J Korean Med Sci.
2023 Dec;38(50):e386. 10.3346/jkms.2023.38.e386.
Significant Reduction in External Ventricular Drain-Related Infections After Introducing a Novel Bundle Protocol: A Before and After Trial
- Affiliations
-
- 1Department of Neurosurgery, Seoul St. Mary’s Hospital, College of Medicine, The Catholic University of Korea, Seoul, Korea
- 2Department of Critical Care Medicine, Seoul National University Hospital, Seoul, Korea
- 3Department of Neurosurgery, Seoul National University Hospital, Seoul, Korea
- 4Department of Neurosurgery, Incheon St. Mary’s Hospital, College of Medicine, The Catholic University of Korea, Incheon, Korea
- 5Center for Infection Control and Prevention, Seoul National University Hospital, Seoul, Korea
- 6Department of Nursing, Seoul National University Hospital, Seoul, Korea
- 7Department of Nursing, Seoul Metropolitan Government-Seoul National University Boramae Medical Center, Seoul, Korea
- 8Department of Internal Medicine, Seoul National University College of Medicine, Seoul, Korea
- KMID: 2549956
- DOI: http://doi.org/10.3346/jkms.2023.38.e386
Abstract
- Background
External ventricular drain (EVD)-related infection (ERI) is a serious complication in neurosurgical patients. The estimated ERI rates range from 5 to 20 cases per 1,000 EVD catheter days. The pathophysiology of ERI is similar to central line-associated bloodstream infections (CLABSIs) stemming from skin-derived bacterial colonization. The use of bundle management can reduce CLABSI rates. Due to the pathogenic similarities between infections related to the two devices, we developed and evaluated the effectiveness of an ERI-bundle protocol based on CLABSI bundles.
Methods
From November 2016 to November 2021, we conducted a study to evaluate the effectiveness of an ERI-bundle protocol. This study adopted a before-and-after trial, comparing the ERI rates for the 2 years before and 3 years after the introduction of the newly developed ERI-bundle protocol. We also analyzed the contributing factors to ERI using logistic regression analysis.
Results
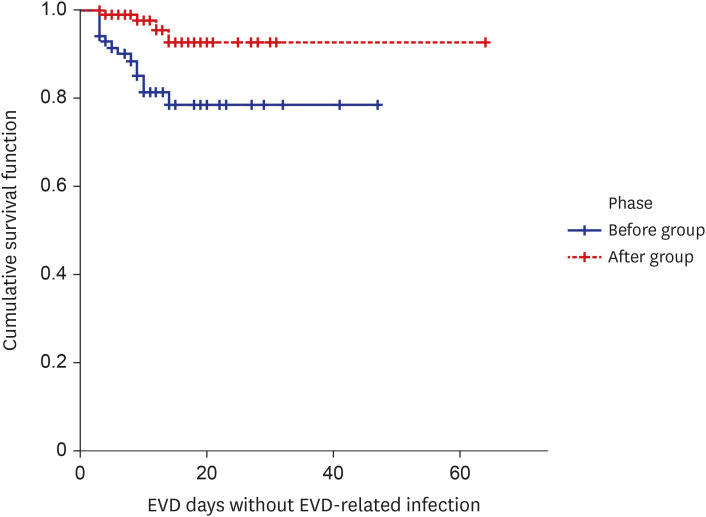
A total of 183 patients with 2,381 days of catheter use were analyzed. The ERI rate decreased significantly after the ERI-bundle protocol from 16.7% (14 of 84; 14.35 per 1,000 catheter days) to 4.0% (4 of 99; 3.21 per 1,000 catheter days) (P = 0.004).
Conclusion
Introduction of the ERI-bundle protocol was very effective in reducing ERI.
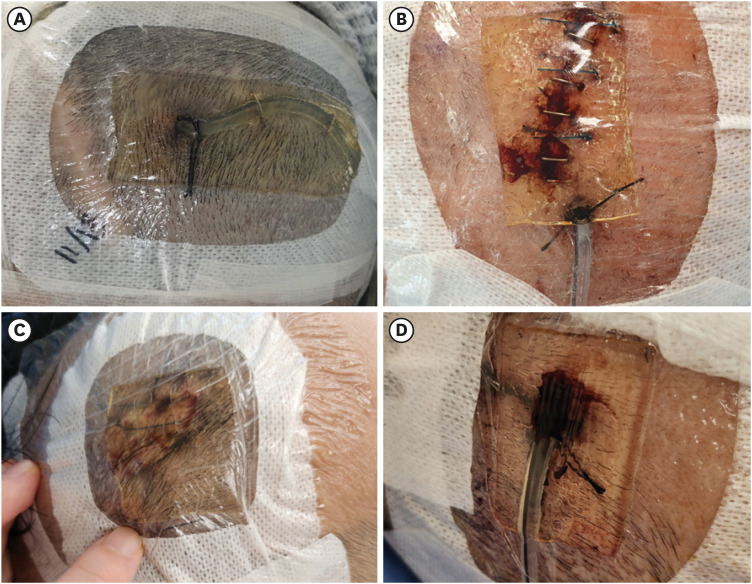
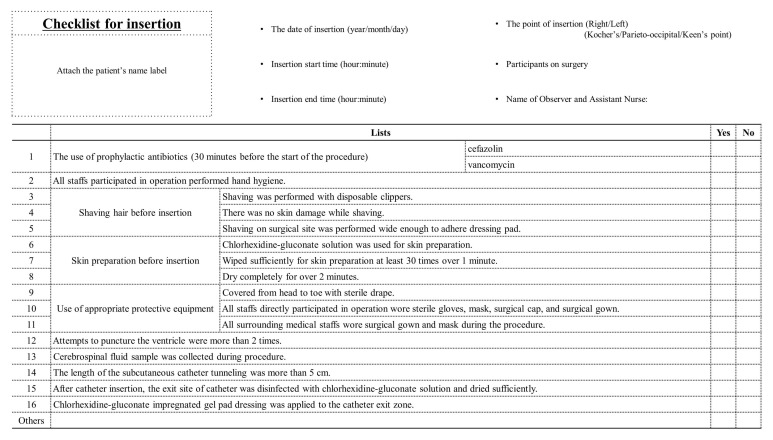
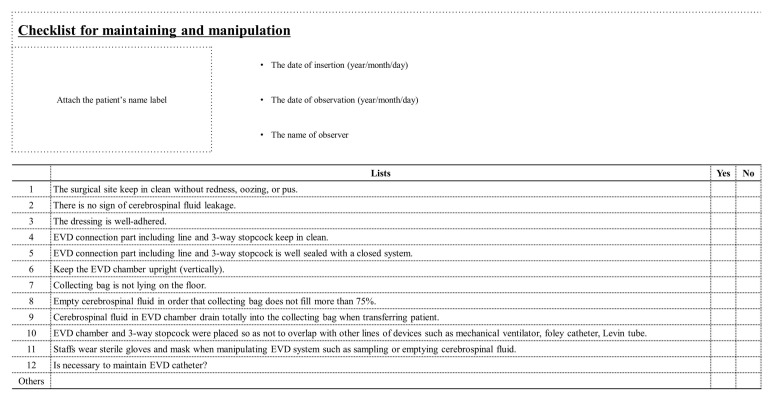
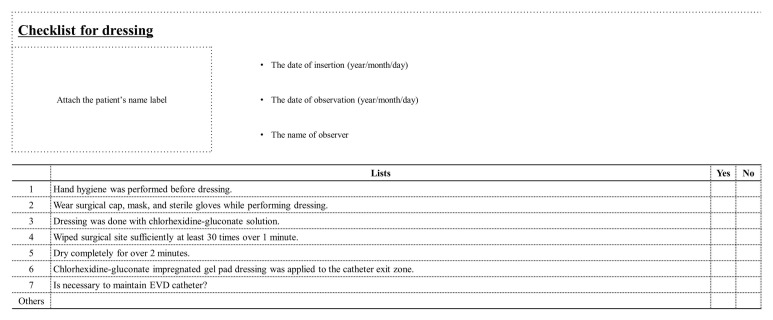
Figure
Reference
-
1. Timsit JF, Schwebel C, Bouadma L, Geffroy A, Garrouste-Orgeas M, Pease S, et al. Chlorhexidine-impregnated sponges and less frequent dressing changes for prevention of catheter-related infections in critically ill adults: a randomized controlled trial. JAMA. 2009; 301(12):1231–1241. PMID: 19318651.2. Scheithauer S, Bürgel U, Bickenbach J, Häfner H, Haase G, Waitschies B, et al. External ventricular and lumbar drainage-associated meningoventriculitis: prospective analysis of time-dependent infection rates and risk factor analysis. Infection. 2010; 38(3):205–209. PMID: 20333433.3. Babu MA, Patel R, Marsh WR, Wijdicks EF. Strategies to decrease the risk of ventricular catheter infections: a review of the evidence. Neurocrit Care. 2012; 16(1):194–202. PMID: 22045248.4. Ramanan M, Lipman J, Shorr A, Shankar A. A meta-analysis of ventriculostomy-associated cerebrospinal fluid infections. BMC Infect Dis. 2015; 15(1):3. PMID: 25567583.5. Jamjoom AAB, Joannides AJ, Poon MT, Chari A, Zaben M, Abdulla MAH, et al. Prospective, multicentre study of external ventricular drainage-related infections in the UK and Ireland. J Neurol Neurosurg Psychiatry. 2018; 89(2):120–126. PMID: 29070645.6. Arabi Y, Memish ZA, Balkhy HH, Francis C, Ferayan A, Al Shimemeri A, et al. Ventriculostomy-associated infections: incidence and risk factors. Am J Infect Control. 2005; 33(3):137–143. PMID: 15798667.7. Hoefnagel D, Dammers R, Ter Laak-Poort MP, Avezaat CJ. Risk factors for infections related to external ventricular drainage. Acta Neurochir (Wien). 2008; 150(3):209–214. PMID: 18278575.8. Maki DG, Stolz SM, Wheeler S, Mermel LA. Prevention of central venous catheter-related bloodstream infection by use of an antiseptic-impregnated catheter. A randomized, controlled trial. Ann Intern Med. 1997; 127(4):257–266. PMID: 9265424.9. Fellner A, Goldstein L, Lotan I, Keret O, Steiner I. Meningitis without meningeal irritation signs: What are the alerting clinical markers? J Neurol Sci. 2020; 410:116663. PMID: 31951834.10. Tracy A, Waterfield T. How to use clinical signs of meningitis. Arch Dis Child Educ Pract Ed. 2020; 105(1):46–49. PMID: 30692129.11. Horan TC, Andrus M, Dudeck MA. CDC/NHSN surveillance definition of health care-associated infection and criteria for specific types of infections in the acute care setting. Am J Infect Control. 2008; 36(5):309–332. PMID: 18538699.12. Flint AC, Toossi S, Chan SL, Rao VA, Sheridan W. A simple infection control protocol durably reduces external ventricular drain infections to near-zero levels. World Neurosurg. 2017; 99:518–523. PMID: 28012890.13. Flint AC, Rao VA, Renda NC, Faigeles BS, Lasman TE, Sheridan W. A simple protocol to prevent external ventricular drain infections. Neurosurgery. 2013; 72(6):993–999. PMID: 23467249.14. Pronovost P, Needham D, Berenholtz S, Sinopoli D, Chu H, Cosgrove S, et al. An intervention to decrease catheter-related bloodstream infections in the ICU. N Engl J Med. 2006; 355(26):2725–2732. PMID: 17192537.15. Pronovost P. Interventions to decrease catheter-related bloodstream infections in the ICU: the Keystone Intensive Care Unit Project. Am J Infect Control. 2008; 36(10):171.e1–171.e5.16. Pronovost PJ, Goeschel CA, Colantuoni E, Watson S, Lubomski LH, Berenholtz SM, et al. Sustaining reductions in catheter related bloodstream infections in Michigan intensive care units: observational study. BMJ. 2010; 340:c309. PMID: 20133365.17. Álvarez-Moreno CA, Valderrama-Beltrán SL, Rosenthal VD, Mojica-Carreño BE, Valderrama-Márquez IA, Matta-Cortés L, et al. Multicenter study in Colombia: Impact of a multidimensional International Nosocomial Infection Control Consortium (INICC) approach on central line-associated bloodstream infection rates. Am J Infect Control. 2016; 44(11):e235–e241. PMID: 27317408.18. Selby LM, Rupp ME, Cawcutt KA. Prevention of central-line associated bloodstream infections: 2021 update. Infect Dis Clin North Am. 2021; 35(4):841–856. PMID: 34752222.19. Mounier R, Lobo D, Cook F, Martin M, Attias A, Aït-Mamar B, et al. From the skin to the brain: pathophysiology of colonization and infection of external ventricular drain, a prospective observational study. PLoS One. 2015; 10(11):e0142320. PMID: 26555597.20. Darouiche RO, Wall MJ Jr, Itani KM, Otterson MF, Webb AL, Carrick MM, et al. Chlorhexidine-alcohol versus povidone-iodine for surgical-site antisepsis. N Engl J Med. 2010; 362(1):18–26. PMID: 20054046.21. Mimoz O, Lucet JC, Kerforne T, Pascal J, Souweine B, Goudet V, et al. Skin antisepsis with chlorhexidine-alcohol versus povidone iodine-alcohol, with and without skin scrubbing, for prevention of intravascular-catheter-related infection (CLEAN): an open-label, multicentre, randomised, controlled, two-by-two factorial trial. Lancet. 2015; 386(10008):2069–2077. PMID: 26388532.22. Zhou YJ, Wu JN, Chen LJ, Zhao HY. Comparison of infection rate with tunneled vs standard external ventricular drainage: a prospective, randomized controlled trial. Clin Neurol Neurosurg. 2019; 184:105416. PMID: 31319234.23. Garg K, Verma SK, Singh PK, Singh M, Chandra PS, Kale SS. Effect of external ventricular drain tunnel length on cerebrospinal fluid infection rates-a Bayesian network meta-analysis. World Neurosurg. 2022; 158:268–278.e4. PMID: 34774808.24. Mikhaylov Y, Wilson TJ, Rajajee V, Thompson BG, Maher CO, Sullivan SE, et al. Efficacy of antibiotic-impregnated external ventricular drains in reducing ventriculostomy-associated infections. J Clin Neurosci. 2014; 21(5):765–768. PMID: 24411330.25. Alleyne CH Jr, Hassan M, Zabramski JM. The efficacy and cost of prophylactic and perioprocedural antibiotics in patients with external ventricular drains. Neurosurgery. 2000; 47(5):1124–1127. PMID: 11063105.26. Ratilal B, Costa J, Sampaio C. Antibiotic prophylaxis for surgical introduction of intracranial ventricular shunts: a systematic review. J Neurosurg Pediatr. 2008; 1(1):48–56. PMID: 18352803.27. Dorresteijn KR, Brouwer MC, Jellema K, van de Beek D. Bacterial external ventricular catheter-associated infection. Expert Rev Anti Infect Ther. 2020; 18(3):219–229. PMID: 31994951.28. Walton MN, Hamilton LA, Kennedy SJ, Veve MP, Rowe AS. Antibiotic prophylaxis and incidence of infection with external ventricular drains and intra-cranial pressure monitors. Surg Infect (Larchmt). 2022; 23(3):262–269. PMID: 35133886.29. Scheithauer S, Möller M, Höllig A, Marx G, Thoröe S, Lopez-Gonzalez L, et al. Are chlorhexidine-containing dressings safe for use with ventricular drainages? Infection. 2014; 42(3):545–548. PMID: 24515936.30. Talibi SS, Silva AH, Afshari FT, Hodson J, Roberts SA, Oppenheim B, et al. The implementation of an external ventricular drain care bundle to reduce infection rates. Br J Neurosurg. 2020; 34(2):181–186. PMID: 32046516.31. Wong GK, Poon WS, Wai S, Yu LM, Lyon D, Lam JM. Failure of regular external ventricular drain exchange to reduce cerebrospinal fluid infection: result of a randomised controlled trial. J Neurol Neurosurg Psychiatry. 2002; 73(6):759–761. PMID: 12438486.32. Park P, Garton HJ, Kocan MJ, Thompson BG. Risk of infection with prolonged ventricular catheterization. Neurosurgery. 2004; 55(3):594–599. PMID: 15335426.33. Tunkel AR, Hasbun R, Bhimraj A, Byers K, Kaplan SL, Scheld WM, et al. 2017 Infectious Diseases Society of America’s clinical practice guidelines for healthcare-associated ventriculitis and meningitis. Clin Infect Dis. 2017; 64(6):e34–e65. PMID: 28203777.34. Yaseen M, Al-Hameed F, Osman K, Al-Janadi M, Al-Shamrani M, Al-Saedi A, et al. A project to reduce the rate of central line associated bloodstream infection in ICU patients to a target of zero. BMJ Qual Improv Rep. 2016; 5(1):u212545.w4986.35. Gupta P, Thomas M, Patel A, George R, Mathews L, Alex S, et al. Bundle approach used to achieve zero central line-associated bloodstream infections in an adult coronary intensive care unit. BMJ Open Qual. 2021; 10(1):e001200.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Case of External Ventricular Drain-related Ventriculitis: Implementation of a Standardized Bundle to Prevent Infection
- Multiple Intracranial Calcifications as a Complication of External Ventricular Drain Placement
- Rapid versus gradual external ventricular drain weaning: a general review of best practices
- Sphingomonas Paucimobilis: A Rare Infectious Agent Found in Cerebrospinal Fluid
- Device for Catheter Placement of External Ventricular Drain