Pediatr Emerg Med J.
2024 Jan;11(1):39-47. 10.22470/pemj.2023.00871.
Change of utilization of emergency department in children after lifting mask mandates in a single center in Korea
- Affiliations
-
- 1Department of Emergency Medicine, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Republic of Korea
- 2Department of Pediatrics, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Republic of Korea
- KMID: 2549539
- DOI: http://doi.org/10.22470/pemj.2023.00871
Abstract
- Purpose
We aimed to investigate changes in visiting patterns after the lifting of mask mandates in a single pediatric emergency medical center in Seoul, Korea.
Methods
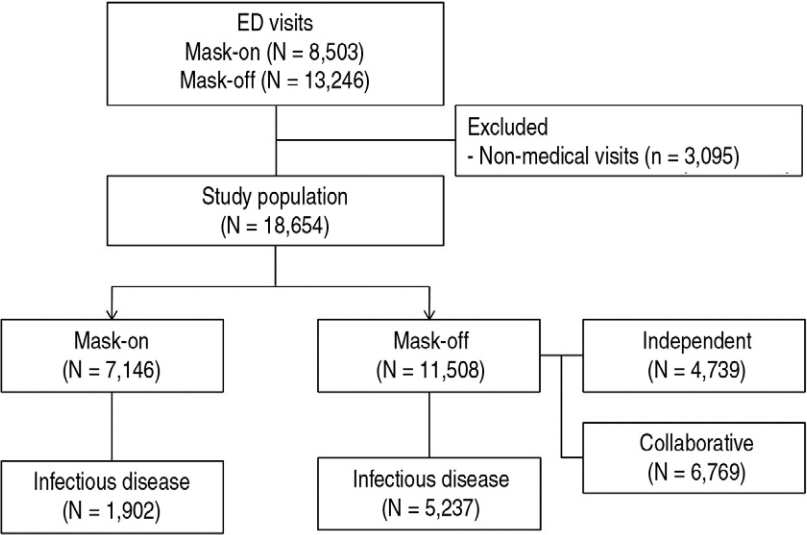
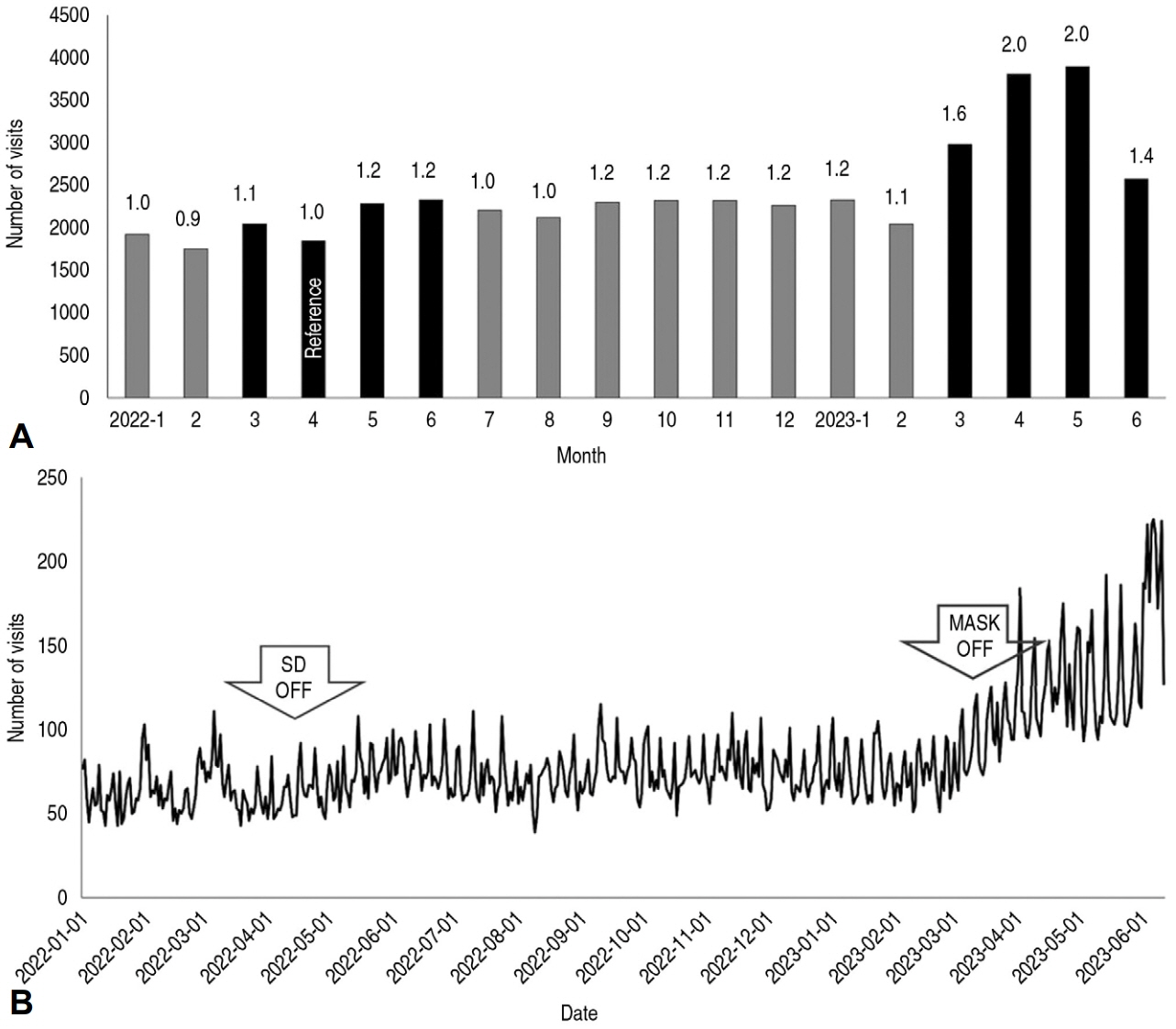
This retrospective study was based on the data of patients’ (≤ 18 years) visits to the emergency department (ED) of the center from January 1, 2022 through June 30, 2023. Clinical characteristics, Korean Triage and Acuity Scale (KTAS) level, ED outcomes, and length of stay were compared between before (March 20-June 30, 2022) and after (March 20-June 30, 2023) the lifting of mask mandates. The comparisons were iterated in the patients with infectious disease.
Results
During the study period, a total of 18,654 children visited the ED. After the lifting of mask mandates, ED visits increased from 7,146 to 11,508 (61.0%; 95% confidence interval, 59.5-62.6; P < 0.001). The increase was more prominent in the age of 2-5 years (82.9%), infectious diseases (175.3%), KTAS level 3 (127.7%), and length of stay shorter than 3 hours (78.8%-92.6%). The number of patients per hour increased by 151.2% for 5 patients or more and over 3,000% for 10 or more. Median length of stay decreased (2.3 hours [interquartile range, 1.2-4.1] to 1.9 hours [1.1-3.5]; P < 0.001). The patients with infectious disease (n = 7,139) showed similar patterns of increase in the age of 2-5 years, KTAS level 3, and length of stay shorter than 3 hours, with an additional increase in the age of 6-18 years.
Conclusion
After the lifting of mask mandates, pediatric visits increased by 61%, with the highest increase in children with mild infectious diseases on weekends and at night, and the proportion of more than 10 visits per hour significantly increased. We need urgent and realistic support measures from health authorities.
Keyword
Figure
Reference
-
References
1. Chaiyachati BH, Agawu A, Zorc JJ, Balamuth F. Trends in pediatric emergency department utilization after institution of coronavirus disease19 mandatory social distancing. J Pediatr. 2020; 226:274–277. e1.2. Jang KM, Ahn JY, Choi HJ, Lee S, Kim D, Lee DW, et al. Pediatric emergency department utilization and coronavirus disease in Daegu, Korea. J Korean Med Sci. 2021; 36:e11.3. Choi DH, Jung JY, Suh D, Choi JY, Lee SU, Choi YJ, et al. Impact of the COVID-19 outbreak on trends in emergency department utilization in children: a multicenter retrospective observational study in Seoul Metropolitan Area, Korea. J Korean Med Sci. 2021; 36:e44.4. Korea Disease Control and Prevention Agency (KDCA). Mask wearing to become mandatory [Internet]. KDCA; c2023 [cited 2023 Sep 20]. Available from : https://www.kdca.go.kr/board/board.es?mid=a30402000000&bid=0030&act=view&list_no=711162&tag=&nPage=1.5. Ministry of Health and Welfare (MOHW). Social distancing restrictions to be lifted starting April 18 [Internet]. MOHW; c2023 [cited 2023 Sep 20]. Available from : https://www.mohw.go.kr/board.es?mid=a20401000000&bid=0032&act=view&list_no=371146&tag=&nPage=16.6. Korea Disease Control and Prevention Agency (KDCA). From March 20 (Monday), the obligation to wear indoor masks on public transportation will be lifted [Internet]. KDCA; c2023 [cited 2023 Sep 20]. Korean. Available from: http://152.99.102.25/gallery.es?mid=a2040104010000&bid=0002&list_no=146055&act=view.7. Park SJ. Pediatric specialized emergency medical center, “zero realism”[Internet]. MEDICAL Observer; 2015 Mar 9 [cited 2023 Sep 20]. Korean. Available from: http://www.monews.co.kr/news/articleView.html?idxno=81203.8. The Korean Pediatric Society. Press release on the crisis in the healthcare system due to a shortage of pediatricians and primary care physicians. The Korean Pediatric Society; 2022 [cited 2023 Sep 20]. Korean. Available from: https://www.pediatrics.or.kr/general/notice/view.php?code=notice&category=&gubun=&page=1&number=12378&mode=view&keyfield=&key=.9. Williams K, Thomson D, Seto I, ContopoulosIoannidis DG, Ioannidis JP, Curtis S, et al. Standard 6: age groups for pediatric trials. Pediatrics. 2012; 129 Suppl 3:S153–60.10. Lim T, Park J, Je S. Pediatric Korean Triage and Acuity Scale. Pediatr Emerg Med J. 2015; 2:53–8. Korean.11. Kang DH. Coronavirus disease 2019 pandemic-related change in children’s visits to the emergency department. Pediatr Emerg Med J. 2022; 9:29–34. Korean.12. Lee SJ, Choi A, Ryoo HW, Pak YS, Kim HC, Kim JH. Changes in clinical characteristics among febrile patients visiting the emergency department before and after the COVID-19 outbreak. Yonsei Med J. 2021; 62:1136–44.13. Hwang SY, Lee JK, Ryu HS, Park SS, Choi JY, Lee HJ, et al. Long-term impact of coronavirus disease 2019 pandemic on emergency department utilization in a metropolitan emergency department in Korea. Pediatr Emerg Med J. 2021; 8:57–65. Korean.14. Comelli I, Scioscioli F, Cervellin G. Impact of the COVID-19 epidemic on census, organization and activity of a large urban emergency department. Acta Biomed. 2020; 91:45–9.15. Paek SH, Kim DK, Lee JH, Kwak YH. The impact of Middle East respiratory syndrome outbreak on trends in emergency department utilization patterns. J Korean Med Sci. 2017; 32:1576–80.16. Jang WM, Jang DH, Lee JY. Social distancing and transmission-reducing practices during the 2019 coronavirus disease and 2015 Middle East respiratory syndrome coronavirus outbreaks in Korea. J Korean Med Sci. 2020; 35:e220.17. Hartnett KP, Kite-Powell A, DeVies J, Coletta MA, Boehmer TK, Adjemian J, et al. Impact of the COVID-19 pandemic on emergency department visits - United States, January 1, 2019- May 30, 2020. MMWR Morb Mortal Wkly Rep. 2020; 69:699–704.18. Kim HB, Kim DK, Kwak YH, Shin SD, Song KJ, Lee SC, et al. Epidemiology of traumatic head injury in Korean children. J Korean Med Sci. 2012; 27:437–42.19. Kim MJ. Pediatric specialized emergency centers, disqualified due to not meeting the designation criteria, with about half losing their qualifications [Internet]. Medical Today; 2020 Nov 3 [cited 2023 Sep 20]. Korean. Avalable from: https://mdtoday.co.kr/news/view/179517237130897.20. Kim KE. The pediatric residency program has a capacity of 208 positions, but there are only one-fourth of the applicants [Internet]. Chosunilbo; 2023 Feb 7 [cited 2023 Sep 20]. Korean. Avalable from: https://www.chosun.com/national/welfaremedical/2023/02/07/LS2JT5OQCNC7JDE6LPH62POM34/.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Effect of Mask Mandates on the Intraocular Pressure Measured via Goldmann Applanation Tonometry
- Usefulness of transparent mask for communication in emergency room
- Utilization characteristics of an advanced pediatric emergency center: a single center study over 2 years
- Erratum to “Clinical utilization of four-factor prothrombin complex concentrate: a retrospective single center study”
- Association between face covering policies and the incidence of coronavirus disease 2019 in European countries