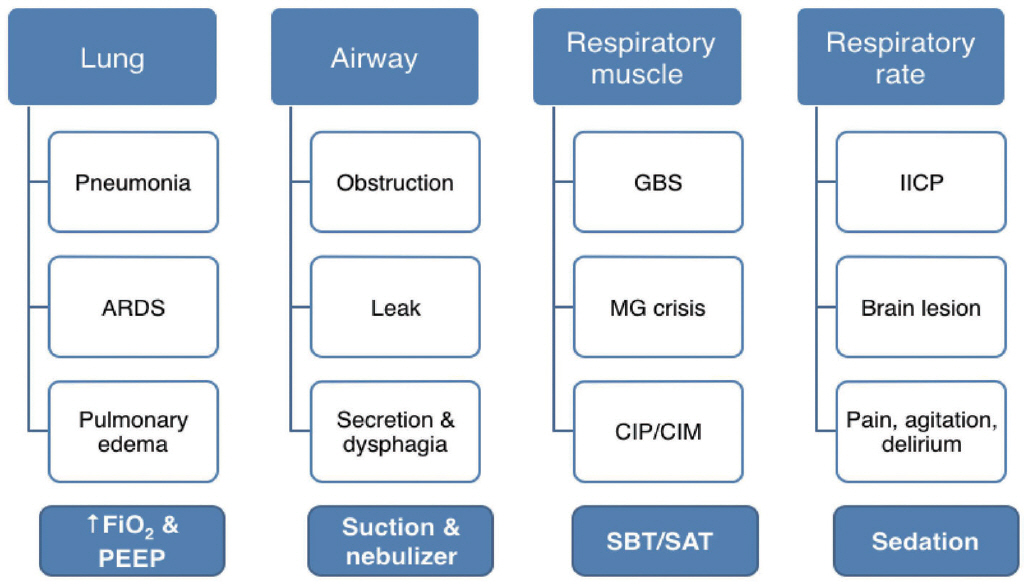
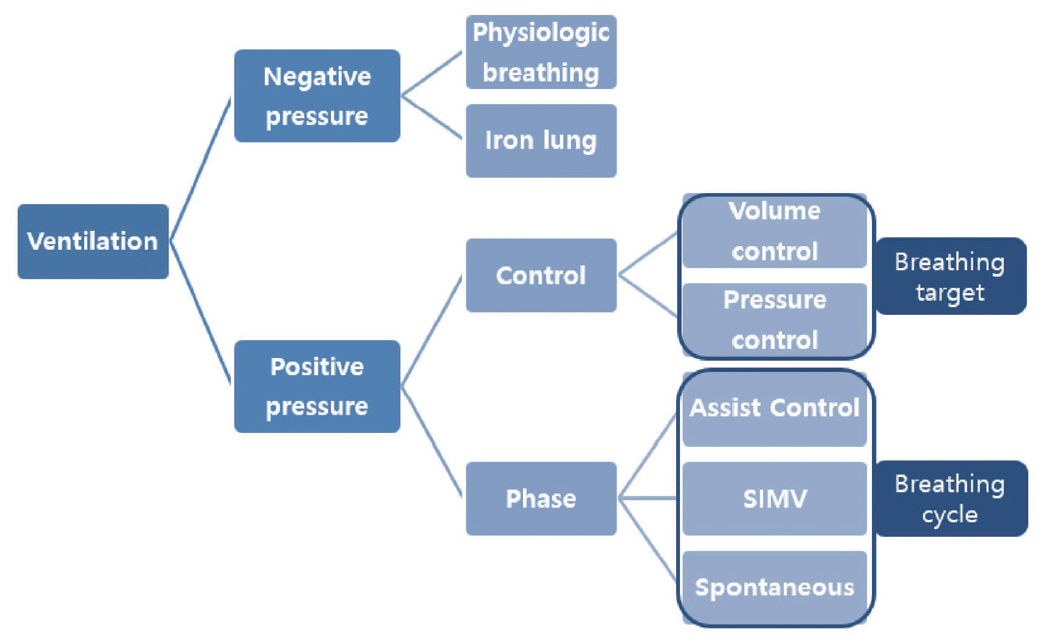
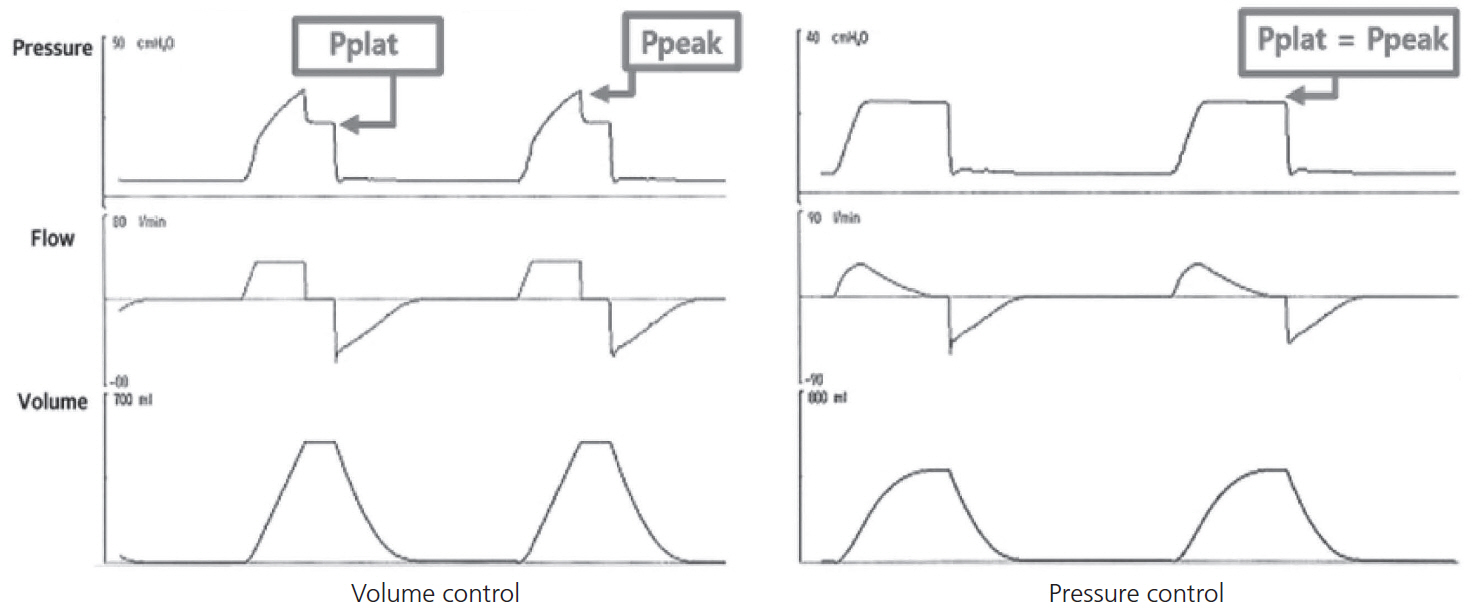
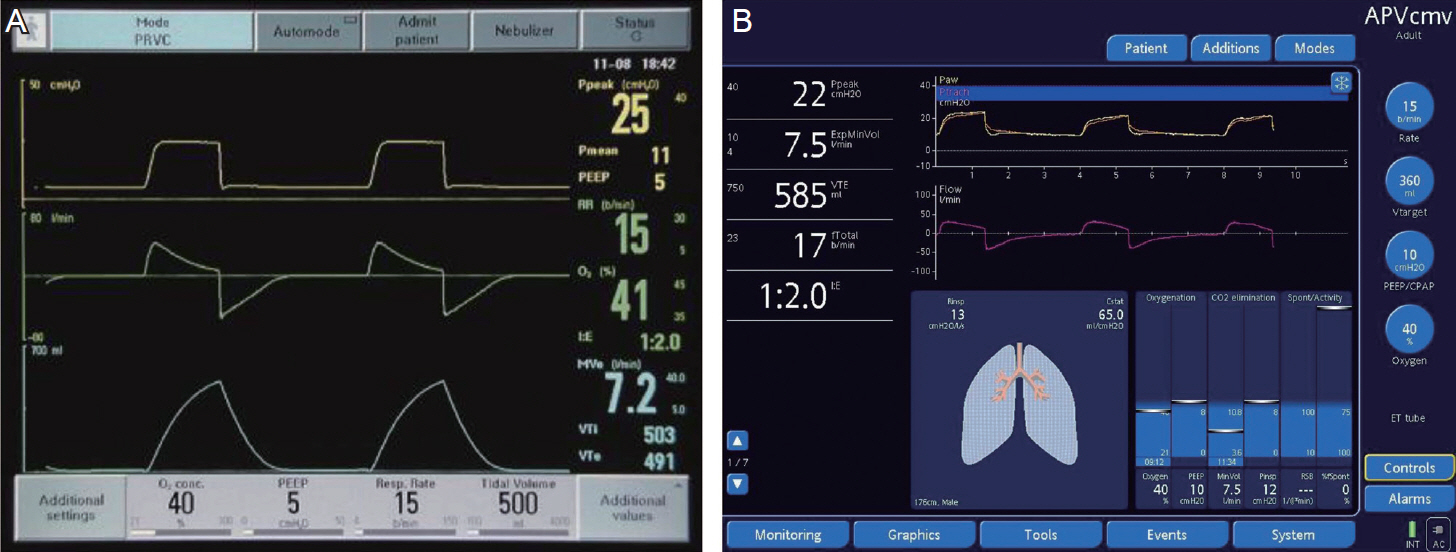
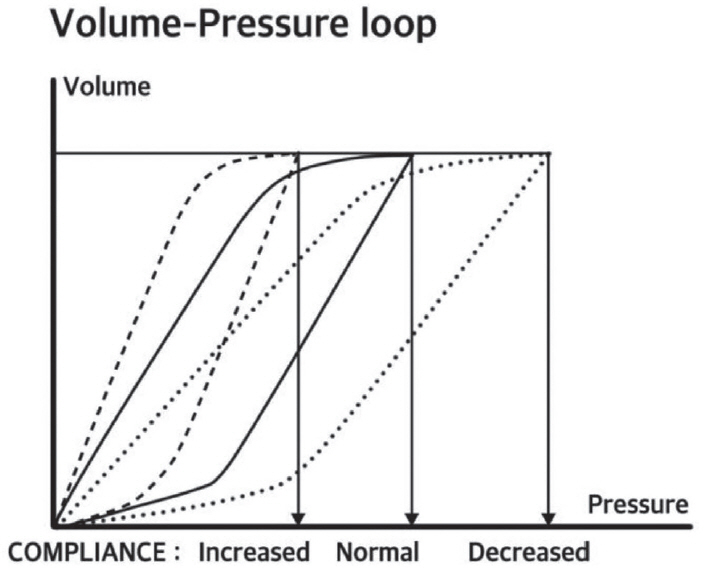
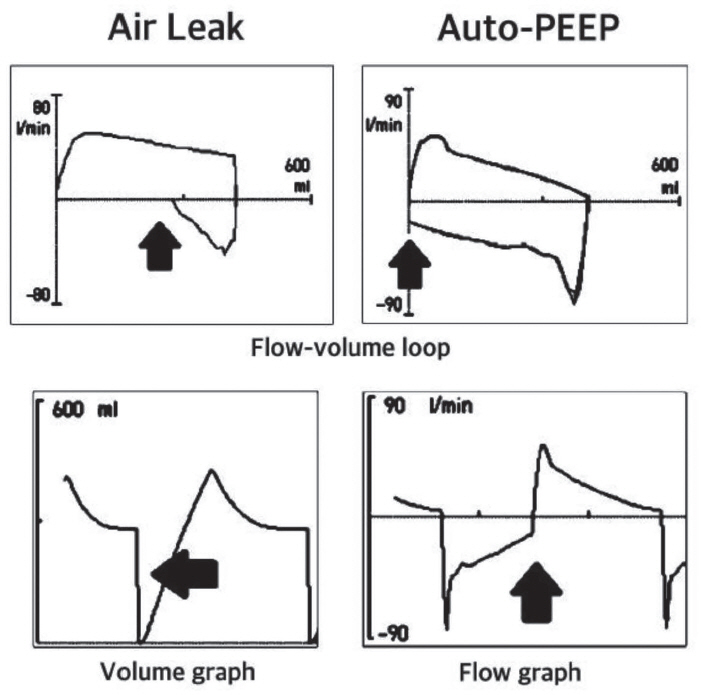
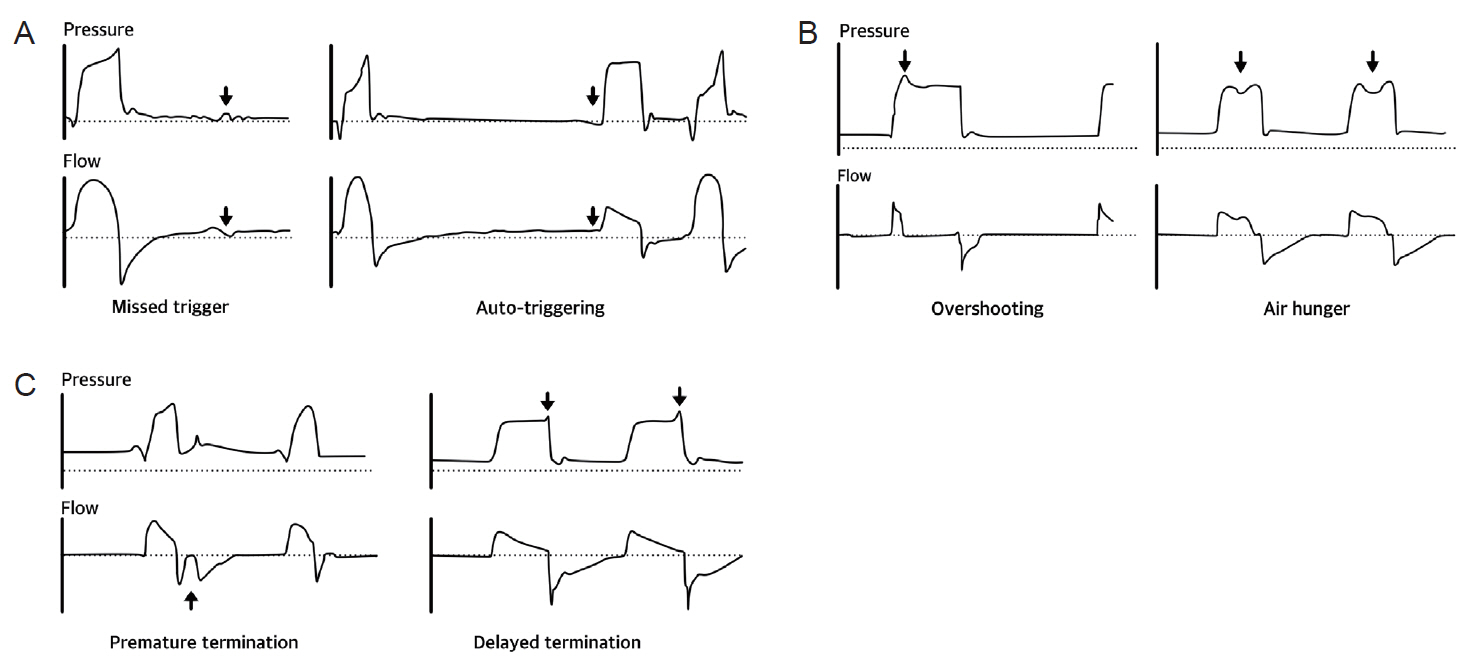
- Management of mechanical ventilation is essential for patients with neuro-critical illnesses who may also have impairment of airways, lungs, respiratory muscles, and respiratory drive. However, balancing the approach to mechanical ventilation in the intensive care unit (ICU) with the need to prevent additional lung and brain injury, is challenging to intensivists. Lung protective ventilation strategies should be modified and applied to neuro-critically ill patients to maintain normocapnia and proper positive end expiratory pressure in the setting of neurological closed monitoring. Understanding the various parameters and graphic waveforms of the mechanical ventilator can provide information about the respiratory target, including appropriate tidal volume, airway pressure, and synchrony between patient and ventilator, especially in patients with neurological dysfunction due to irregularity of spontaneous respiration. Several types of asynchrony occur during mechanical ventilation, including trigger, flow, and termination asynchrony. This review aims to present the basic interpretation of mechanical ventilator waveforms and utilization of waveforms in various clinical situations in the neuro-ICU.
Keyword
MeSH Terms
Figure
Reference
-
1. Holland MC, Mackersie RC, Morabito D, Campbell AR, Kivett VA, Patel R, et al. The development of acute lung injury is associated with worse neurologic outcome in patients with severe traumatic brain injury. J Trauma. 2003; 55:106–11.
Article2. Bratton SL, Davis RL. Acute lung injury in isolated traumatic brain injury. Neurosurgery. 1997; 40:707–12.
Article3. Amato MB, Barbas CS, Medeiros DM, Magaldi RB, Schettino GP, Loraenzi-Filho G, et al. Effect of a protective-ventilation strategy on mortality in the acute respiratory distress syndrome. N Engl J Med. 1998; 338:347–54.
Article4. Acute Respiratory Distress Syndrome Network, Brower RG, Matthay MA, Morris A, Schoenfeld D, Thompson BT, et al. Ventilation with lower tidal volumes as compared with traditional tidal volumes for acute lung injury and the acute respiratory distress syndrome. N Engl J Med. 2000; 342:1301–8.
Article5. Determann RM, Royakkers A, Wolthuis EK, Vlaar AP, Choi G, Paulus F, et al. Ventilation with lower tidal volumes as compared with conventional tidal volumes for patients without acute lung injury: a preventive randomized controlled trial. Crit Care. 2010; 14:R1.
Article6. Wolthuis EK, Choi G, Dessing MC, Bresser P, Lutter R, Dzoljic M, et al. Mechanical ventilation with lower tidal volumes and positive end-expiratory pressure prevents pulmonary inflammation in patients without preexisting lung injury. Anesthesiology. 2008; 108:46–54.
Article7. Pinheiro de Oliveira R, Hetzel MP, dos Anjos Silva M, Dallegrave D, Friedman G. Mechanical ventilation with high tidal volume induces inflammation in patients without lung disease. Crit Care. 2010; 14:R39.
Article8. Brower RG, Lanken PN, MacIntyre N, Matthay MA, Morris A, Ancukiewicz M, et al. Higher versus lower positive end-expiratory pressures in patients with the acute respiratory distress syndrome. N Engl J Med. 2004; 351:327–36.
Article9. Frost EA. Effects of positive end-expiratory pressure on intracranial pressure and compliance in brain-injured patients. J Neurosurg. 1977; 47:195–200.
Article10. McGuire G, Crossley D, Richards J, Wong D. Effects of varying levels of positive end-expiratory pressure on intracranial pressure and cerebral perfusion pressure. Crit Care Med. 1997; 25:1059–62.
Article11. Caricato A, Conti G, Della Corte F, Mancino A, Santilli F, Sandroni C, et al. Effects of PEEP on the intracranial system of patients with head injury and subarachnoid hemorrhage: the role of respiratory system compliance. J Trauma. 2005; 58:571–6.
Article12. The Korean Academy of Tuberculosis and Respiratory Diseases; Korean Society of Critical Care Medicine. Clinical practice guideline of acute respiratory distress syndrome. Seoul: MEDrang;2016.13. Jung JH. Brain and lung: lung injury in patients with brain injury. J Neurocrit Care. 2017; 10:1–6.
Article14. Amato MB, Meade MO, Slutsky AS, Brochard L, Costa EL, Schoenfeld DA, et al. Driving pressure and survival in the acute respiratory distress syndrome. N Engl J Med. 2015; 372:747–55.
Article15. Mascia L, Grasso S, Fiore T, Bruno F, Berardino M, Ducati A. Cerebro-pulmonary interactions during the application of low levels of positive end-expiratory pressure. Intensive Care Med. 2005; 31:373–9.
Article16. Branson RD, Blakeman TC, Robinson BR. Asynchrony and dyspnea. Respir Care. 2013; 58:973–89.
Article17. Nguyen TN, Badjatia N, Malhotra A, Gibbons FK, Qureshi MM, Greenberg SA. Factors predicting extubation success in patients with Guillain-Barré syndrome. Neurocrit Care. 2006; 5:230–4.
Article18. Wu JY, Kuo PH, Fan PC, Wu HD, Shih FY, Yang PC. The role of non-invasive ventilation and factors predicting extubation outcome in myasthenic crisis. Neurocrit Care. 2009; 10:35–42.
Article19. Williamson CA, Sheehan KM, Tipirneni R, Roark CD, Pandey AS, Thompson BG, et al. The association between spontaneous hyperventilation, delayed cerebral ischemia, and poor neurological outcome in patients with subarachnoid hemorrhage. Neurocrit Care. 2015; 23:330–8.
Article20. Carrera E, Schmidt JM, Fernandez L, Kurtz P, Merkow M, Stuart M, et al. Spontaneous hyperventilation and brain tissue hypoxia in patients with severe brain injury. J Neurol Neurosurg Psychiatry. 2010; 81:793–7.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Cardiac Complications in Patients Admitted to the Neuro-Intensive Care Unit
- Effect of a Clinical Nursing Practice Guideline of Enteral Nutrition Care on the Duration of Mechanical Ventilator for Critically Ill Patients
- Patient-Ventilator Dyssynchrony
- Prevention and Management of Ventilator-Associated Pneumonia
- Home Mechanical Ventilation of Pediatric Patients